| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Short Communication
Volume 16, Number 2, April 2025, pages 161-168
Long-Term Outcomes and Predictors of Recurrence in Atrial Arrhythmia Ablations Post-Fontan Procedure: A Retrospective Analysis
Khush M. Kharidiaa, Weiyi Tana, Nimesh S. Patela, b
aDepartment of Internal Medicine, University of Texas Southwestern Medical Center, Dallas, TX, USA
bCorresponding Author: Nimesh S. Patel, Department of Internal Medicine, University of Texas Southwestern Medical Center, Dallas, TX 75390-9030, USA
Manuscript submitted December 27, 2024, accepted February 14, 2025, published online February 25, 2025
Short title: Outcomes of SVT Ablation in Fontan
doi: https://doi.org/10.14740/cr2034
| Abstract | ▴Top |
Background: Supraventricular tachycardia (SVT) is common in patients who have undergone a Fontan procedure and is poorly tolerated. SVT recurrence rates after catheter ablations are high. Recent data on the outcomes of SVT ablation and the predictors of recurrence in this population are limited.
Methods: Electronic medical records of patients who had undergone a Fontan procedure and SVT ablation between January 1, 1995, and October 1, 2023, at a tertiary care center were reviewed. Demographic, clinical, and outcome variables over 5 years were compared between patients with and without SVT recurrence.
Results: Twenty-five patients (56% male, mean age 31.5 ± 7.2 years) with a mean age of 6.1 ± 3.6 years at Fontan surgery were included. Ablation success rate was 92%. Recurrence occurred in 12 (48%) patients, of whom 7 (28%) required repeat ablations. Thirteen (59%) patients had a cardiac hospitalization, and one patient died in the 5-year follow-up period. Atypical (71%) and typical (33%) right atrial flutter were the most common SVTs. Higher brain natriuretic peptide (BNP) levels pre- (1,702 vs. 242, P = 0.028) and post-ablation (862 vs. 112, P = 0.017) were associated with recurrence. Atriopulmonary (AP) Fontan type (91% vs. 17%, P = 0.0006), number of radiofrequency (RF) applications (48 vs. 14, P = 0.045), post-ablation cardiovascular (CV) hospitalizations (82% vs. 36% P = 0.030), and post-ablation antiarrhythmic prescriptions (1.8 vs. 1.2, P = 0.0256) were more prevalent in patients with recurrence.
Conclusion: Catheter ablation of SVT in patients with Fontan physiology is associated with a high success rate and a high long-term recurrence rate. Recurrence of SVT is associated with markers of severe heart disease and type of Fontan.
Keywords: Supraventricular arrhythmia; Fontan; Ablation; Outcomes; Recurrence
| Introduction | ▴Top |
Fontan and hemi-Fontan surgery offers a surgical solution for patients with a functional single ventricle, resulting in an 85-95% survival rate at 15 years post-procedure [1, 2]. Despite surgical advances like the total cavopulmonary connection and extra-cardiac (EC) or lateral tunnel (LT) conduits, the burden of atrial or supraventricular arrhythmias after Fontan palliation remains high [3-5]. Atrial arrhythmias are poorly tolerated in Fontan physiology, potentially leading to reduced cardiac output and increased risk of thromboembolic disease [6-8].
Electrophysiology (EP) catheter ablation has been shown to be more effective than antiarrhythmic drugs for managing atrial arrhythmias in patients with Fontan physiology. Multiple studies have confirmed lower arrhythmia burden after the procedure [9-11]. Nevertheless, recurrence rates after ablation are substantial [12-16].
EP studies in patients with Fontan physiology can be challenging due to their complex cardiac anatomies [7, 17]. Little is known about the outcomes of EP ablation in this population in recent years. Previous studies have established the safety of catheter ablation for atrial arrhythmias but have incompletely investigated long-term outcomes [15, 18]. Our study aims to 1) identify clinical characteristics of patients with a history of Fontan palliation surgery who have undergone EP ablations, 2) evaluate the long-term outcomes of ablation in these patients, and 3) determine factors that may influence the recurrence of atrial arrhythmias.
| Materials and Methods | ▴Top |
This study was deemed exempt from review by the University of Texas (UT) Southwestern Institutional Review Board.
