| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Review
Volume 16, Number 2, April 2025, pages 81-85
Five Years of Long COVID Syndrome: An Updated Review on Cardiometabolic and Psychiatric Aspects
Stefanos G. Sakellaropoulosa, b, k , Panagiotis G. Sakellaropoulosc, Benedict Schulte Steinbergd, Claire Rogerse, Omar Ismaelf, Eckart Wolfram Schollb, Muhemin Mohammedg, Andreas Mitsish, Nikoletta G. Patrinoui, j
aDepartment of Cardiology, University Hospital and University of Basel, Basel, Switzerland
bDepartment of Internal Medicine, Medical Center of Wurenlingen, Wurenlingen, Switzerland
cDepartment of Biopathology and Medical Biochemistry, Kalamata General Hospital, Kalamata, Greece
dDepartment of Cardiology and Internal Vascular Medicine, ALB FILS KLINIKUM GmbH, Goppingen, Germany
eDepartment of Cardiology and Angiology, SRH Health Center Bad Herrenalb, Bad Herrenalb, Germany
fDepartment of Cardiology and Internal Medicine, Klinikum Nordfriesland, Flensburg, Germany
gClinic of Internal Medicine, Hospital Affoltern, Affoltern, Switzerland
hCardiology Department, Nicosia General Hospital, Nicosia, Cyprus
iDepartment of Sociology, Panteion University of Social and Political Sciences, Athens, Greece
jDepartment of Psychology, Scientific College of Greece (SCG), Athens, Greece
kCorresponding Author: Stefanos G. Sakellaropoulos, Department of Cardiology, University Hospital and University of Basel, Basel, Switzerland
Manuscript submitted November 28, 2024, accepted January 9, 2025, published online February 6, 2025
Short title: LC on Cardiometabolic and Psychiatric Aspects
doi: https://doi.org/10.14740/cr2014
- Abstract
- Introduction
- Central and Peripheral Nervous System
- Dysautonomia
- Psychiatric Manifestations, Mitochondriopathy and Bipolar Disorder
- Myocardial Involvement
- The Role of Anemia and Vitamin D Deficiency in LC
- Aspects and the Potential Role of Medical Cannabis
- Conclusions
- References
| Abstract | ▴Top |
Five years after the outbreak of the coronavirus disease 2019 (COVID-19) pandemic, there is still a significant number of people who have survived COVID-19 but never fully recovered from the disease. They go through an odyssey of doctor visits and a multitude of diagnostic tests, which ultimately do not provide concrete correlations and answers to the question of how exactly long COVID (LC) affects both physical and mental health, and performance. Often, not even highly technical and highly specialized methods, such as cardiac magnetic resonance imaging (MRI), can provide further explanation. Various research efforts continue to investigate the causes, effects and possible treatments of LC, particularly its impact on cognition and mental health. Patients with LC may experience persistent symptoms, but new symptoms also occur. Based on available studies, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) does not only affect the pulmonary system, but nearly every major system and organ, from the brain and heart to the kidneys and immune system. What mechanisms could explain the persistent symptoms of LC and the inadequate recovery? How valuable is an early internal and neurological examination, particularly in the context of psychotherapy? In this review, we examined which factors could contribute to the persistence of LC symptoms and to what extent mitochondrial impairment by LC can explain the symptoms of LC.
Keywords: Long COVID; Mitochondria; Psychiatry; Myocardium
| Introduction | ▴Top |
Five years after the outbreak of the coronavirus disease 2019 (COVID-19) pandemic, there is still a significant number of people who have survived COVID-19 but never fully recovered from the disease. They go through an odyssey of doctor visits and a multitude of diagnostic tests that ultimately do not provide concrete correlations and answers to the question of how exactly long COVID (LC) disease affects both physical and mental health, and performance. Often, not even highly technical and highly specialized methods, such as cardiac magnetic resonance imaging (MRI), can provide further explanation. Various research efforts continue to investigate the causes, effects and possible treatments of LC, particularly its impact on cognition and mental health. Patients with LC may experience persistent symptoms, but new symptoms also occur. Based on available studies, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) does not only affect the pulmonary system, but nearly every major system and organ, from the brain and heart, to the kidneys and immune system [1].
