| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Review
Volume 000, Number 000, June 2025, pages 000-000
Pulmonary Arterial Hypertension and Left Heart Disease Phenotype: A Challenging Crossroad
aCardiology Division, Cardinal G. Massaia Hospital, Asti, Italy
bPulmonary Hypertension Outpatient Clinic, University of Genoa, Genoa, Italy
cCorresponding Author: Riccardo Scagliola, Cardiology Division, Cardinal G. Massaia Hospital, Asti, Italy
Manuscript submitted March 29, 2025, accepted June 5, 2025, published online June 16, 2025
Short title: PAH and LHD Phenotype
doi: https://doi.org/10.14740/cr2067
- Abstract
- Introduction
- Epidemiology
- Pathophysiology
- Hemodynamic Features
- Non-Invasive Tools
- Clinical Outcomes and Response to Pharmacological Treatment
- Therapeutic Approaches
- Conclusions
- References
| Abstract | ▴Top |
Although pulmonary arterial hypertension (PAH) usually affects young people with a low burden of cardiovascular comorbidities, epidemiologic changes over time have been providing a codified phenotype of subjects with PAH, characterized by a hemodynamic profile compatible with pure pre-capillary pulmonary hypertension (PH), associated with increased risk factors for left heart disease (LHD). Compared with the younger subjects belonging to the classical PAH phenotype, those with PAH and LHD phenotype share several distinctive features. They include: 1) the older mean age at diagnosis of PAH; 2) peculiar hemodynamic features, characterized by a trend toward lower values of mean pulmonary arterial pressure and pulmonary vascular resistances, and higher values of pulmonary artery wedge pressure; 3) greater clinical deterioration; 4) more impaired exercise capacity; 5) higher mortality risk; 6) weaker response to PAH-targeted treatment; and 7) higher rate of PAH drug discontinuation. Physicians must be aware of such peculiar phenotype of PAH. This is advisable for providing a comprehensive diagnostic workup, in order to reduce the risk of PH misclassification and provide the most appropriate decision-making approach.
Keywords: Pulmonary arterial hypertension; Left heart disease; Cardiovascular risk factors; Diagnostic workup; Decision-making approach
| Introduction | ▴Top |
Pulmonary hypertension (PH) is a hemodynamic condition characterized by mean pulmonary arterial pressure (mPAP) > 20 mm Hg at rest. This definition encompasses heterogeneous pathophysiological disorders and a wide spectrum of clinical comorbidities. Such heterogeneity actively impacts its natural history and therapeutic approaches. Specifically, PH related to left heart disease (LDH) is defined by pulmonary arterial wedge pressure (PAWP) values > 15 mm Hg. This post-capillary form of PH includes several clinical conditions, such as heart failure with reduce or preserved ejection fraction, left-sided valvular heart disease, and other congenital or acquired conditions leading to increased left atrial pressure and its backward transmission to pulmonary circulation [1]. Conversely, pulmonary arterial hypertension (PAH) is a peculiar type of pre-capillary PH, defined by PAWP values ≤ 15 mm Hg, together with pulmonary vascular resistance (PVR) > 2 Wood Units. In this context, epidemiologic changes over time have progressively codified a distinct subset of PAH subjects, characterized by a hemodynamic profile of purely pre-capillary PH, together with risk factors for LHD, who share several clinical and instrumental features with PH due to LHD. In this regard, a potential crossroad between these two kinds of PH has been hypothesized [2, 3].