Study population
We conducted a retrospective study of patients at the UT Southwestern Medical Center with history of Fontan or hemi-Fontan procedure and EP ablation for SVTs between January 1, 1995, and October 1, 2023. Patients with Current Procedural Terminology (CPT) diagnosis codes for Fontan/hemi-Fontan procedures and EP ablation of SVTs were included in the study. Chart review was subsequently performed to confirm eligibility and abstract baseline data. Patients who had SVT ablations prior to a Fontan procedure were excluded from the cohort.
Data collection
We conducted a detailed chart review to collect demographic information, congenital heart disease (CHD) diagnosis, laboratory results, cardiac medication history, electrocardiogram (EKG) findings, transthoracic echocardiogram (TTE) results, right heart catheterization (RHC) data, procedural details, and outcomes measures. Procedural variables, such as length of procedure, number of applications, and location of arrhythmia, were abstracted from procedure notes. Typical right atrial (RA) flutter was defined as macro-reentry around the tricuspid annulus dependent on the cavo-tricuspid isthmus. Atypical RA flutter was defined as any macro-reentrant circuit not dependent on the cavo-tricuspid isthmus and included intra-atrial re-entrant tachycardia. Atrial tachycardia (AT) was defined as automaticity or micro-reentry circuits from sites ectopic to the sinus node. Cardiac medications were defined as antiarrhythmics (class I-V), anti-hypertensives, heart failure medications, diuretics, and anticoagulants including aspirin, warfarin, P2Y12 inhibitors, and direct oral anticoagulants. For pre- and post-ablation variables, only the most recent data within 2 years of the index procedure were recorded.
Outcome measures
Outcome measures of importance included recurrence of arrhythmia after first ablation, repeat ablation, hospitalizations, and death at 5 years. Procedural success was determined by clinician documentation in the ablation procedure note. Recurrence of atrial arrhythmia was defined by documentation of recurrent tachycardia symptoms, EKG confirmation of SVT, or history of repeat atrial arrhythmia ablation. Recurrent arrythmias were classified as same or different based on EKG analysis upon recurrence or documentation of arrythmias during repeat ablation. Hospitalizations were identified through the electronic medical record system and were classified as cardiovascular (CV) or non-CV hospitalizations. CV hospitalizations were defined as admission to a medicine or cardiology service with cardiac chief complaint or cardiac primary problem in the initial history and physical documentation. The 5-year follow-up time point was selected to capture a clinically meaningful sample as has been done by Egbe et al, and recurrence rates before and after 2018 were analyzed given a lack of data in the literature on this subject since 2018 [9].
Statistical analysis
Descriptive statistics were used to analyze the variables for the overall cohort. Student’s t-tests, Fisher’s exact test, and two-sample proportions tests were employed to investigate differences between patients with and without recurrence, with a significance level set at α < 0.05.
| Results | ▴Top |
Twenty-six patients at UT Southwestern had a history of a Fontan procedure and SVT ablation. One patient with ablation before the Fontan procedure was excluded from the study. The 25 participants included had a total of 34 ablations; 12 (48%) had a documented recurrence within 5 years.
Demographics
The mean age (± SD) at Fontan surgery was 6.1 ± 3.6 years and the mean age at ablation procedure was 31.5 ± 7.2 years. Fourteen (56%) patients were male. The average body mass index (BMI) of the patients was 26.3 ± 4.7 kg/m2. The most common CHDs in the cohort were tricuspid atresia (TA, 40%) and transposition of great arteries (TGA, 35%). AP (48%) and fenestrated LT (36%) were the most common initial Fontan types (Table 1).
 Click to view | Table 1. Patient Demographic and Clinical Correlates in Patients With and Without Arrhythmia Recurrence |
Clinical covariates and predictors of recurrence
Forty-four percent of patients who had an ablation after 2018 and 55% of those who had an ablation before 2018 had recurrence (P = 0.6). Similarly, 42% of patients who had an ablation after 2020 and 54% of those who had one earlier had recurrence (P = 0.5). Of those with an AP approach, 10 (91%) had recurrence while of those with an LT approach, only 1 (11%) had recurrence (P = 0.0006 and P = 0.0094, respectively). Among the patients with AP Fontan procedure who had a recurrence, two had a revision to EC.