In this review, we examined which factors could contribute to the persistence of LC symptoms and to what extent mitochondrial impairment by LC can explain the symptoms of LC.
| Central and Peripheral Nervous System | ▴Top |
As mentioned, the brain and nervous system are no exception; in fact, some of the most pervasive symptoms of LC appear to be neurological, cognitive or psychiatric in nature. The study by Taquet et al demonstrated that more than 2.5 million people experience neurological and psychiatric manifestations, such as psychotic disorders, cognitive deficit, dementia, and epilepsy or seizures, which may persist for years [2].
Patients with moderate disease, meaning they were hospitalized but not treated in an intensive care unit or required mechanical ventilation, showed cognitive deficits, and neuroimaging demonstrated altered patterns of connectivity in their brains [3].
| Dysautonomia | ▴Top |
Autonomic dysfunction is considered the main cause of neurocardiogenic abnormalities. This can lead to poor tissue perfusion, particularly in the brain and structures above the heart. This may result in orthostatic dysfunction (e.g., postural orthostatic tachycardia syndrome (POTS) or orthostatic hypotension) or syncope. Moreover, clinical manifestations are often associated with symptoms such as fatigue, exercise intolerance, lightheadedness, memory, and cognitive or sleep difficulties. Additionally, depression, anxiety and frequent headaches or migraines may also be common [4].
Brain fog associated with LC may involve mechanisms such as cardiac deconditioning, post-traumatic stress or dysautonomia [5]. The association between LC syndrome and brain fog may result from autonomic dysfunction, specifically sympathetic withdrawal (i.e., alpha-adrenergic dysfunction), which leads to orthostatic dysfunction [6].
| Psychiatric Manifestations, Mitochondriopathy and Bipolar Disorder | ▴Top |
Psychiatric manifestations are also common in COVID-19 survivors lasting more than 1 month. An Italian study found that 15% show evidence of depression, post-traumatic stress, anxiety, insomnia and obsessive-compulsive behavior [7].
It has been also observed that multiple psychiatric symptoms, resulting from encephalopathy and encephalitis, were noted in young adults [8].
Recent studies demonstrate that abnormally low fatty acid oxidation (FAO) and increased lactate production are causes of functional impairment. As glycolysis gradually increases during exercise, lactate is oxidized in the mitochondria for energy production, primarily in slow-twitch muscle fibers. Similar to FAO, lactate clearance capacity is an important marker of mitochondrial function. In post-COVID patients, muscular metabolic disturbances may be more severe than in active individuals or those with metabolic syndrome [9].
While lactate levels typically increase during high exercise intensity, elevated blood levels at lower exercise intensities indicate underlying mitochondrial dysfunction. Increased arterial lactate levels at relatively low exercise intensity (e.g., 0.9 mM at 150 W) suggest a premature transition from FAO to carbohydrate (CHO) oxidation, indicating metabolic reprogramming and dysfunctional mitochondria in LC syndrome, as illustrated in Figure 1 [9, 10].
