
Figure 1. Photograph of the operating room monitor demonstrating ST segment depression.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Case Report
Volume 15, Number 6, December 2024, pages 467-471
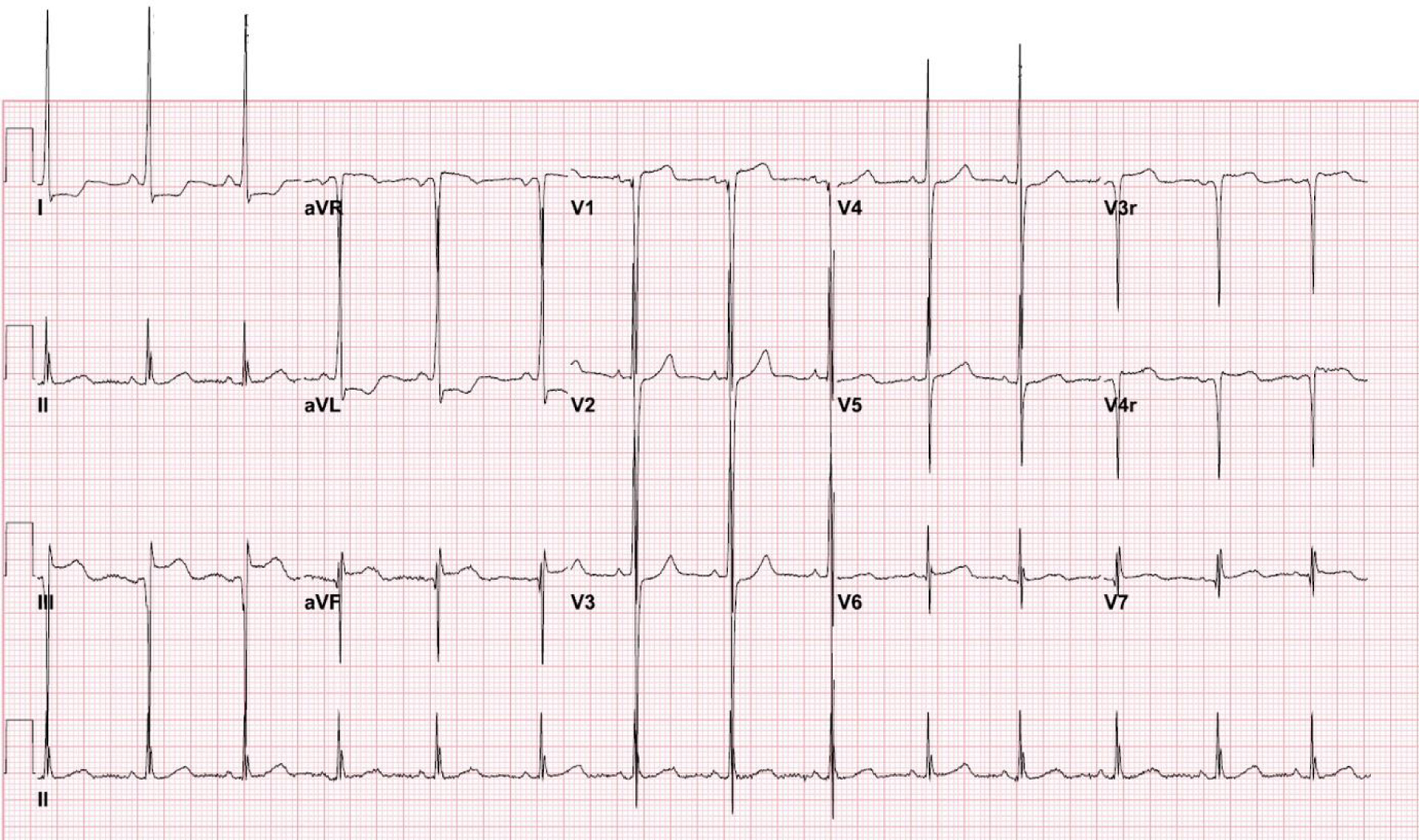
Intraoperative ST Segment Depression During General Anesthesia in a Child: Early Detection of Hypertrophic Cardiomyopathy
Figures

Table
| Authors and reference | Summary of cases and outcome |
|---|---|
| PDA: patent ductus arteriosus; TGA: transposition of the great vessels; HR: heart rate; BP: blood pressure; CHD: congenital heart disease; CPB: cardiopulmonary bypass; POD: postoperative day; ECG: electrocardiographic. | |
| Bell et al [2] | Case series of three patients including a 1-month-old, 790 g, 26-week gestation infant for PDA ligation; a 2-day-old, 3.5 kg, term infant with TGA for Senning procedure; and a 3-week-old, 4 kg, term infant with complex CHD following cardiac surgery. In the first patient, 3 mm ST segment elevations during awake laryngoscopy resolved after intubation of the trachea. A second episode of 2 mm ST segment elevation during lung compression with a decrease in oxygen saturation. In the second patient, 3 mm ST segment elevations and increased HR, BP during chest closure, treated with dopamine, isoproterenol, and nitroglycerin. The patient had a postoperative cardiac arrest and expired. In the third patient, 1 mm ST segment depression, decreased BP, heart block, and ventricular tachycardia occurred following separation from CPB. Following successful resuscitation, there was depressed myocardial function which eventually resolved with inotropic support. The patient was discharged home on POD 8 with normal myocardial function. |
| Alfirevic et al [4] | A 22-month-old, 13 kg toddler for adenoidectomy. ST segment depression with decreased BP and decreased oxygen saturation following laryngospasm. ECG changes resolved after 10 min with correction of BP and oxygen saturation. |
| Girshin et al [5] | A 4-week-old, 1.7 kg term infant with Hanhart syndrome for tracheostomy. ST segment elevation and decreased BP due to intraoperative right tension pneumothorax. ECG changes resolved with needle thoracostomy. |
| Geyer et al [11] | Case series of two patients including a 6-week-old, 5.96 kg infant scheduled for lensectomy with anterior vitrectomy and a 4-year-old boy for circumcision. In the first patient, intraoperative hypotension occurred followed by secondary ECG changes (ST segment depression and T wave inversion). With correction of BP, ECG changes disappeared. In the second patient, after anesthetic induction, ST segment depression with a biphasic T wave was noted with no change in vital signs. ECG changes reverted to baseline with a decrease in the volatile anesthetic agent. No postoperative concerns were noted in either patient. |