Patients with Fontan palliation undergoing SVT ablation were prescribed on average 4.00 cardiac medications before the ablation and 3.91 medications after their first post-procedural visit. Patients who later developed recurrence had significantly more anti-arrhythmic medications prescribed post-ablation than those without recurrence (1.8 vs. 1.2, P = 0.03). The most common post-ablation anti-arrhythmic medications prescribed were metoprolol (52%), digoxin (24%), sotalol (20%), and dofetilide (16%). There were no significant differences in the prescription patterns of these medications between patients with and without recurrence. Six (24%) patients had a history of prior implantable cardioverter defibrillator/pacemaker (ICD/PPM) and 11 (44%) had a history of prior cardioversion (Table 1).
Brain natriuretic peptide (BNP) levels decreased after ablation (1,054 to 524). Those with recurrence had higher BNP levels both before (1,702 vs. 242, P = 0.03) and after the ablation (862 vs. 112, P = 0.02). Thirteen (52%) patients had a history of heart failure and 10 of the 21 with echocardiography data had an ejection fraction (EF) < 50%, but neither metric was significantly different between those with and without recurrence (Table 1). Fourteen patients had RHC performed within 2 years of the EP ablation procedure. There was no significant difference in the RHC or TTE data between participants with and without recurrence (Supplementary Material 1, cr.elmerpub.com).
Procedural variables
Procedural data were obtained for 22 of the 25 patients. Three patients had procedures done at other facilities where detailed procedural notes were unavailable. The most common arrhythmias identified were atypical RA flutter (71%) and typical RA flutter (33%). One patient had left atrial flutter, two had focal ATs, and one had an atrioventricular nodal re-entrant tachycardia. There was no significant difference in procedure length, arrhythmia types, and arrhythmia location between the recurrent and nonrecurrent subgroups. Patients with recurrence had significantly more applications than those who did not (48 vs. 14, P = 0.045, Table 2). Six (23%) patients had documented transeptal puncture during the procedure, of which four had LT, one had EC, and one had AP that was revised to EC Fontan type.
 Click to view | Table 2. Procedural Correlates in Patients With and Without Arrhythmia Recurrence |
Outcomes
Medium follow-up period was 3.3 ± 3.7 years. Ablation was noted to be successful in 23 of the 25 cases (92%). Two patients had minor complications after the ablation, one with a groin hematoma and the other with mild post-discharge femoral bleeding which was managed conservatively. Of the 12 patients who experienced SVT recurrence, 10 (83%) had a different arrhythmia.
The mean time to recurrence was 1.4 ± 0.93 years. Two patients (8.0%) had a recurrence at 6 months and four (16.0%) had a recurrence by 1 year. Seven (28%) patients had a repeat ablation and the median time to repeat ablation was 2.70 years. One patient in the cohort died in the 5-year follow-up period.
Thirteen (59%) of the 22 patients with follow-up hospitalization data available had cardiac hospitalizations within 5 years, while seven (32%) had non-cardiac hospitalization. At 5 years, nine patients (82%) in the recurrence and four patients (36%) in the nonrecurrence groups had cardiac hospitalizations (Table 3, P = 0.030).
 Click to view | Table 3. Hospitalization Outcomes in Patients With and Without Arrhythmia Recurrence |
| Discussion | ▴Top |
Atrial arrhythmias are a significant concern in patients who have undergone Fontan palliation given their high prevalence and potential for adverse outcomes. Our study aimed to investigate long-term outcomes in Fontan patients undergoing EP ablation and determine factors that are associated with recurrence. We found that nearly half of the patients with SVT ablation after Fontan surgery had recurrence and over a quarter had repeat ablations at 5 years. We identified elevated BNP levels, more RF applications, and AP Fontan type to be associated with increased risk of arrhythmia recurrence.
