| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 16, Number 1, February 2025, pages 64-71
Correlations Between Endothelial Function and Right Ventricular Performance in Primary Hypertension
Lu Wanga, b, Feng Gana, Yu Tong Yanc, Jing Gaob, d
aDepartment of Cardiology, Beijing Aerospace General Hospital, Beijing, China
bDepartment of Cardiology, Xuanwu Hospital, Beijing, China
cNord Anglia School, Xiangcheng, Suzhou, China
dCorresponding Author: Jing Gao, Department of Cardiology, Xuanwu Hospital, Capital Medical University, Beijing, China
Manuscript submitted October 29, 2024, accepted December 12, 2024, published online December 31, 2024
Short title: Endothelial Function and RV Performance in Hypertension
doi: https://doi.org/10.14740/cr1747
| Abstract | ▴Top |
Background: This study aims to elucidate the correlation between endothelial function and both cardiac structure and function in patients newly diagnosed with primary (essential) grade 1 hypertension.
Methods: We retrospectively reviewed clinical and echocardiographic data from 109 patients attending a cardiology outpatient clinic from January to December 2022. All subjects underwent comprehensive laboratory tests including lipid profile, glucose, electrolytes, and high-sensitivity C-reactive protein, alongside echocardiography to assess cardiac function. A subset of 34 patients underwent flow-mediated dilation (FMD) testing to evaluate endothelial function, and the results categorized them into normal (FMD ≥ 6%) and reduced (FMD < 6%) endothelial function groups.
Results: The study found no significant differences in baseline demographic or clinical parameters between groups. Age was negatively correlated with FMD values, indicating decreased endothelial function with advancing age. The normal endothelial function group demonstrated better diastolic and systolic parameters and lower right ventricular Tei indices compared to the reduced function group. Additionally, there was a significant negative correlation between the right ventricular Tei index and FMD values.
Conclusions: Endothelial function is associated with right ventricular performance in patients with primary (essential) grade 1 systemic hypertension. Improved endothelial function is associated with better overall cardiac performance. Further studies with age-matched controls are necessary to confirm these findings and determine the independent effects of hypertension on cardiac function.
Keywords: Echocardiography; Cardiac function; Hypertension; Flow-mediated dilation; Tei index
| Introduction | ▴Top |
Hypertension, characterized by elevated systemic arterial pressure, is predominantly primary (essential) in nature, accounting for over 95% of cases [1]. As a principal risk factor for cardiovascular and cerebrovascular diseases, primary hypertension often coexists with other cardiovascular risk factors and can damage vital organs such as the heart, brain, and kidneys, potentially leading to organ failure [2]. The heart and blood vessels are primary targets of hypertensive damage. Although early stages may show no overt pathological changes, chronic hypertension can lead to left ventricular (LV) hypertrophy and systemic arterial remodeling, leading to ischemia in target organs.
Endothelial dysfunction is one of the earliest and most characteristic pathophysiological changes in primary hypertension [3]. Endothelial cells, a single layer of flat cells lining the blood vessels, play critical roles in cardiovascular homeostasis and immunological responses [4]. Their physiological functions include regulating vasomotion through the release of vasoactive substances, synthesizing and secreting various cytokines, and maintaining the stability of the vascular basement membrane, among others. Endothelial dysfunction is a reversible condition, and improving endothelial function can mitigate a range of diseases caused by disturbances in endothelial integrity [5].
Various clinical techniques exist for assessing endothelial function, such as quantitative coronary angiography and flow-mediated dilation (FMD). FMD is a noninvasive ultrasound method that measures the vasodilatory response of a conduit artery, typically the brachial artery, to increased shear stress following transient arterial occlusion [6]. This method evaluates the endothelium’s ability to release nitric oxide and induce vasodilation in response to increased blood flow, reflecting overall endothelial health. In contrast, quantitative coronary angiography is an invasive procedure involving the direct visualization of the coronary arteries using contrast dye and X-ray imaging, often assessing endothelial function by measuring vasomotor responses to pharmacological agents. While coronary angiography provides detailed information about coronary endothelial function and is considered the gold standard, its invasive nature limits its use in routine clinical practice [7]. FMD, on the other hand, offers a practical and noninvasive alternative that correlates well with coronary angiography results, making it widely used for evaluating systemic endothelial function in both clinical and research settings [8]. Conventional echocardiographic indices like the left ventricular ejection fraction (LVEF) and the ratio of early (E) to late (A) ventricular filling velocities (E/A ratio) often do not fully reflect cardiac function. The E/A ratio assesses diastolic function by comparing the velocities of early (E peak) and late (A peak) ventricular filling during diastole. However, it can be influenced by factors like heart rate (HR) and loading conditions. The Tei index, also known as the myocardial performance index, which includes isovolumetric contraction and relaxation times relative to ejection time, provides a valuable measure of overall cardiac performance, has a normal reference range for the LV Tei index typically between 0.39 and 0.45 indicating normal global ventricular function, and remains relatively stable with age after 3 years [9].