| Epidemiology | ▴Top |
Ltaief et al pointed out the pathophysiology, hemodynamic assessment, diagnostic algorithm, and therapeutic strategies in PH associated with LHD [4]. However, in this context, differential diagnosis between pre-capillary and occult post-capillary PH may not always be easily recognizable. Specifically, progressive changes in the demographics of PAH in the last decades underscored a codified phenotype of patients with an increased mean age and risk factors for LHD at the incident diagnosis of PAH. Data from the European COMPERA (Prospective Registry of Newly Initiated Therapies for Pulmonary Hypertension) registry and AMBITION (Ambrisentan and Tadalafil in Patients with Pulmonary Arterial Hypertension) trial showed a higher rate of patients with PAH and age over 65 years, and an increased burden of risk factors for LHD, compared with the younger counterparts [5, 6]. Therefore, the term “atypical PAH” was initially introduced to identify a hybrid phenotype of subjects with a pure pre-capillary PH profile associated with comorbidities and risk factors for LHD, particularly for heart failure with preserved ejection fraction (HFpEF), in whom a pathophysiological crosstalk between these two clinical entities has been hypothesized [1, 7]. However, to date there is still no unanimous consensus on a shared definition of this challenging PAH phenotype. Specifically, the AMBITION trial defined the presence of LHD phenotype by the contextual presence of at least three risk factors of left ventricular (LV) diastolic dysfunction. They include: 1) history of systemic arterial hypertension; 2) diabetes mellitus; 3) a body mass index ≥ 30 kg/m2; and historical evidence of coronary artery disease (established by at least one of the following: 1) history of myocardial infarction; 2) history of percutaneous coronary intervention; 3) positive stress test; 4) previous coronary artery bypass graft; 5) stable angina; or 6) angiographic evidence of > 50% stenosis in ≥ 1 epicardial vessel) [6]. On the contrary, in the COMPERA registry, the presence of a single risk factor for LV diastolic dysfunction was sufficient for defining this patient’s PAH phenotype [5]. Nevertheless, all the aforementioned PAH registries have still adopted the former hemodynamic criteria for defining PAH, involving more stringent values of mPAP and PVR, but identical targets of PAWP. This could represent a potential limitation for further speculations on the demographic changes of subjects with PAH over the last decades. Epidemiologic data referring to the updated PAH hemodynamic criteria, together with shared classification criteria defining LHD risk factors, are advisable in order to better categorize this codified PAH subset.
| Pathophysiology | ▴Top |
Despite its pure pre-capillary hemodynamic profile, the peculiar epidemiologic features of this PAH population have raised further insights suggesting a potential pathophysiologic crossroad between PAH and PH due to LHD, especially related to HFpEF [7]. This intriguing perspective is suggested by several points of convergence and shared neurohormonal pathways predisposing to right ventricular (RV) failure and pulmonary vascular disease in these two PH phenotypes. The progressive impairment of the nitric oxide (NO)-cyclic guanosine monophosphate (cGMP) pathway has been extensively investigated both in subjects with idiopathic PAH and in patients with PH due to LHD. Endothelial dysfunction and the upregulation of phosphodiesterase type 5 in PAH are the main responsible processes of low intracellular levels of cGMP [8]. Similarly, increased inflammatory status and oxidative stress in HFpEF cause cGMP phosphorylation and inhibition of NO delivery, thus leading to endothelial impairment and loss of vascular elastance [9]. Additionally, the endothelin-1 (ET-1) pathway has been reported to play a pivotal role in both PAH and PH due to LHD, as it favors pulmonary vasoconstriction, vascular remodeling, and smooth muscle cell proliferation in patients with PAH. Similarly, ET-1 has been shown to represent an early biochemical marker of pulmonary vascular disease and RV impairment in patients with HFpEF [10]. Furthermore, the decreased production of prostacyclin due to endothelial dysfunction, as well as the impaired balance between vasodilator mediators and vasoconstrictors molecules, such as ET-1 and thromboxane-A2, remains a pathobiological hallmark in PAH, and is exacerbated in subjects with contextual LHD risk factors and comorbidities. Taken together, the aforementioned molecular changes and impaired signaling pathways lead to several pathophysiological consequences, such as pulmonary vasoconstriction, smooth muscle cell proliferation, and platelet aggregation, and contribute to the development of a complex architectural wall derangement including concentric lesions and plexiform lesions. As a consequence of these histopathologic signatures, a maladaptive RV remodeling may occur, and reflects a chronic right-sided pressure overload which is the common scenario seen in the final stage in both PH phenotypes [11]. Ventricular-arterial coupling includes several adaptive mechanisms provided as a reactive adaptation to the increased RV afterload. They include: 1) homeometric adaptation (represented by RV concentric hypertrophy and enhanced contractility, in order to preserve RV systolic and diastolic function and maintain an adequate stroke volume at minimal energetic dissipation) [12]; and 2) heterometric adaptation (a maladaptive RV remodeling leading to an increased RV end-diastolic volume due to RV free wall stretching and distension in order to restore the stroke volume and secure the cardiac output, with a higher oxygen consumption and energetic dissipation) [3, 11, 13, 14]. These compensatory mechanisms are especially damaged in the elderly, who are prone to modulating RV remodeling through cardiomyocyte loss, fiber reorientation, and replacement with fibrous tissue, thus providing a weaker age-related response to pulmonary afterload, compared with younger PAH subjects [15]. Subsequently, when a maladaptive RV remodeling process proceeds and the aforementioned compensatory mechanisms are not sufficient to preserve the cardiac output, ventricular-arterial uncoupling occurs, and reflects the discordance between RV contractility and pulmonary vascular compliance, the prolonged contraction time of RV muscular fibers, and loss of ventricular interdependence secondary to the increased RV afterload. This in turn leads to RV dyssynchrony and further dilatation, with a progressive reduction of stroke volume and cardiac output [16-19]. Of note, although a potential overlap between PAH and PH due to LHD is conceivable, this pathophysiological crossroad remains only partial. In this regard, data on clinical benefits of PAH-targeted therapy in patients with PH due to LHD (characterized by a pure post-capillary hemodynamic profile) are very limited [1, 2]. Further investigation of shared pathophysiological findings and molecular signatures in subjects with PAH and LHD phenotype is needed for better elucidating the pathogenic link between PAH and risk predictors for LHD in these kinds of patients.