Limited studies conducted prior to 2018 on this patient population have shown that freedom from atrial arrhythmia recurrence at 60 months was 41% and that 29% of patients underwent repeat ablation [9, 11]. This contemporary study mirrors these findings, revealing a freedom from recurrence at 60 months of 52% and a repeat ablation rate of 28%. A procedural success rate of 92% falls in the range of these past studies as well (83-94%). Consistent with prior studies, the risk of recurrence seems to increase with time. The similarities lend validity to our findings (despite the small sample size) and re-demonstrate that catheter ablation is safe and effective in managing SVT in this patient population.
This study found no significant difference in recurrence between ablations before and after 2018 or 2020, though there was notably a 10-15% reduction of recurrence in recent years. Although the small sample may have been insufficient to capture this difference, these results indicate that there has not been a major change in outcomes in recent years. Rates of hospitalization post-ablation are substantial, with a 5-year CV hospitalization rate of 59%. This was the first study to report that patients with recurrence were more likely to experience CV hospitalization post-ablation than those without. Whether arrhythmia recurrence contributes to CV hospitalization or is simply a consequence of severe underlying disease from deteriorating Fontan hemodynamics and atrial stress is unknown and requires further investigation.
It is known that AP Fontan type is associated with an increased risk of atrial arrhythmia [4]. This study expands on these findings by showing that an AP approach is also strongly associated with a much higher rate of recurrence after ablation than the LT approach. With 90% of those with an AP Fontan having recurrence of arrhythmias, upfront rhythm control with cardioversion or ablation, as well as earlier consideration of transplant workup may be clinically prudent in these patients.
BNP levels were associated with arrhythmia recurrence. The lower BNP levels post-ablation may indicate the effect of ablation on reducing the deleterious effects of arrhythmias on cardiac hemodynamics [19]. Patients with recurrence had significantly higher baseline BNP pre- and post-ablation, suggesting that BNP may be a predictor of outcomes in this population as it has shown to be in other atrial arrhythmias [20].
Patients with recurrence had more procedural applications during the ablation and were prescribed more antiarrhythmic medications post-ablation than those without recurrence. These findings complement prior studies demonstrating that ablating more circuits was associated with unfavorable outcomes, likely related to the presence of more complex arrhythmia substrate in general [9, 18]. The predictive factors noted here (BNP, antiarrhythmic medications, RF applications, etc.) may be helpful in identifying patients with more severe heart disease that may have a greater risk of arrhythmia recurrence.
While atypical flutters are generally associated with higher recurrence rates after ablation (7-53%) compared to typical flutter (11%), this study reveals a high recurrence rate in patients with typical (57%) and atypical flutter (53%) in this cohort [21]. This unexpected similarity in recurrence rates may be explained by the complex hemodynamic and atrial anatomy of patients with a Fontan as opposed to patients in the general population undergoing ablation (Figs. 1 and 2). Most patients in this cohort had 3D high density mapping performed during their EP study, especially in recent years, but a significant difference in recurrence rates with their use was not observed. While the use of these novel technologies has significantly aided ablation procedures by more accurately identifying and successfully ablating arrythmia foci with less fluoroscopy exposure, their impact on long-term outcomes remains unclear. Future studies should evaluate the long-term benefits of novel mapping and ablation techniques (including pulsed field ablation), exploring how they may impact outcomes in patients with a Fontan and atrial arrhythmias.