Given the scarcity of studies on the relationship between endothelial and cardiac functions in patients with primary grade 1 hypertension, this study aims to compare cardiac functions between groups with normal and reduced endothelial functions, analyze echocardiographic parameters and clinical characteristics, identify sensitive early indicators of cardiac function, and explore the correlation between endothelial and cardiac functions, thereby offering references for clinical judgment and timely intervention.
| Materials and Methods | ▴Top |
Ethics statement
This study was conducted as a retrospective analysis using fully anonymized data to ensure the confidentiality and privacy of all participants. Given the noninvasive and retrospective nature of the study, where no identifiable personal information was accessed or used in the analysis, the study protocol was reviewed and approved by the Ethics Committee of Xuanwu Hospital (13JL34) and conducted in accordance with the Declaration of Helsinki. All participants involved in this study signed written informed consent to participate for their clinical data to be used in future research at the time of their initial evaluation.
Study design
From January to December 2022, 109 patients with newly diagnosed primary grade 1 hypertension who visited the cardiology outpatient clinic in hospital were included. Among them, 34 underwent further FMD and tissue Doppler examinations.
Inclusion and exclusion criteria
Inclusion criteria
The patient was diagnosed with primary grade 1 hypertension according to the 2018 Revision of Chinese Hypertension Prevention and Treatment Guidelines [10].
Exclusion criteria
Exclusion criteria included: 1) patients with diabetes, impaired glucose tolerance, or fasting hyperglycemia; 2) patients with liver or kidney dysfunction, arrhythmias, valvular regurgitation, valvular heart disease, coronary artery disease, heart failure, secondary hypertension, thyroid dysfunction, cerebrovascular or peripheral vascular disease, or autoimmune diseases; 3) patients who smoke, abuse alcohol or drugs; 4) pregnant or breastfeeding women; 5) patients with incomplete data.
Blood pressure measurement
Blood pressure was measured twice, at least 3 min apart, after a 5-min rest in a seated position, without smoking, caffeine, or tea consumption 30 min prior. If the systolic or diastolic readings differed by more than 5 mm Hg between the two measurements, a third measurement was taken. The average of the two closest readings was then used for analysis.
General and laboratory examinations
Patients underwent venous blood sampling and provided baseline data (age, history of hypertension, diabetes, coronary artery disease, etc.) within 12 h of their visit. All subjects received routine blood test, liver and kidney function tests, lipid profiles, electrolytes, glucose, homocysteine, high-sensitivity C-reactive protein, electrocardiogram (ECG), and echocardiogram.
FMD assessment
FMD was performed by experienced physicians under controlled conditions using a PHILIPS EPIQ7C ultrasound machine. Patients lay supine with their right arm extended at a 15° angle, and the probe was placed 2 - 15 cm above the elbow for longitudinal scanning of the brachial artery. After image optimization (clearly displaying the anterior and posterior intimal lines with good color flow), measurements were triggered by the R-wave on the ECG at the end of arterial dilation, recorded twice, and averaged to determine the brachial artery diameter. After a 30-min rest, the basal diameter (D0) was measured, followed by cuff inflation above systolic pressure by 50 mm Hg for 5 min to induce reactive hyperemia. The post-occlusion diameter (D1) was measured 60 s after cuff release. FMD was calculated as ((D1 - D0)/D0) × 100%. The representative image is shown in Figure 1.