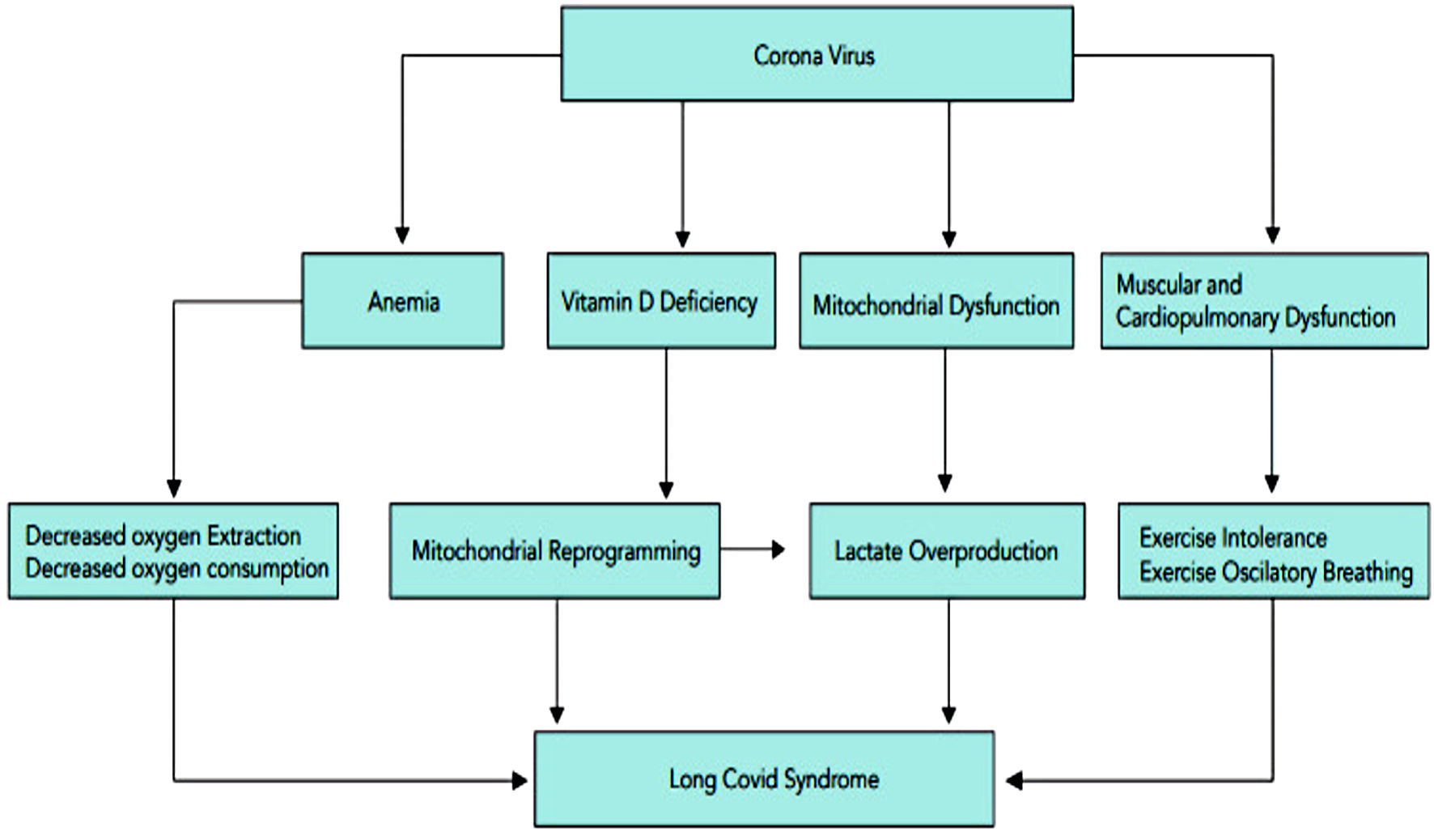 Click for large image | Figure 1. Proposed pathophysiology cascade of long COVID-19 syndrome, showcasing metabolic reprogramming and mitochondrial dysfunction. COVID-19: coronavirus disease 2019. |
Bipolar disorder (BD) is one of the major psychiatric diseases associated with impaired mitochondrial functions. Various lines of evidence have investigated this, with particular focus on dysregulation of energy metabolism, genetic predisposition, oxidative stress, cell death and apoptosis, dysregulated calcium homeostasis and electrophysiology. Currently, pharmacological interventions generally offer limited efficacy in preventing relapses or aiding recovery from mania or depressive episodes [10].
| Myocardial Involvement | ▴Top |
Myocardial involvement is typically suspected in cases of persistent (exertional) dyspnea, exercise intolerance, palpitations, and fatigue during or after SARS-CoV-2 infection. Although a psychosomatic etiology may be possible in these cases, myocardial involvement should be considered as a differential diagnosis and excluded first through a process of elimination.