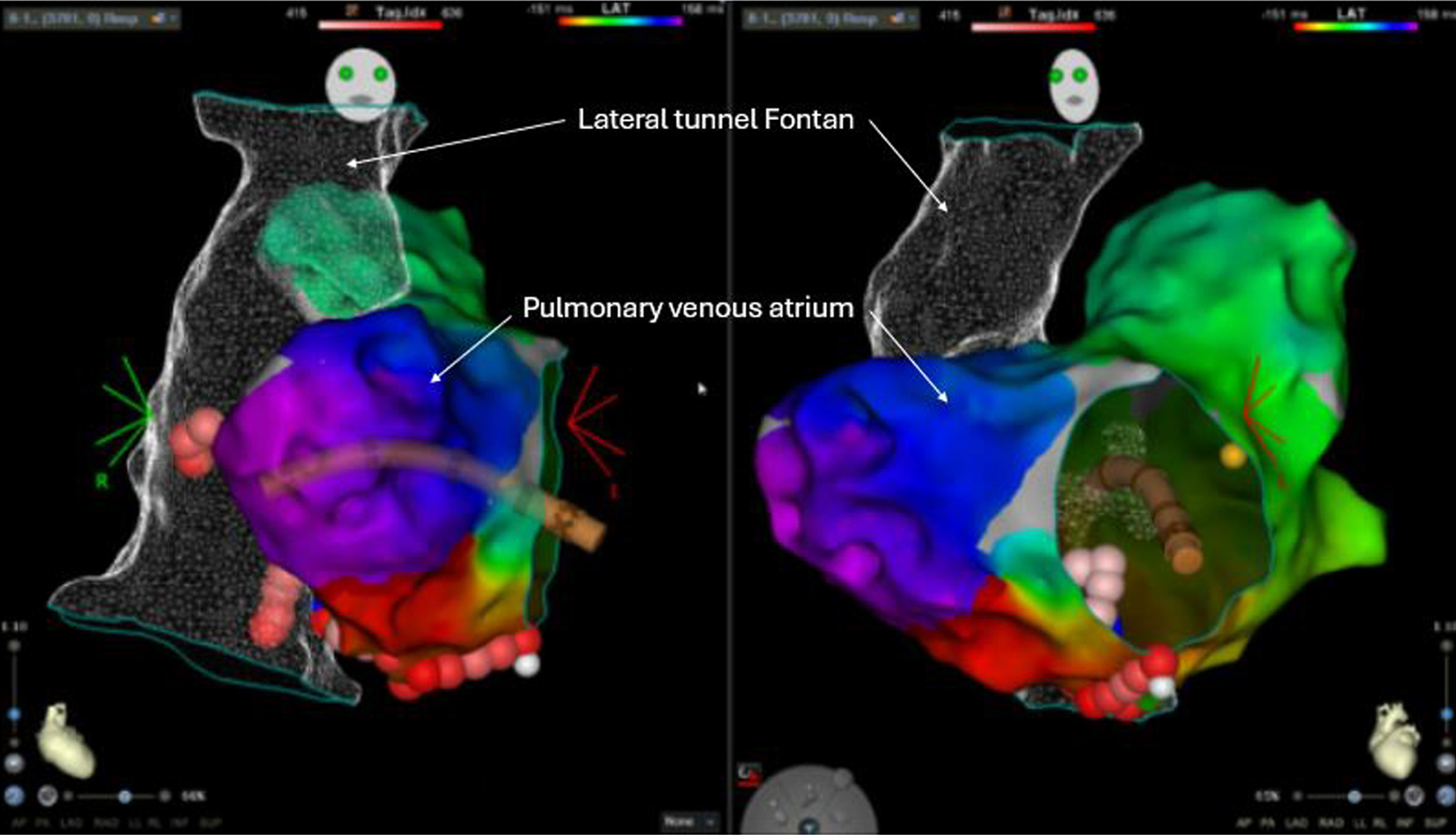 Click for large image | Figure 1. Electroanatomic map for a 26-year-old female with history of hypoplastic left heart syndrome with a lateral tunnel Fontan who underwent electrophysiology study and ablation of atrial flutter. Anterior/posterior (left) and left anterior oblique (right) projections show the lateral tunnel Fontan and the pulmonary venous atrium, which was accessed with trans-baffle puncture and a Vizigo sheath (Carto). Activation map showed counterclockwise cavotricuspid isthmus dependent atrial flutter, which was successfully ablated with ablation (red and pink dots) on both the pulmonary venous atrial and Fontan portion of the cavotricuspid isthmus. |
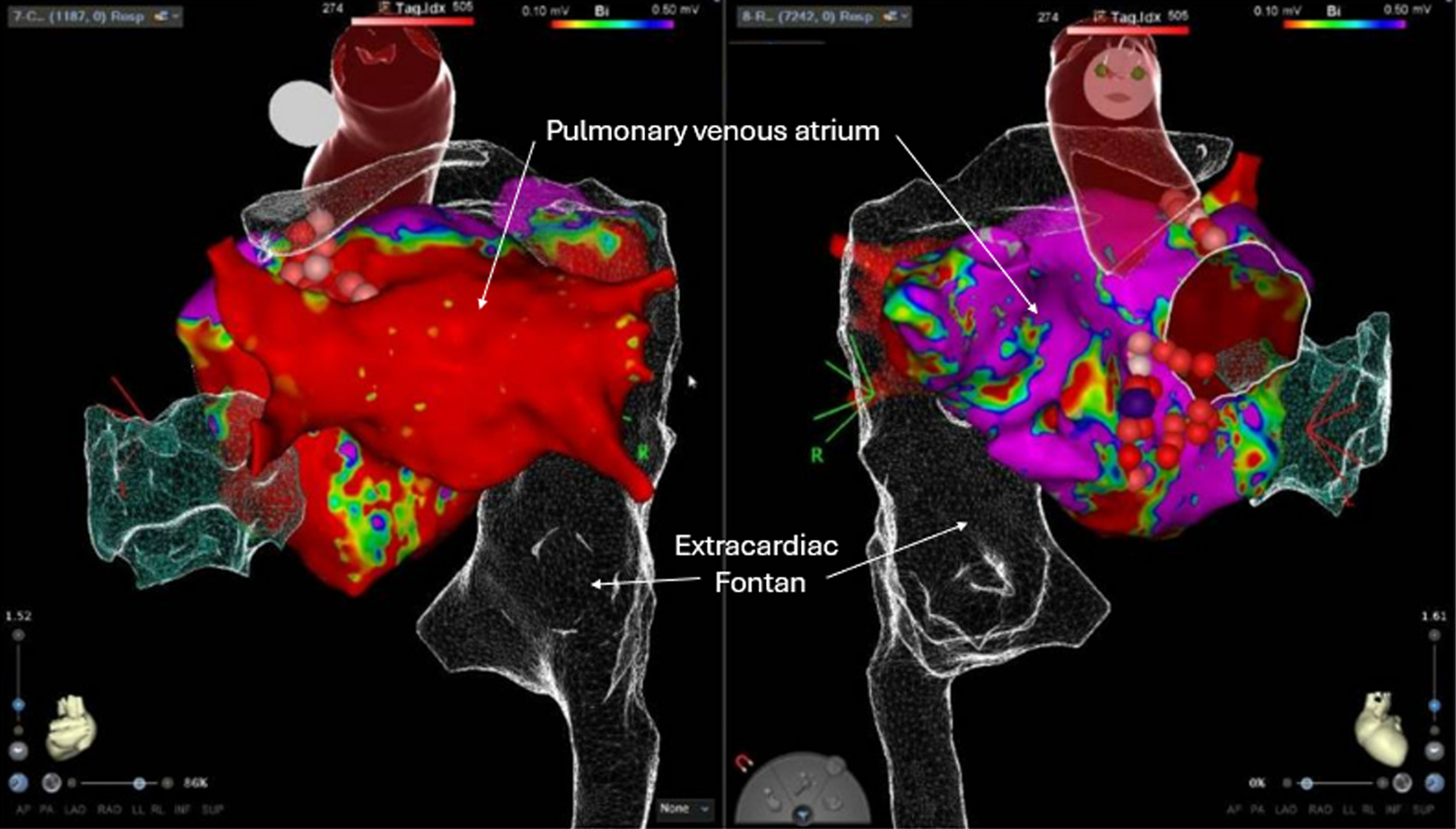 Click for large image | Figure 2. A 30-year-old male with tricuspid and pulmonary atresia status post bidirectional Glenn with anastomosis between the right-sided SVC and right pulmonary artery, classic right atrial appendage-pulmonary artery Fontan procedure, and history of bilateral cryo maze with conversion to extracardiac Fontan, and atrial reduction with septectomy presented for ablation of atypical atrial flutter. Electroanatomical 3D bipolar voltage and activation map created during atrial pacing from the epicardial pacemaker system is shown here. Activation map showed typical flutters with double loop mitral/septal scar re-entry and LA roof/LA appendage reentry that were ablated (red and pink dots). Trans-Fontan baffle puncture and balloon angioplasty of the Fontan baffle was performed for this procedure. LA: left atrial; SVC: superior vena cava. |
Limitations
This observational retrospective study is limited by low power given a small sample size at a single tertiary center, incomplete follow-up, and descriptive nature of clinical variables. The characteristics of patients who were seen at this center may not be representative of all patients with a Fontan undergoing SVT ablations. Outcome estimates may be underestimated as it is possible that patients had hospitalizations, procedures, or follow-up at outside facilities that were not captured in our electronic health record. Multicenter prospective studies are needed to better assess outcomes after SVT ablation in patients who have undergone the Fontan procedure.