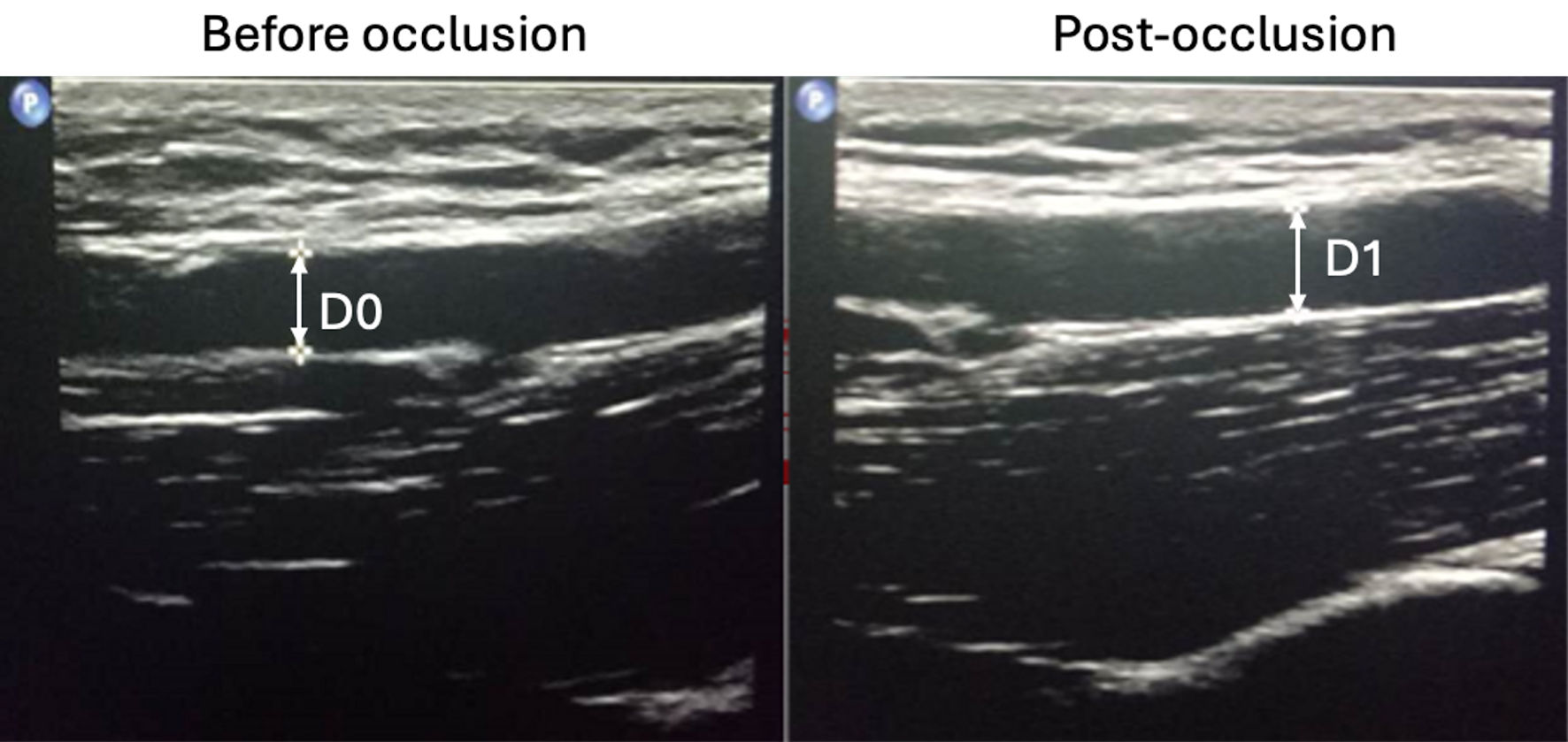 Click for large image | Figure 1. Flow-mediated dilation (FMD) measurement. The baseline diameter (D0) of the artery was measured under resting conditions. Subsequently, a cuff was inflated to 50 mm Hg above systolic pressure for 5 min to induce reactive hyperemia. Following cuff release, the post-occlusion diameter (D1) was measured 60 s later. |
Conventional echocardiographic parameters
All enrolled patients underwent echocardiography using the Philips EPIQ 7C device and an S4-2 phased-array probe. The examination was conducted in the left lateral decubitus position, starting with a standard two-dimensional scan from parasternal and apical windows to assess LV long-axis and short-axis planes and apical four-chamber views. Pulsed Doppler ultrasound sampled 1 cm below the mitral valve to measure early (E peak) and late (A peak) diastolic flow velocities over three cardiac cycles.