Suitable methods for further investigation in suspected myocardial involvement include, in addition to the clinical presentation, a standard 12-lead electrocardiogram (ECG), transthoracic echocardiogram and Holter monitoring to exclude wall motion abnormalities, supraventricular or ventricular arrhythmias, electric disturbances, and to evaluate overall left ventricular function. In suspected non-COVID myocarditis, as well as in post-SARS-CoV-2 vaccination myocarditis, troponin levels are commonly used as a diagnostic tool to exclude myocardial injury. Cardiac MRI for diagnosis of myocarditis and/or pericarditis is a highly validated, noninvasive option and is a recognized alternative to endomyocardial biopsy for non-severe cases of post-vaccination myocarditis [11].
At the core of the already well-established pathomechanism underlying the initiation of SARS-CoV-2 myocarditis is the angiotensin receptor system.
Angiotensin-converting enzyme 2 (ACE2) is a multifunctional protein, with multiple functions including its primary role being the conversion of angiotensin II to angiotensin, and angiotensin I to angiotensin. In COVID-19 infection, ACE2 serves as the host receptor for SARS-CoV-2 entry into the myocardial cells, initiating infection and leading to myocarditis. Beyond the acute phase, the mechanisms of myocardial involvement and injury remain incompletely understood. A recent study by Blagova et al demonstrated that COVID-19 could lead to long-term severe post-COVID myoendocarditis, characterized by prolonged persistence of COVID-19 in cardiomyocytes, endothelium, and macrophages (up to 18 months), along with high immune activity [12]. Corticosteroids and anticoagulants should be considered as a treatment option in these cases of post-COVID myoendocarditis [12].
In line with this, Raman et al also suggest four major pathomechanisms of myocardial injury: direct viral toxicity, as promoted by the aforementioned invasion through the angiotensin receptor system; inflammatory response with extensive cytokine release, macrophage and T-lymphocyte involvement; thrombosis/vasculitis due to endothelial inflammation and dysfunction; neutrophil molecular defense mechanisms and immunothrombosis; and, finally, an autoimmune response, particularly through molecular mimicry and autoantibodies [13].
These four mechanisms lead to a wide range of cardiovascular implications, including viral, autoimmune, and inflammatory myocarditis, myocardial infarction, POTS or right ventricular injury [13]. The resulting long-term cardiovascular events, such as ventricular and supraventricular tachycardia, recurrent myocarditis, heart failure and thromboembolic events [13], highlight the critical importance of further investigation into the molecular pathomechanisms to establish cause-directed therapies and prevent long-term adverse events.
| The Role of Anemia and Vitamin D Deficiency in LC | ▴Top |
As far as we know, anemia impacts the severity of a SARS-CoV-2 infection. In a retrospective analysis of hospital records in the United Arab Emirates, ZainAlAbdin et al linked clinical laboratory data of COVID-19 patients to disease severity, intensive care unit admission and mortality rates [14].
Statistical analysis of data from over 3,000 patients revealed that anemia was associated with a statistically significant increased risk of severe COVID-19 outcomes, with intensive care unit admission being three times more likely in anemic patients than in those without anemia. Above all, ZainAlAbdin et al found that the overall mortality rate in anemic patients was 2.5 times higher than in non-anemic patients. Another retrospective analysis, which included an intensive care registry from over 6,000 patients across more than 370 international sites, examined the effect of hemoglobin levels on cardiac arrest and stroke in COVID-19 patients [15]. The study showed that moderate or severe anemia was associated with an increased risk of the aforementioned cardiovascular and cerebrovascular events. These results suggest that anemia may be both a significant predictor and a potential risk factor for the development of LC. However, it remains unclear to what extent reduced oxygen uptake or altered oxygen consumption due to anemia contributes, particularly in LC [15].