| Hemodynamic Features | ▴Top |
Several data from the literature have shown a distinct hemodynamic profile of subjects with PAH and LHD phenotype, characterized by a trend toward higher PAWP values and lower mean PAP and PVR, compared with the younger counterparts without LHD risk factors [20, 21] (Fig. 1). Similarly, the older age at PAH diagnosis and the increasing prevalence of LHD comorbidities raise uncertainties in adequately distinguishing between pre-capillary and post-capillary PH in this population subset. These concerns should be advisable, as they predispose to several implications on the therapeutic approach in these kinds of patients [22-24]. The increasing mean age at PAH diagnosis and the high rate of comorbidities predisposing to LHD raise several concerns about the threshold level of PAWP used to discriminate between pre-capillary and post-capillary PH in these kinds of patients [25]. The inclusion eligibility criterium of a baseline PAWP cut-off value raised to 18 mm Hg in the REVEAL (Registry to Evaluate Early and Long-term PAH Disease Management) registry predisposed to a high likelihood of misclassifying patients with PH due to LHD as subjects belonging to the PAH phenotype [26]. The limitations and uncertainties concerning the use of clear hemodynamic thresholds for a proper PH categorization also include different methods of PAWP measurements, which often lead to a mean difference of PAWP values between 4 and 6 mm Hg. Potential pitfalls and limitations which may hinder occult post-capillary PH include: 1) discrepancies in PAWP reading, due to the respirophasic variations of the intrathoracic pressure during the respiratory cycle; 2) the lack of a standardized method of calibration of the zero reference level during right heart catheterization; 3) the impact of volume depletion on LV unloading, due to pharmacological diuresis and/or low volume intake; and 4) a direct measure of LV end-diastolic pressure, particularly when PAWP measures are not reliably obtainable [9, 27].
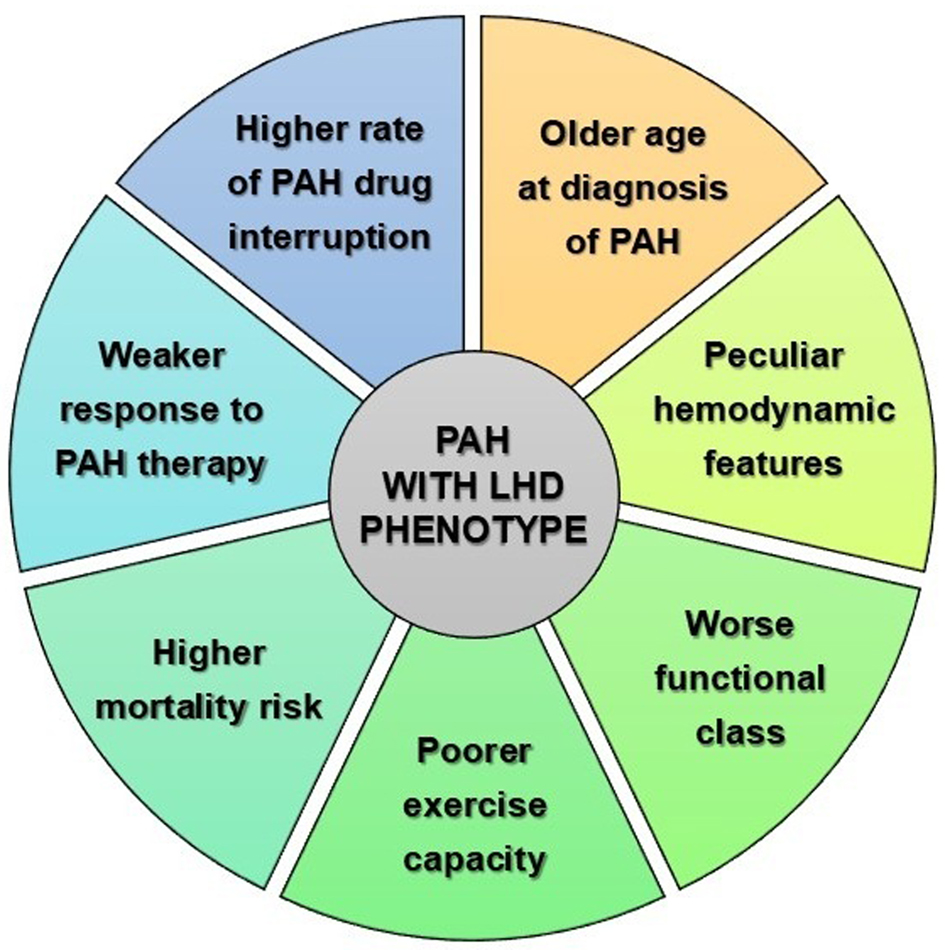 Click for large image | Figure 1. Features of patients with PAH and LHD phenotype. LHD: left heart disease; PAH: pulmonary arterial hypertension. |
| Non-Invasive Tools | ▴Top |
Despite several precautions for the hemodynamic assessment of PAH in subjects with LHD phenotype, hemodynamic findings alone are often insufficient for a proper characterization of this patient population, especially whether invasive results are not consistent with the preliminary clinical suspicion of these kinds of patients. Therefore, several non-invasive tools are helpful in providing further insights for properly phenotyping these kinds of patients. They include: 1) clinical findings of heart failure (e.g., signs and symptoms of lung and/or peripheral congestion, such as pulmonary crackles, peripheral edema, ascites, jugular turgor, and hepatojugular reflux; the presence of S3 and/or S4 sounds, signs of valvular dysfunctions such as heart murmurs, clinical manifestations like asthenia, fatigue, orthopnea, bendopnea, and paroxysmal nocturnal dyspnea); 2) 12-lead electrocardiogram (ECG) (assessing sinus vs. non-sinus rhythm, signs of atrial enlargement, LV or RV hypertrophy, left vs. right axis deviation ischemic or load-induced changes in ventricular repolarization); 3) chest X-ray (e.g., enlargement of right vs. left heart chambers, pulmonary arterial dilatation, peripheral pulmonary arterial pruning, hilar