Tissue Doppler imaging
Tissue Doppler measurements included early (e’) and late (a’) diastolic velocities at the septal and lateral sides of the mitral annulus, sampled within 1 cm of the septal or lateral myocardium beneath the annulus. The angle between the ultrasound beam and cardiac motion was minimized to less than 20°, with a recording speed of 50 - 100 cm/s. Measurements were averaged over at least three cardiac cycles, adhering to the American Society of Echocardiography (ASE) 2010 guidelines for evaluating adult right heart function [11].
Tei index measurement
The Tei index was measured using tissue Doppler imaging at the apical four-chamber view, capturing the motion spectrum at the junction of the valvular anterior leaflets and the annulus. The intervals (a) between the end of the atrial wave (Aa) and the start of the next early diastolic wave (Ea) and duration (b), which is the ejection time (ET), were measured and used to calculate the Tei index as (a - b)/b (Fig. 2). Measurements were performed by the same operator, ensuring the ultrasound beam was parallel or at an angle less than 15° to the direction of blood flow or annular motion, with measurements averaged over three cardiac cycles.
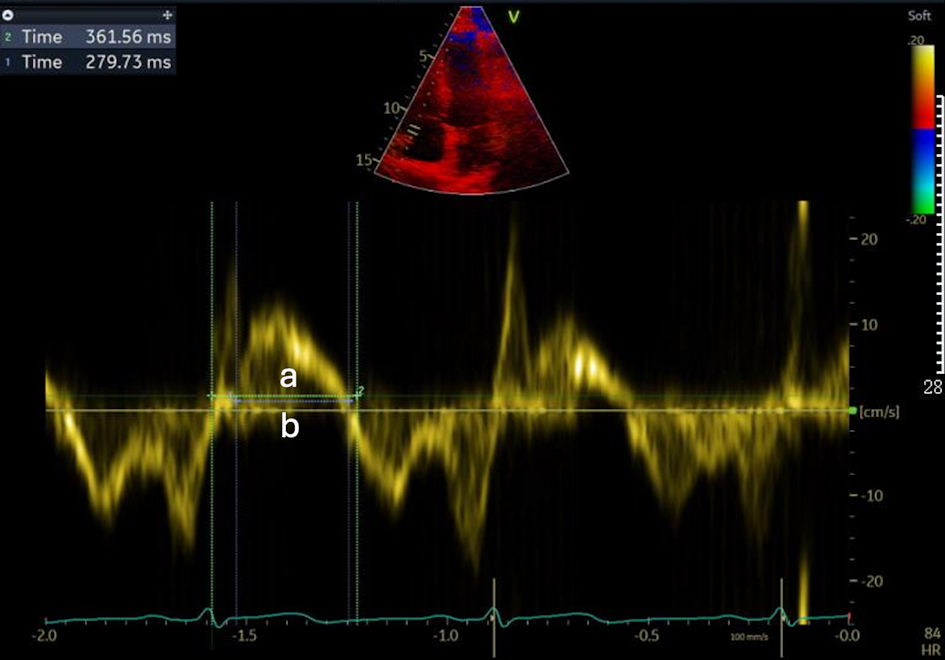 Click for large image | Figure 2. Tei index measurement. Tei index = (a - b)/b = (ICT + IRT)/ET. ET: ejection time; IRT: isovolumetric relaxation time; ICT: isovolumetric contraction time; Tei index: myocardial performance index. |
Statistical analysis
Data were analyzed using SPSS 24.0. Participants were divided into two groups based on FMD ≥ 6%. Continuous variables following a normal distribution were analyzed using t-tests, while non-normal distributions used the rank-sum test. Correlations were assessed using Pearson’s correlation method, with significance set at P < 0.05.
| Results | ▴Top |
This study enrolled 109 patients with newly diagnosed primary grade 1 hypertension, including 52 males (average age: 45.44 ± 12.35 years) and 57 females (average age: 52.80 ± 11.65 years). All participants had normal liver and kidney function, electrolytes, blood glucose, and procalcitonin levels. Among these, 22 were obese, two underweight, 60 had hyperlipidemia, 27 had hyperuricemia, 16 had H-type hypertension, three had elevated white blood cell count, three had increased high-sensitivity C-reactive protein, and abnormalities were observed in three aortic sinus diameters and eight left atrial diameters. The LV systolic and diastolic functions were within normal limits across all participants.