Another important factor that appears to influence the development of LC is vitamin D. Vitamin D, a steroid hormone, plays a key role in physiological metabolic processes and, according to the literature, also has protective effects against inflammation and oxidative stress [16]. For example, vitamin D has been shown to be beneficial for viral respiratory diseases. However, since the impact of vitamin D deficiency in patients suffering from COVID-19 remained unclear, Rachman et al [17] examined its effects on the clinical outcome of hospitalized COVID-19 patients in September 2023 as part of an Indonesian cohort study. They found that patients with vitamin D deficiency were significantly more likely to develop cardiovascular disease, experience more severe COVID-19 progression, and require mechanical respiratory support [17]. Another study examined the prevalence of vitamin D deficiency in patients with fatigue and neuropsychiatric symptoms of LC and found that while vitamin D insufficiency or deficiency was common, it was not significantly associated with fatigue or neuropsychiatric symptoms [18]. The lack of associations between vitamin D levels and fatigue, depression, anxiety, sleep problems or cognitive functions suggests that vitamin D deficiency may play a subordinate role in the disease process of LC. However, this may also be due to the small sample size (82 patients) or the limitations in the study methodology (e.g., inclusion criteria, study design, etc.). On the other hand, other studies have shown that vitamin D deficiency is associated with delayed recovery in LC [19] and that patients with vitamin D deficiency have more than threefold increased risk of experiencing a severe course of the disease [20]. Due to the divergent study results, larger-scale randomized controlled trials are needed to further investigate the role of vitamin D in COVID-19 patients.
Nevertheless, vitamin D deficiency appears to have numerous negative effects on disease progression, including LC and may be another, albeit subordinate, factor contributing to the pathogenesis of LC.
| Aspects and the Potential Role of Medical Cannabis | ▴Top |
Medical cannabis is considered a class of medicines [21]. Cannabis preparations include pharmaceutical formulations that may contain a broad spectrum of the bioactive chemical constituents of the cannabis plant. The plant produces various compounds, including cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC), terpenes, and flavonoids [22]. Cannabis acts on the endocannabinoid system, a complex neuromodulator system involved in multiple physiological functions throughout the body [23].
The potential role of cannabinoids as a treatment has been demonstrated in the context of acute COVID-19 infection, where cannabigerolic acid and cannabidiolic acid inhibited the entry of SARS-CoV-2 into epithelial cells in vitro [24].
Several studies demonstrate that COVID-19 survivors exhibit an increased 12-month risk of cardiovascular complications, such as cerebrovascular disorders, arrhythmias, heart failure and thromboembolic complications [25]. It is important to consider the potential adverse cardiovascular effects of medical cannabis in LC patients, as the composition of cannabis can influence adverse effects on the cardiovascular system [26]. While tachycardia and acute coronary events may be associated with cannabis use, they are more likely linked to the high THC content [26]. CBD has therapeutic potential in the context of cardiovascular diseases, including stroke, myocardial infarction, myocarditis, cardiomyopathies and cardiovascular complications of diabetes, due to its vasodilatory, antioxidant, anti-inflammatory and neuroprotective properties. Such properties could be particularly important as a potential treatment, considering its pathomechanism and pathophysiology of LC [27, 28]. Furthermore, the literature highlights that CBD has little to no effect on blood pressure and heart rate under physiological conditions [28].
| Conclusions | ▴Top |
To the best of our knowledge, there is currently no evidence-based examination suggested to diagnose or exclude LC. The perception of persistence of symptoms beyond 10 - 12 weeks justifies the existence of this condition.