congestion, Kerley B lines, or pleural effusions); 4) transthoracic echocardiography (assessing signs of LV systolic and/or diastolic dysfunction; left atrial enlargement; left-sided valvular disease); 5) cardiac biomarkers (with particular reference to increased levels of high-sensitivity troponin and natriuretic peptides - especially brain natriuretic peptide or N-terminal pro-brain natriuretic peptide - that provide supporting information on the likelihood of heart failure, particularly if confirmed by other non-invasive tools). In line with the aforementioned non-invasive findings, several HFpEF prediction algorithms have been provided (e.g., the H2FPEF and HFA-PEFF scores), although a shared multi-layered prediction model is still missing to date [28-30]. For these reasons, comprehensive diagnostic models incorporating hemodynamic and non-invasive data should be provided, instead of relying on the pure hemodynamic measurements alone [31-34].
| Clinical Outcomes and Response to Pharmacological Treatment | ▴Top |
Compared with younger patients with a classical PAH phenotype, elderly subjects with PAH and LHD phenotype have shown to become symptomatic at lower values of PVR, and to present with worse functional class and more impaired exercise capacity at diagnosis of PAH [1, 2, 6, 35]. These data raise the suspicion of a progressively decline of the RV capability to generate high pulmonary pressures over time, thus hypothesizing that older individuals have a less physiological functional reserve to cope with the progressive increase in pulmonary arterial pressures and RV impairment, than their younger counterparts [22, 36]. Data from the literature highlight the effect of the aging modulation on RV remodeling by several mechanisms, including cardiomyocyte loss and fibrosis substitution; increased peak pressure; and myocardial fiber reorientation, finalized to alter biomechanical properties in a similar way to those occurring in response to RV pressure overload [15]. Additionally, older patients with PAH and LHD phenotype have shown to present a higher mortality risk, a weaker response to PAH-targeted treatment, and a higher rate of PAH drug discontinuation, compared with the younger counterparts [31, 35, 37]. The higher rate of LHD comorbidities, as well as a persistent delay in confirming PAH diagnosis seems to be the main reasons of such a poorer prognostic outcome and worse therapeutic response in this patient population [1, 38]. The first plausible explanation seems to be the persistent delay in diagnosing PAH in this population subset, usually due to the longer duration of symptoms, which are commonly attributed to the older age and other more prevalent comorbidities, rather than suspecting a timely diagnosis of PAH [22, 32, 33]. Additionally, a higher rate of LHD-associated comorbidities seems to be also actively involved in the worse clinical outcome and the weaker pharmacological response in patients with PAH and LHD phenotype [15, 38]. Specifically, several reports suggest how cardiovascular risk factors, such as the impaired lipid metabolism, diabetes mellitus, and insulin resistance, significantly impact on worsening outcomes on clinical impairment, poor prognostic outcome, and weak therapeutic response in patients with PAH, taking into account their pathogenic role in systemic inflammation and coronary microvascular dysfunction, and their implications on RV impairment in PAH subjects [39, 40].