Clinical and echocardiographic data comparison
Participants were divided into two groups based on FMD ≥ 6%. The normal endothelial function group (20 patients) had an average age of 44.29 ± 11.44 years, and the reduced endothelial function group (14 patients) had an average age of 56.60 ± 8.59 years, which was significantly higher (P < 0.05). There were no significant differences in gender, HR, body mass index (BMI), total cholesterol (TC), and other general clinical data (Table 1).
 Click to view | Table 1. Comparison of General Clinical Data Between Groups |
Echocardiographic comparisons
Patients were divided into two groups based on whether their FMD was ≥ 6%, indicating normal endothelial function, or < 6%, indicating reduced endothelial function. There were 20 patients in the normal endothelial function group and 14 in the reduced endothelial function group. The normal endothelial function group exhibited significantly higher values for E peak, s’1, e’1, e’2, right ventricle e’, and tricuspid annular plane systolic excursion (TAPSE), compared to those of the reduced endothelial function group. Additionally, the right ventricular (RV) Tei index was significantly lower in the normal endothelial function group (P < 0.05). There were no significant differences in other echocardiographic data including aortic sinus diameter, left atrium (LA) and LV end-diastolic volume (EDV), cardiac output (CO), stroke volume (SV), E peak, A peak, pulmonary artery ejection time (PAET), aortic ejection time, LV isovolumic relaxation time (IRT), LV isovolumic contraction time (ICT), peak systolic velocity of the lateral wall mitral annulus (s’2), RV IRT, the late diastolic velocity of the free wall tricuspid annulus (RV a’), isovolumic relaxation time of the free wall tricuspid annulus (IRT, RV), isovolumic contraction time of the free wall tricuspid annulus (ICT, RV), LV Tei index, left ventricular posterior wall (LVPW), LVEF, late diastolic velocity of the interventricular septal mitral annulus (a’1) and the lateral wall mitral annulus (a’2), isovolumic contraction time of the lateral wall mitral annulus (ICT2) (all P > 0.05). Specific details are presented in Table 2.
 Click to view | Table 2. Comparison of Echocardiographic Parameters Between Groups |
Correlation analysis of FMD
Using age, sex, HR, and other variables in a Pearson correlation analysis, age, E peak, and early diastolic velocities showed significant correlations with FMD. Specifically, age was inversely correlated with FMD (r = -0.536, P = 0.001), and RV early diastolic velocity (e’ RV) showed the strongest positive correlation (r = 0.624, P < 0.001) (Table 3).
 Click to view | Table 3. Correlation Factors of FMD |
| Discussion | ▴Top |
Cardiovascular diseases (CVDs) have emerged as a significant global health threat, leading to the highest mortality rates among non-communicable diseases worldwide, with an increasing trend among younger populations [12]. According to the World Health Organization’s Global Health Estimates 2016, CVDs cause one-third of all deaths annually in the United States and up to 45% in Europe, with mortality rates in rural and urban China at 44.6% and 42.5%, respectively [13]. Hypertension is a crucial risk factor for coronary artery disease, heart failure, and stroke, and is predicted to affect 29.2% of the global population by 2025 [14].
Aging is recognized as a primary risk factor for the development of many CVDs, including hypertension. It is associated with increased arterial elastance, leading to arterial stiffness and elevated peripheral resistance [15]. As arteries stiffen with age, their ability to expand and recoil during the cardiac cycle diminishes, resulting in increased systolic blood pressure and pulse pressure. This increased arterial stiffness contributes to the development and progression of hypertension. Arterial elastance reflects the net arterial load exerted on the left ventricle and is a key determinant of ventricular-arterial coupling. A previous study that examined aging individuals without CVDs found that ventricular-arterial coupling was markedly reduced due to increased arterial elastance and LV end-systolic elastance, indicating that arterial stiffness and myocardial stiffness both contribute to altered cardiovascular performance in the elderly [16]. This finding suggests that even in the absence of overt CVD, age-related changes in vascular and myocardial stiffness can significantly impact cardiac function. In addition, vascular aging and endothelial dysfunction, significantly tied to decreased bioavailability of nitric oxide - a crucial vasodilator - play pivotal roles in the pathogenesis of CVDs. Studies have shown that endothelial function declines with age, emphasizing the importance of early assessment and intervention in managing hypertension, particularly in individuals over the age of 55 [17].