Furthermore, there is no consensus on the treatment for patients with LC syndrome. Further investigation into its pathomechanism and pathophysiology could contribute to evaluating prognosis and treatment strategies.
Last but certainly not least, patients with psychiatric and/or psychosomatic issues in the era of LC, particularly those with a history of COVID-19 infection, should be further investigated metabolically, neurologically, and cardiologically rather than being treated solely as psychiatric cases.
Acknowledgments
None to declare.
Financial Disclosure
The authors did not receive support from any foundation, grant maker or donor.
Conflict of Interest
None to declare.
Author Contributions
Stefanos G. Sakellaropoulos contributed to the main text and article design, providing clinical expertise for clinical revision. Panagiotis G. Sakellaropoulos contributed to the section on infection. Benedict Schulte Steinberg contributed to the section on pathophysiology. Claire Rogers, Omar Ismael, Eckaart Wolfram Scholl, Muhemin Mohammed, and Andreas Mitsis contributed to the section on myocardial involvement. Nikoletta G. Patrinou contributed to the section on psychiatry and psychology.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
ACE2: angiotensin-converting enzyme 2; BD: bipolar disorder; CBD: cannabidiol; CHO: carbohydrate; ECG: electrocardiogram; FAO: fatty acid oxidation; LC: long COVID; MRI: magnetic resonance imaging; POTS: postural orthostatic tachycardia syndrome; THC: delta-9-tetrahydrocannabinol
| References | ▴Top |
- Bowe B, Xie Y, Al-Aly Z. Postacute sequelae of COVID-19 at 2 years. Nat Med. 2023;29(9):2347-2357.
doi pubmed - Taquet M, Sillett R, Zhu L, Mendel J, Camplisson I, Dercon Q, Harrison PJ. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. 2022;9(10):815-827.
doi pubmed - Voruz P, Allali G, Benzakour L, Nuber-Champier A, Thomasson M, Jacot de Alcantara I, Pierce J, et al. Long COVID neuropsychological deficits after severe, moderate, or mild infection. Clin Transl Neurosci. 2022;6:9.
doi - Colombo J, Arora RR, DePace NL, Vinik AI. Clinical autonomic dysfunction: measurement, indications, therapies, and outcomes. Springer Science + Business Media. New York, NY. 2014.
- Stremel RW, Convertino VA, Bernauer EM, Greenleaf JE. Cardiorespiratory deconditioning with static and dynamic leg exercise during bed rest. J Appl Physiol. 1976;41(6):905-909.
doi pubmed - Arora RR, Bulgarelli RJ, Ghosh-Dastidar S, Colombo J. Autonomic mechanisms and therapeutic implications of postural diabetic cardiovascular abnormalities. J Diabetes Sci Technol. 2008;2(4):645-657.
doi pubmed - Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, Melloni EMT, et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594-600.
doi pubmed - Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, Sultan M, et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7(10):875-882.
doi pubmed - Sakellaropoulos SG, Ali M, Papadis A, Mohammed M, Mitsis A, Zivzivadze Z. Is Long COVID syndrome a transient mitochondriopathy newly discovered: implications of CPET. Cardiol Res. 2022;13(5):264-267.
doi pubmed - Lam XJ, Xu B, Yeo PL, Cheah PS, Ling KH. Mitochondria dysfunction and bipolar disorder: From pathology to therapy. IBRO Neurosci Rep. 2023;14:407-418.
doi pubmed - Srivastava A, Nalroad Sundararaj S, Bhatia J, Singh Arya D. Understanding long COVID myocarditis: A comprehensive review. Cytokine. 2024;178:156584.
doi pubmed - Blagova O, Lutokhina Y, Kogan E, Savina P, Aleksandrova S, Zaklyazminskaya E. Post-COVID myocarditis in patients with primary cardiomyopathies: diagnosis, clinical course and outcomes. Genes (Basel). 2024;15(8):ehab724.1751.