Conclusions
Catheter ablation remains safe and effective for managing SVTs that develop after the Fontan procedure. Recurrence rates and repeat ablation rates at 5 years after ablation in this population remain high. Elevated pre- and post-ablation BNP levels and history of AP Fontan approach may help clinicians identify patients at higher risk of atrial arrhythmia recurrence after ablation. Patients with recurrence are at a greater risk of CV hospitalization at 5 years after their initial SVT ablation.
| Supplementary Material | ▴Top |
Suppl 1. Echocardiographic and hemodynamic correlates of atrial arrhythmia recurrence post-ablation in patients with Fontan procedure.
Acknowledgments
The authors would like to thank Kevin Pham for his assistance in identifying patients who met inclusion criteria and gathering basic patient information from the electronic medical record.
Financial Disclosure
Dr. Tan reports consulting for W.L. Gore and Associates. The other authors have no financial disclosures.
Conflict of Interest
The authors have no conflict of interest.
Informed Consent
Informed consent was not required for this IRB approved retrospective study, as it involved the use of de-identified, pre-existing data in accordance with ethical guidelines.
Author Contributions
Khush Kharidia: study design, data collection, data analysis, interpretation of data, manuscript writing and approval. Weiyi Tan: study design, interpretation of data, manuscript writing and approval. Nimesh Patel: study design, data analysis, interpretation of data, manuscript writing and approval.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
AP: atriopulmonary; AT: atrial tachycardia; BNP: brain natriuretic peptide; CHD: congenital heart disease; CPT: Current Procedural Terminology; CV: cardiovascular; EC: extra-cardiac; EKG: electrocardiogram; EP: electrophysiology; ICD: implantable cardioverter-defibrillator; IQR: interquartile range; LT: lateral tunnel; PPM: pacemaker; RA: right atrial; RHC: right heart catheterization; SVT: supraventricular tachycardia; TGA: transposition of great arteries; TA: tricuspid atresia; TTE: transthoracic echocardiogram
| References | ▴Top |
- Downing TE, Allen KY, Glatz AC, Rogers LS, Ravishankar C, Rychik J, Faerber JA, et al. Long-term survival after the Fontan operation: Twenty years of experience at a single center. J Thorac Cardiovasc Surg. 2017;154(1):243-253.e242.
doi pubmed - Dennis M, Zannino D, du Plessis K, Bullock A, Disney PJS, Radford DJ, Hornung T, et al. Clinical outcomes in adolescents and adults after the Fontan procedure. J Am Coll Cardiol. 2018;71(9):1009-1017.
doi pubmed - Quinton E, Nightingale P, Hudsmith L, Thorne S, Marshall H, Clift P, de Bono J. Prevalence of atrial tachyarrhythmia in adults after Fontan operation. Heart. 2015;101(20):1672-1677.
doi pubmed - Laubham M, Blais B, Kamp AN. Atrial arrhythmias in adults with Fontan palliation. Cardiol Ther. 2023;12(3):473-487.
doi pubmed - Song MK, Bae EJ, Kwon BS, Kim GB, Noh CI, Choi JY, Kim WH, et al. Intra-atrial reentrant tachycardia in adult patients after Fontan operation. Int J Cardiol. 2015;187:157-163.
doi pubmed - Giannakoulas G, Dimopoulos K, Yuksel S, Inuzuka R, Pijuan-Domenech A, Hussain W, Tay EL, et al. Atrial tachyarrhythmias late after Fontan operation are related to increase in mortality and hospitalization. Int J Cardiol. 2012;157(2):221-226.