Primary hypertension is a heterogeneous systemic disease characterized by systemic arterial spasms and increased peripheral resistance. It is a risk factor for various structural and functional cardiovascular changes, including myocardial and vascular remodeling which impact both ventricular functions. RV function is less studied due to the complex geometry and its position in the thorax, which imposes certain limitations on conventional diagnostic approaches [17]. However, research has identified the right ventricle as a primary site of hypertensive cardiac damage [18]. Early stages of hypertension may show no significant changes in LV function, whereas RV function might already be compromised [19]. This suggests that conventional measures like the LVEF may not fully reflect early cardiac dysfunction. This study supports findings that endothelial function is closely related to RV performance and could serve as a sensitive indicator of early cardiac function in hypertension.
Previous study investigated patients with varying durations of hypertension and different blood pressure stages to explore the relationship between the Tei index and RV damage [20]. It was found that in early hypertension, the RV Tei index increases even when the LV Tei index is within the normal range. Our study, involving patients with primary grade 1 hypertension, indicated no significant differences in atrial and septal dimensions, nor in LV Tei index changes between groups based on endothelial function. However, significant differences in the RV Tei index suggest early changes in RV function that precede those in LV function, indicating early cardiac damage due to hypertension.
Our findings also suggest that improvements in endothelial function can significantly lower the risk of cardiovascular events. For instance, in a study where endothelial function was assessed before and after treatment in hypertensive postmenopausal women, those with improved function demonstrated a considerably lower rate of cardiovascular events compared to those without improvement. Furthermore, tissue Doppler imaging has proven superior to conventional echocardiography in detecting early cardiac dysfunction, suggesting its utility in routine clinical assessment of cardiac function in hypertensive patients. Given the complexity and systemic nature of hypertension, a comprehensive approach that includes early assessment and intervention of endothelial function could significantly enhance cardiovascular outcomes.
Limitations
One of the primary limitations of our study is the lack of an age-matched normotensive control group. Age is a well-known factor affecting both endothelial function and cardiac performance. The reduced endothelial function group was significantly older than the normal endothelial function group, which raises the possibility that age, rather than hypertension alone, may have influenced our findings. Previous studies have indicated that endothelial function declines with age due to decreased nitric oxide bioavailability and increased oxidative stress [17, 21]. Therefore, without age-matched controls, it is challenging to discern the extent to which our observations are attributable to hypertension versus age-related changes. Moreover, the small sample size and cross-sectional design limit our ability to generalize the results and establish causality. Future longitudinal studies with larger cohorts and inclusion of age-matched normotensive controls are essential to validate our findings and to explore the temporal relationship between endothelial dysfunction and RV impairment in hypertension.
Conclusions
This study suggests a correlation between endothelial function and RV performance in patients with primary grade 1 hypertension. Specifically, reduced endothelial function is associated with impaired RV diastolic and systolic parameters and a higher RV Tei index. However, due to the absence of an age-matched normotensive control group and the significant age difference between groups, we cannot exclude the influence of age as a confounding factor. Future studies involving larger populations and age-matched normotensive controls are necessary to confirm these associations and to isolate the effects of hypertension from age-related changes on cardiac function.
Acknowledgments
We appreciate all participants involved in this study.
Financial Disclosure
None to declare.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
Informed consent was obtained.
Author Contributions
LW conducted the study, analyzed and interpreted the results, and prepared the initial draft of the manuscript. FG provided support for the interpretation of the results. YTY handled the data collection and classification. JG conceived and designed the study.
Data Availability
The data that support the findings of this study are not publicly available due to their containing information that could compromise the privacy of research participants but are available from the corresponding author JG upon reasonable request.