| Therapeutic Approaches | ▴Top |
To date, little evidence-based recommendations are provided for guiding therapeutic strategies of subjects with PAH and LHD phenotype, as they are often under-represented in randomized therapeutic trials, because of their advanced age and the contextual presence of cardiovascular comorbidities [2, 41, 42]. As reported in the latest clinical practice guidelines from the European Society of Cardiology and the European Respiratory Society, initial monotherapy is recommended, in order to reduce the high risk of side effects (such as fluid retention and/or a decline in the peripheral oxygen saturation) in this population subset [1, 35, 43]. Registry data support the use of phosphodiesterase type 5 inhibitors (PDE5I) as a primary treatment option for subjects with PAH and LHD phenotype, as the use of endothelial receptor antagonists has been associated with an increased risk of fluid overload. Little experience is known about the use of prostacyclin analogues or prostacyclin receptor antagonists in this patient population [6, 13, 41]. In this regard, the therapeutic features of sildenafil on cardiovascular comorbidities and risk factors have been widely investigated in either animal models or humans, showing favorable effects either on RV and LV systolic function, or on microcirculation through an acute improvement of coronary functional reserve in patients with microvascular coronary dysfunction, while little is known on their long-term effects in this population subset [44-46]. Additionally, PDE5I have also shown a similar efficacy and safety pharmacological profile, either in elderly subjects with PAH and LHD phenotype, or in the younger PAH counterparts, as shown in the post-hoc analysis of the randomized, double-blind, placebo-controlled phase 3 PHIRST-1 (Pulmonary Arterial Hypertension and Response to Tadalafil) trial [47]. On the other hand, little is known on the therapeutic role of neurohormonal inhibitors (NEUi) (e.g., beta-blockers, angiotensin-converting enzyme inhibitors, angiotensin-2 receptor antagonists, and angiotensin receptor-neprilysin inhibitor) in patients with PAH and LHD phenotype, as these medications are not currently labelled in PAH guidelines, unless required for the management of cardiovascular comorbidities, for which they are recommended instead [1, 48]. In this clinical scenario, data from the literature pointed out the pivotal role of chronic activation of neurohormonal axis in PAH, thus providing novel insights into the potential effects of the neurohormonal blockade as hypothetical therapeutic target on these kinds of patients [49, 50]. However, to date, data related to the therapeutic effects of NEUi in subjects with PAH and LHD phenotype are scarce and often limited to single-center retrospective analysis [51, 52]. Further double-blind, randomized, placebo-controlled trials are warranted to better define the proper therapeutic approach in this population subset.
| Conclusions | ▴Top |
Epidemiologic changes over time underscored a peculiar phenotype of subjects with PAH and LHD risk profile. Despite their pure pre-capillary profile, patients with PAH and LHD phenotype are characterized by distinct hemodynamic features, together with a greater clinical deterioration and impaired exercise capacity, as well as a weaker response to PAH-targeted treatment and a higher rate of PAH drug discontinuation, compared with younger subjects with the classical PAH phenotype. A comprehensive diagnostic algorithm involving hemodynamic measurements and non-invasive findings should be advisable, in order to minimize the risk of underestimating and misclassifying occult forms of post-capillary PH in this population subset.
Acknowledgments
None to declare.
Financial Disclosure
The author declares he has not financial or funding to disclose.
Conflict of Interest
The author declares he has no conflict of interest to disclose.
Author Contributions
Riccardo Scagliola: paper conception and design, literature review, and manuscript writing.