doi pubmed - Raman B, Bluemke DA, Luscher TF, Neubauer S. Long COVID: post-acute sequelae of COVID-19 with a cardiovascular focus. Eur Heart J. 2022;43(11):1157-1172.
doi pubmed - ZainAlAbdin S, Aburuz S, Akour A, Beiram R, Alnajjar M, Abdel-Qader D, Arafat M, et al. Could anemia impact the severity of infections? COVID-19 as an example. F1000Res. 2024;13:295.
doi pubmed - Feng SN, Kelly TL, Fraser JF, Li Bassi G, Suen J, Zaaqoq A, Griffee MJ, et al. Impact of hemoglobin levels on composite cardiac arrest or stroke outcome in patients with respiratory failure due to COVID-19. Crit Care Explor. 2024;6(9):e1143.
doi pubmed - Matta Reddy A, Iqbal M, Chopra H, Urmi S, Junapudi S, Bibi S, Kumar Gupta S, et al. Pivotal role of vitamin D in mitochondrial health, cardiac function, and human reproduction. EXCLI J. 2022;21:967-990.
doi pubmed - Rachman A, Rahmaniyah R, Khomeini A, Iriani A. The association between vitamin D deficiency and the clinical outcomes of hospitalized COVID-19 patients. F1000Res. 2023;12:394.
doi pubmed - Charoenporn V, Charernboon T. Prevalence of vitamin D deficiency in patients with fatigue and neuropsychiatric symptoms of long COVID and its correlation with symptom severity. Curr Nutr Food Sci. 2025;21(4):501-507.
doi - Chen KY, Lin CK, Chen NH. Effects of vitamin D and zinc deficiency in acute and long COVID syndrome. J Trace Elem Med Biol. 2023;80:127278.
doi pubmed - Singhsakul A, Satirapoj B, Nimitphuwadon S, Rapeepattana S, Benjamanukul S, Traiyan S. Association of vitamin D level and severity of COVID-19 disease. J Southeast Asian Med Res [Internet]. 2024;8:e0202.
doi - Freeman TP, Hindocha C, Green SF, Bloomfield MAP. Medicinal use of cannabis based products and cannabinoids. BMJ. 2019;365:l1141.
doi pubmed - Goncalves J, Rosado T, Soares S, Simao AY, Caramelo D, Luis A, Fernandez N, et al. Cannabis and its secondary metabolites: their use as therapeutic drugs, toxicological aspects, and analytical determination. Medicines (Basel). 2019;6(1):31.
doi pubmed - Zou S, Kumar U. Cannabinoid receptors and the endocannabinoid system: signaling and function in the central nervous system. Int J Mol Sci. 2018;19(3):833.
doi pubmed - van Breemen RB, Muchiri RN, Bates TA, Weinstein JB, Leier HC, Farley S, Tafesse FG. Cannabinoids block cellular entry of SARS-CoV-2 and the emerging variants. J Nat Prod. 2022;85(1):176-184.
doi pubmed - Wang W, Wang CY, Wang SI, Wei JC. Long-term cardiovascular outcomes in COVID-19 survivors among non-vaccinated population: A retrospective cohort study from the TriNetX US collaborative networks. EClinicalMedicine. 2022;53:101619.
doi pubmed - Pacher P, Steffens S, Hasko G, Schindler TH, Kunos G. Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat Rev Cardiol. 2018;15(3):151-166.
doi pubmed - Stanley CP, Hind WH, O'Sullivan SE. Is the cardiovascular system a therapeutic target for cannabidiol? Br J Clin Pharmacol. 2013;75(2):313-322.
doi pubmed - Kicman A, Toczek M. The effects of cannabidiol, a non-intoxicating compound of cannabis, on the cardiovascular system in health and disease. Int J Mol Sci. 2020;21(18):6740.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.