Abbreviations
A: late diastolic filling velocity; a’: late diastolic mitral annular velocity; CVDs: cardiovascular diseases; E: early diastolic filling velocity; e’: early diastolic mitral annular velocity; FMD: flow-mediated dilation; LA: left atrium; LVEF: left ventricular ejection fraction; LVPW: left ventricular posterior wall; LV: left ventricular; TAPSE: tricuspid annular plane systolic excursion; Tei index: myocardial performance index
| References | ▴Top |
- Oparil S, Acelajado MC, Bakris GL, Berlowitz DR, Cifkova R, Dominiczak AF, Grassi G, et al. Hypertension. Nat Rev Dis Primers. 2018;4:18014.
doi pubmed - Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75(2):285-292.
doi pubmed - Gallo G, Volpe M, Savoia C. Endothelial dysfunction in hypertension: current concepts and clinical implications. Front Med (Lausanne). 2021;8:798958.
doi pubmed - Li G, Gao J, Ding P, Gao Y. The role of endothelial cell-pericyte interactions in vascularization and diseases. J Adv Res. 2025;67:269-288.
doi pubmed - Ananthakrishna R, Shankarappa RK, Rangan K, Chandrasekaran D, Nanjappa MC. Endothelial function and carotid intimal medial thickness in asymptomatic subjects with and without cardiovascular risk factors. Cardiol Res. 2012;3(4):180-186.
doi pubmed - Sena CM, Goncalves L, Seica R. Methods to evaluate vascular function: a crucial approach towards predictive, preventive, and personalised medicine. EPMA J. 2022;13(2):209-235.
doi pubmed - Minhas AS, Goerlich E, Corretti MC, Arbab-Zadeh A, Kelle S, Leucker T, Lerman A, et al. Imaging assessment of endothelial function: an index of cardiovascular health. Front Cardiovasc Med. 2022;9:778762.
doi pubmed - Oz F, Elitok A, Bilge AK, Mercanoglu F, Oflaz H. Relationship Between Brachial Artery flow-mediated dilation, carotid artery intima-media thickness and coronary flow reserve in patients with coronary artery disease. Cardiol Res. 2012;3(5):214-221.
doi pubmed - Nada T, Fukuda N, Yamaguchi Y, Shinohara H, Sakabe K, Morishita S, Fukuda Y, et al. [Age-related changes in cardiac performance index (TEI index) with special reference to the difference between the ventricles]. J Cardiol. 2007;49(6):337-344.
pubmed - Prevention CH. Guidelines for the prevention and treatment of hypertension in China (2018 Revised Edition). Chin J Cardiovasc Med. 2019;24(01):24-56.
- Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685-713.
doi pubmed - Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021.
doi pubmed - Di Cesare M, Perel P, Taylor S, Kabudula C, Bixby H, Gaziano TA, McGhie DV, et al. The heart of the world. Glob Heart. 2024;19(1):11.
doi pubmed - Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223-237.
doi pubmed - Redfield MM, Jacobsen SJ, Borlaug BA, Rodeheffer RJ, Kass DA. Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation. 2005;112(15):2254-2262.
doi pubmed - Sonaglioni A, Baravelli M, Lombardo M, Sommese C, Anza C, Kirk JA, Padeletti L. Ventricular-arterial coupling in centenarians without cardiovascular diseases. Aging Clin Exp Res. 2018;30(4):367-373.
doi pubmed - Seals DR, Jablonski KL, Donato AJ. Aging and vascular endothelial function in humans. Clin Sci (Lond). 2011;120(9):357-375.
doi pubmed - Ryan JJ, Archer SL. The right ventricle in pulmonary arterial hypertension: disorders of metabolism, angiogenesis and adrenergic signaling in right ventricular failure. Circ Res. 2014;115(1):176-188.
doi pubmed - Akintunde AA, Akinwusi PO, Familoni OB, Opadijo OG. Effect of systemic hypertension on right ventricular morphology and function: an echocardiographic study. Cardiovasc J Afr. 2010;21(5):252-256.
doi pubmed - Akintunde AA, Akinwusi PO, Opadijo GO. Relationship between Tei index of myocardial performance and left ventricular geometry in Nigerians with systemic hypertension. Cardiovasc J Afr. 2011;22(3):124-127.
doi pubmed - Kakabadze K, Megreladze I, Khvichia N, Mitagvaria N, Kipiani N, Dumbadze M, Sanikidze T. Some aspects of role of nitric oxide in the mechanisms of hypertension (Experimental Study). Cardiol Res. 2021;12(1):16-24.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.