Data Availability
The author declares that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, Carlsen J, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618-3731.
doi pubmed - Opitz CF, Hoeper MM, Gibbs JS, Kaemmerer H, Pepke-Zaba J, Coghlan JG, Scelsi L, et al. Pre-capillary, combined, and post-capillary pulmonary hypertension: a pathophysiological continuum. J Am Coll Cardiol. 2016;68(4):368-378.
doi pubmed - Ruocco G, Gavazzi A, Gonnelli S, Palazzuoli A. Pulmonary arterial hypertension and heart failure with preserved ejection fraction: are they so discordant? Cardiovasc Diagn Ther. 2020;10(3):534-545.
doi pubmed - Ltaief Z, Yerly P, Liaudet L. Pulmonary hypertension in left heart diseases: pathophysiology, hemodynamic assessment and therapeutic management. Int J Mol Sci. 2023;24(12):9971.
doi pubmed - Hoeper MM, Huscher D, Ghofrani HA, Delcroix M, Distler O, Schweiger C, Grunig E, et al. Elderly patients diagnosed with idiopathic pulmonary arterial hypertension: results from the COMPERA registry. Int J Cardiol. 2013;168(2):871-880.
doi pubmed - McLaughlin VV, Vachiery JL, Oudiz RJ, Rosenkranz S, Galie N, Barbera JA, Frost AE, et al. Patients with pulmonary arterial hypertension with and without cardiovascular risk factors: Results from the AMBITION trial. J Heart Lung Transplant. 2019;38(12):1286-1295.
doi pubmed - Scagliola R, Brunelli C, Balbi M. Pulmonary arterial hypertension in the elderly: peculiar features and challenges for a proper phenotyping approach. J Cardiovasc Dev Dis. 2023;10(9):401.
doi pubmed - Chen CN, Watson G, Zhao L. Cyclic guanosine monophosphate signalling pathway in pulmonary arterial hypertension. Vascul Pharmacol. 2013;58(3):211-218.
doi pubmed - van Heerebeek L, Hamdani N, Falcao-Pires I, Leite-Moreira AF, Begieneman MP, Bronzwaer JG, van der Velden J, et al. Low myocardial protein kinase G activity in heart failure with preserved ejection fraction. Circulation. 2012;126(7):830-839.
doi pubmed - Obokata M, Kane GC, Reddy YNV, Melenovsky V, Olson TP, Jarolim P, Borlaug BA. The neurohormonal basis of pulmonary hypertension in heart failure with preserved ejection fraction. Eur Heart J. 2019;40(45):3707-3717.
doi pubmed - Vonk-Noordegraaf A, Haddad F, Chin KM, Forfia PR, Kawut SM, Lumens J, Naeije R, et al. Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol. 2013;62(25 Suppl):D22-33.
doi pubmed - Barilli M, Tavera MC, Valente S, Palazzuoli A. Structural and hemodynamic changes of the right ventricle in PH-HFpEF. Int J Mol Sci. 2022;23(9):4554.
doi pubmed - Montani D, Chaumais MC, Savale L, Natali D, Price LC, Jais X, Humbert M, et al. Phosphodiesterase type 5 inhibitors in pulmonary arterial hypertension. Adv Ther. 2009;26(9):813-825.
doi pubmed - Bernardo RJ, Haddad F, Couture EJ, Hansmann G, de Jesus Perez VA, Denault AY, de Man FS, et al. Mechanics of right ventricular dysfunction in pulmonary arterial hypertension and heart failure with preserved ejection fraction. Cardiovasc Diagn Ther. 2020;10(5):1580-1603.
doi pubmed - Sharifi Kia D, Shen Y, Bachman TN, Goncharova EA, Kim K, Simon MA. The Effects of Healthy Aging on Right Ventricular Structure and Biomechanical Properties: A Pilot Study. Front Med (Lausanne). 2021;8:751338.
doi pubmed - Thenappan T, Prins KW, Cogswell R, Shah SJ. Pulmonary hypertension secondary to heart failure with preserved ejection fraction. Can J Cardiol. 2015;31(4):430-439.
doi pubmed - Gerges M, Gerges C, Pistritto AM, Lang MB, Trip P, Jakowitsch J, Binder T, et al. Pulmonary hypertension in heart failure. epidemiology, right ventricular function, and survival. Am J Respir Crit Care Med. 2015;192(10):1234-1246.
doi pubmed - Melenovsky V, Hwang SJ, Lin G, Redfield MM, Borlaug BA. Right heart dysfunction in heart failure with preserved ejection fraction. Eur Heart J. 2014;35(48):3452-3462.
doi pubmed - Harrison A, Hatton N, Ryan JJ. The right ventricle under pressure: evaluating the adaptive and maladaptive changes in the right ventricle in pulmonary arterial hypertension using echocardiography (2013 Grover Conference series). Pulm Circ. 2015;5(1):29-47.