doi pubmed - Khairy P, Fernandes SM, Mayer JE, Jr., Triedman JK, Walsh EP, Lock JE, Landzberg MJ. Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery. Circulation. 2008;117(1):85-92.
doi pubmed - Wan D, Grewal J, Barlow A, Kiess M, Human D, Krahn AD, Riahi M, et al. Atrial arrhythmias and thromboembolic complications in adults post Fontan surgery. Open Heart. 2020;7(2):e001224.
doi pubmed - Egbe AC, Connolly HM, Khan AR, Niaz T, Said SS, Dearani JA, Warnes CA, et al. Outcomes in adult Fontan patients with atrial tachyarrhythmias. Am Heart J. 2017;186:12-20.
doi pubmed - Deal BJ, Costello JM, Webster G, Tsao S, Backer CL, Mavroudis C. Intermediate-term outcome of 140 consecutive fontan conversions with arrhythmia operations. Ann Thorac Surg. 2016;101(2):717-724.
doi pubmed - Moore BM, Anderson R, Nisbet AM, Kalla M, du Plessis K, d'Udekem Y, Bullock A, et al. Ablation of atrial arrhythmias after the atriopulmonary Fontan procedure: mechanisms of arrhythmia and outcomes. JACC Clin Electrophysiol. 2018;4(10):1338-1346.
doi pubmed - Derejko P, Rybicka J, Biernacka EK, Walczak F, Kowalski M, Urbanek P, Bodalski R, et al. Atrial tachycardia ablation in patients with a functional single ventricle after the Fontan surgery. Kardiol Pol. 2016;74(8):762-771.
doi pubmed - Bhaskaran A, Nayyar S, Charla P, Saeed Y, Haldar S, Porta-Sanchez A, Kugamoorthy P, et al. Lateral tunnel Fontan atrial tachycardia ablation trans-baffle access is not mandatory as the initial strategy. J Interv Card Electrophysiol. 2020;58(3):299-306.
doi pubmed - Correa R, Sherwin ED, Kovach J, Mah DY, Alexander ME, Cecchin F, Walsh EP, et al. Mechanism and ablation of arrhythmia following total cavopulmonary connection. Circ Arrhythm Electrophysiol. 2015;8(2):318-325.
doi pubmed - Kamp AN, Nair K, Fish FA, Khairy P. Catheter ablation of atrial arrhythmias in patients post-Fontan. Can J Cardiol. 2022;38(7):1036-1047.
doi pubmed - Klehs S, Schneider HE, Backhoff D, Muller MJ, Paul T, Krause U. Repeat radiofrequency catheter ablation of atrial tachycardias in patients with congenital heart disease. J Cardiovasc Electrophysiol. 2022;33(5):943-952.
doi pubmed - Tops LF, de Groot NM, Bax JJ, Schalij MJ. Fusion of electroanatomical activation maps and multislice computed tomography to guide ablation of a focal atrial tachycardia in a fontan patient. J Cardiovasc Electrophysiol. 2006;17(4):431-434.
doi pubmed - Triedman JK, Alexander ME, Love BA, Collins KK, Berul CI, Bevilacqua LM, Walsh EP. Influence of patient factors and ablative technologies on outcomes of radiofrequency ablation of intra-atrial re-entrant tachycardia in patients with congenital heart disease. J Am Coll Cardiol. 2002;39(11):1827-1835.
doi pubmed - Hiroki J, Mizukami A, Ueshima D, Mashiki J, Miyakuni S, Kono T, Ono M, et al. Propensity-score matched comparison of renal and neurohormonal effects of catheter ablation for frequent premature ventricular contractions in patients with and without systolic dysfunction. J Arrhythm. 2024;40(2):306-316.
doi pubmed - Okada M, Tanaka N, Tanaka K, Hirao Y, Yoshimoto I, Harada S, Onishi T, et al. Usefulness of post-procedural plasma brain natriuretic peptide levels to predict recurrence after catheter ablation of atrial fibrillation in patients with left ventricular systolic dysfunction. Am J Cardiol. 2021;144:67-76.
doi pubmed - Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, Estes NA, III, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2016;13(4):e136-221.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.