doi pubmed - Ozpelit E, Akdeniz B, Sezgin D, Sevinc C, Tertemiz KC, Ozpelit ME, Baris M, et al. Clinical and hemodynamic profiles of elderly patients with pulmonary arterial hypertension: a single center, prospective study. J Geriatr Cardiol. 2017;14(1):20-27.
doi pubmed - Afshar M, Collado F, Doukky R. Pulmonary hypertension in elderly patients with diastolic dysfunction and preserved ejection fraction. Open Cardiovasc Med J. 2012;6:1-8.
doi pubmed - Ling Y, Johnson MK, Kiely DG, Condliffe R, Elliot CA, Gibbs JS, Howard LS, et al. Changing demographics, epidemiology, and survival of incident pulmonary arterial hypertension: results from the pulmonary hypertension registry of the United Kingdom and Ireland. Am J Respir Crit Care Med. 2012;186(8):790-796.
doi pubmed - Halpern SD, Taichman DB. Misclassification of pulmonary hypertension due to reliance on pulmonary capillary wedge pressure rather than left ventricular end-diastolic pressure. Chest. 2009;136(1):37-43.
doi pubmed - Jansen SMA, Huis In 't Veld AE, Tolen P, Jacobs W, Willemsen HM, Grotjohan HP, Waskowsky M, et al. Clinical characteristics of patients undergoing right heart catheterizations in community hospitals. J Am Heart Assoc. 2022;11(17):e025143.
doi pubmed - Hoeper MM, Lam CSP, Vachiery JL, Bauersachs J, Gerges C, Lang IM, Bonderman D, et al. Pulmonary hypertension in heart failure with preserved ejection fraction: a plea for proper phenotyping and further research. Eur Heart J. 2017;38(38):2869-2873.
doi pubmed - Badesch DB, Raskob GE, Elliott CG, Krichman AM, Farber HW, Frost AE, Barst RJ, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest. 2010;137(2):376-387.
doi pubmed - Scagliola R. Pulmonary arterial hypertension and pulmonary hypertension due to left heart disease: so near and yet so far. Pol Arch Intern Med. 2020;130(4):349-350.
doi pubmed - Amanai S, Harada T, Kagami K, Yoshida K, Kato T, Wada N, Obokata M. The H(2)FPEF and HFA-PEFF algorithms for predicting exercise intolerance and abnormal hemodynamics in heart failure with preserved ejection fraction. Sci Rep. 2022;12(1):13.
doi pubmed - Reddy YNV, Carter RE, Obokata M, Redfield MM, Borlaug BA. A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation. 2018;138(9):861-870.
doi pubmed - Shapiro BP, McGoon MD, Redfield MM. Unexplained pulmonary hypertension in elderly patients. Chest. 2007;131(1):94-100.
doi pubmed - Takahashi Y, Yamamoto K, Tanabe N, Suda R, Koshikawa K, Ikubo Y, Suzuki E, et al. Characteristics of Japanese elderly patients with pulmonary arterial hypertension. Pulm Circ. 2020;10(3):2045894020954158.
doi pubmed - Shimony A, Fox BD, Afilalo J, Rudski LG, Hirsch A, Langleben D. Pulmonary arterial hypertension in the elderly-clinical characteristics and long-term survival. Lung. 2012;190(6):645-649.
doi pubmed - Zhang YY, Xu F, Chu M, Bi LQ. Pulmonary arterial hypertension in critically ill elderly patients. Pak J Med Sci. 2017;33(1):27-32.
doi pubmed - Kovacs G, Avian A, Olschewski A, Olschewski H. Zero reference level for right heart catheterisation. Eur Respir J. 2013;42(6):1586-1594.
doi pubmed - Hoeper MM, Pausch C, Grunig E, Klose H, Staehler G, Huscher D, Pittrow D, et al. Idiopathic pulmonary arterial hypertension phenotypes determined by cluster analysis from the COMPERA registry. J Heart Lung Transplant. 2020;39(12):1435-1444.
doi pubmed - Foley RJ, Wilcox D, Walsh SJ, Azrin M, Hager WD. Survival of geriatric idiopathic pulmonary arterial hypertension patients. Conn Med. 2011;75(1):11-15.
pubmed - Arvanitaki A, Vrana E, Boutsikou M, Anthi A, Apostolopoulou S, Avgeropoulou A, Demerouti E, et al. The impact of cardiovascular comorbidities associated with risk for left heart disease on idiopathic pulmonary arterial hypertension: Data from the Hellenic Pulmonary Hypertension Registry (HOPE). Pulm Circ. 2022;12(2):e12086.
doi pubmed - Hjalmarsson C, Radegran G, Kylhammar D, Rundqvist B, Multing J, Nisell MD, Kjellstrom B, et al. Impact of age and comorbidity on risk stratification in idiopathic pulmonary arterial hypertension. Eur Respir J. 2018;51(5):1702310.
doi pubmed - Charalampopoulos A, Howard LS, Tzoulaki I, Gin-Sing W, Grapsa J, Wilkins MR, Davies RJ, et al. Response to pulmonary arterial hypertension drug therapies in patients with pulmonary arterial hypertension and cardiovascular risk factors. Pulm Circ. 2014;4(4):669-678.
doi pubmed - Jonas K, Waligora M, Magon W, Zdrojewski T, Stokwiszewski J, Plazak W, Podolec P, et al. Prognostic role of traditional cardiovascular risk factors in patients with idiopathic pulmonary arterial hypertension. Arch Med Sci. 2019;15(6):1397-1406.
doi pubmed - Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiery JL. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016;37(12):942-954.
doi pubmed - Rosenkranz S, Pausch C, Coghlan JG, Huscher D, Pittrow D, Grunig E, Staehler G, et al. Risk stratification and response to therapy in patients with pulmonary arterial hypertension and comorbidities: A COMPERA analysis. J Heart Lung Transplant. 2023;42(1):102-114.
doi pubmed - Wissmuller M, Xanthouli P, Benjamin N, Grunig E, Richter MJ, Gall H, Ghofrani HA, et al. Profiles and treatment patterns of patients with pulmonary arterial hypertension on monotherapy at experienced centres. ESC Heart Fail. 2022;9(5):2873-2885.
doi pubmed - Cheng YS, Dai DZ, Ji H, Zhang Q, Dai Y. Sildenafil and FDP-Sr attenuate diabetic cardiomyopathy by suppressing abnormal expression of myocardial CASQ2, FKBP12.6, and SERCA2a in rats. Acta Pharmacol Sin. 2011;32(4):441-448.
doi pubmed - Nagendran J, Archer SL, Soliman D, Gurtu V, Moudgil R, Haromy A, St Aubin C, et al. Phosphodiesterase type 5 is highly expressed in the hypertrophied human right ventricle, and acute inhibition of phosphodiesterase type 5 improves contractility. Circulation. 2007;116(3):238-248.
doi pubmed - Denardo SJ, Wen X, Handberg EM, Bairey Merz CN, Sopko GS, Cooper-Dehoff RM, Pepine CJ. Effect of phosphodiesterase type 5 inhibition on microvascular coronary dysfunction in women: a Women's Ischemia Syndrome Evaluation (WISE) ancillary study. Clin Cardiol. 2011;34(8):483-487.
doi pubmed - Berman-Rosenzweig E, Arneson C, Klinger JR. Effects of dose and age on adverse events associated with tadalafil in the treatment of pulmonary arterial hypertension. Pulm Circ. 2014;4(1):45-52.
doi pubmed - Handoko ML, de Man FS, Allaart CP, Paulus WJ, Westerhof N, Vonk-Noordegraaf A. Perspectives on novel therapeutic strategies for right heart failure in pulmonary arterial hypertension: lessons from the left heart. Eur Respir Rev. 2010;19(115):72-82.
doi pubmed - de Man FS, Handoko ML, Guignabert C, Bogaard HJ, Vonk-Noordegraaf A. Neurohormonal axis in patients with pulmonary arterial hypertension: friend or foe? Am J Respir Crit Care Med. 2013;187(1):14-19.
doi pubmed - Emanuel R, Chichra A, Patel N, Le Jemtel TH, Jaiswal A. Neurohormonal modulation as therapeutic avenue for right ventricular dysfunction in pulmonary artery hypertension: till the dawn, waiting. Ann Transl Med. 2018;6(15):301.
doi pubmed - Scagliola R, Brunelli C, Balbi M. Treatment with neurohormonal inhibitors and prognostic outcome in pulmonary arterial hypertension with risk factors for left heart disease. World J Crit Care Med. 2022;11(2):85-91.
doi pubmed - de Man FS, Tu L, Handoko ML, Rain S, Ruiter G, Francois C, Schalij I, et al. Dysregulated renin-angiotensin-aldosterone system contributes to pulmonary arterial hypertension. Am J Respir Crit Care Med. 2012;186(8):780-789.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.