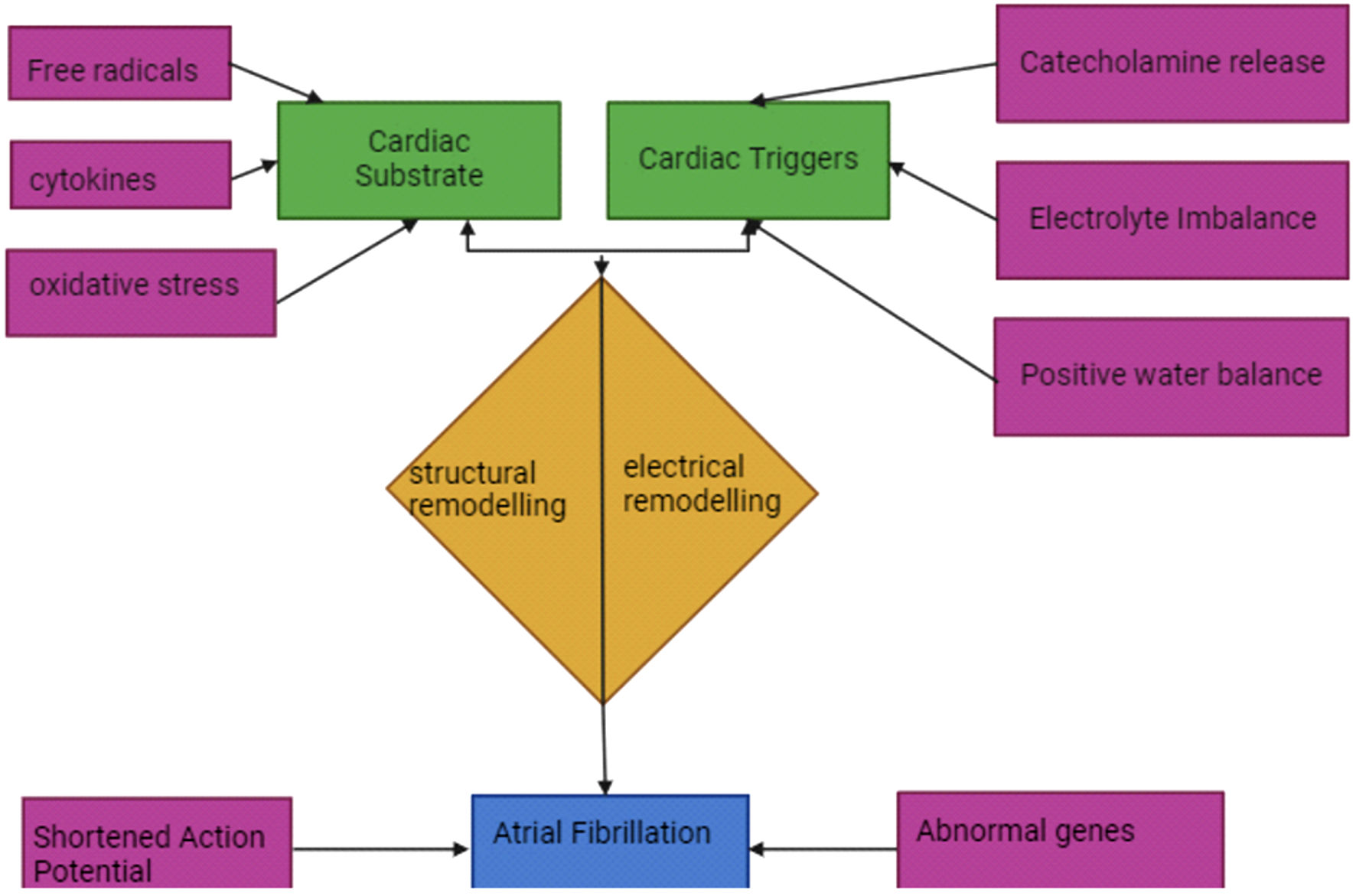
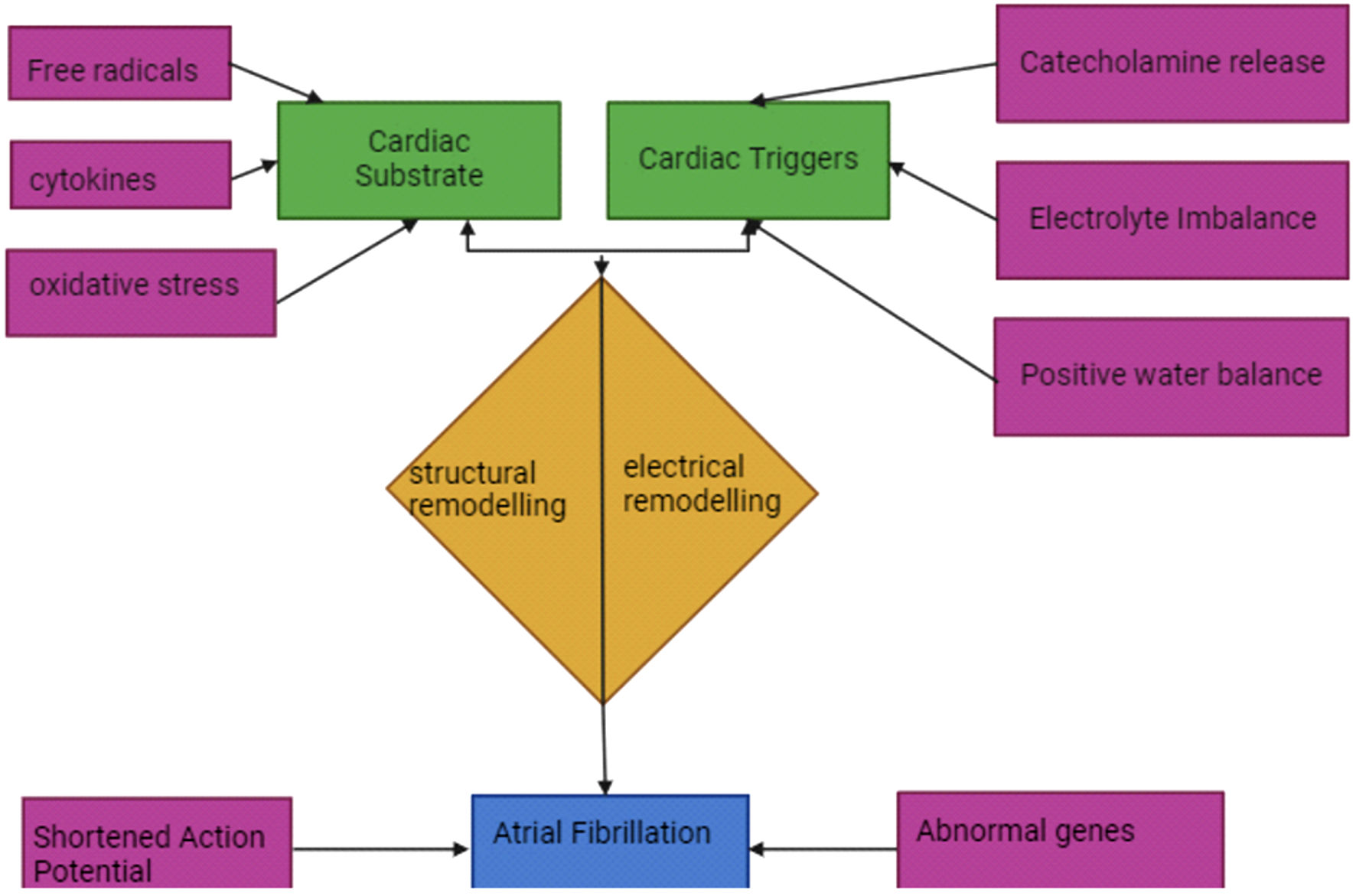
Figure 1. Proposed pathophysiology mechanisms of NOAF in sepsis. NOAF: new-onset atrial fibrillation.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Review
Volume 16, Number 1, February 2025, pages 1-14
Beyond the Beat: A Multifaceted Review of Atrial Fibrillation in Sepsis: Risk Factors, Management Strategies, and Economic Impact
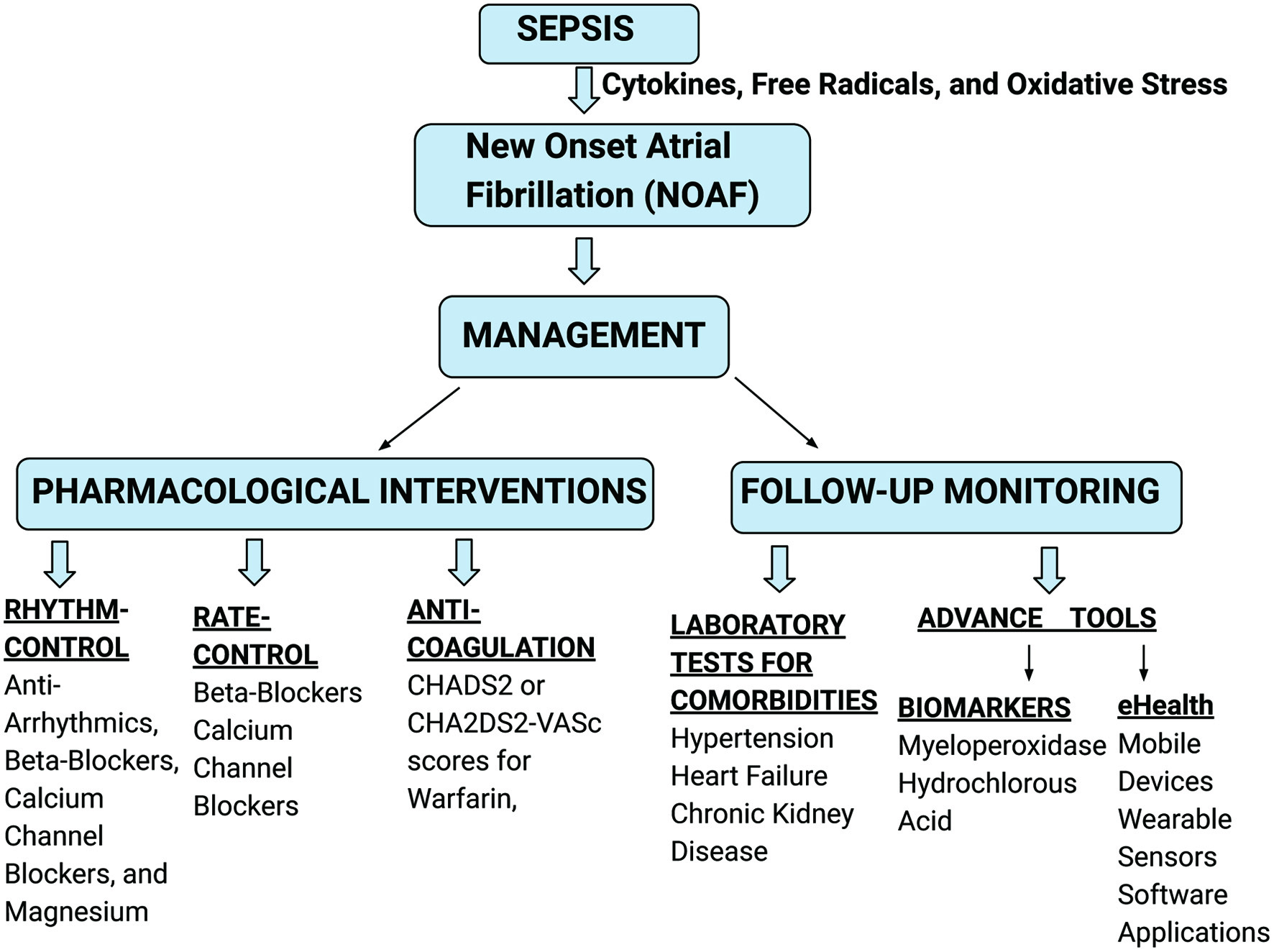
Figures
Table
| Author, year of study | Study design | Number of patients | NOAF, n (%) | Risk factor for NOAF | Outcomes |
|---|---|---|---|---|---|
| NOAF: new-onset atrial fibrillation; AF: atrial fibrillation; HTN: hypertension; CHF: congestive heart failure; CAD: coronary artery disease; MI: myocardial infarction; DM: diabetes mellitus; SAPS: simplified acute physiology score; PAD: peripheral artery disease; HLD: hyperlipidemia; MODS: multiple organ dysfunction score; CKD: chronic kidney disease; SIRS: systemic inflammatory response syndrome; LVEF: left ventricle ejection fraction; APACHE: acute physiology and chronic health evaluation; MAP: mean arterial pressure; SOFA: sequential organ failure assessment; ICU: intensive care unit; SR: sinus rhythm; RR: relative risk; OR: odds ratio; HR: hazard ratio; HLD: hyperlipidemia; PAD: peripheral arterial disease; MICU: medical intensive care unit; BP: blood pressure. | |||||
| Liu et al, 2024 [13] | Retrospective | 1,425,055 patients with sepsis | 21,327 (1.49% (95% CI: 1.47 - 1.51)) | Older age, male sex, HTN, CHF, CAD, valvular disease, mechanical ventilation, renal replacement therapy, pericarditis, myocarditis, MI, ischemic stroke, septic shock, cerebrovascular disease | In-hospital mortality: adjusted RR = 1.03 (95% CI: 1.01 - 1.06) |
| Paula et al, 2024 [14] | Retrospective | 1,357 noncardiac ICU patients | 73 (5.38) | Older age, HTN, DM, renal failure, CHF, SAPS II | Hospital mortality of chronic vs. NOAF: 31% vs. 28.8%, P = 0.779; hospital mortality AF vs. non-AF: 30.2% vs. 22.9%, P = 0.024 |
| Wetterslev et al, 2023 [27] | Prospective | 1,415 ICU patients | 13.3% (11.5 - 15.1) | HTN, paroxysmal AF, sepsis, or high disease severity at ICU admission | Adjusted cause-specific HR for 90-day mortality by AF was 1.38 (95% CI: 0.95 - 1.99) |
| Savaie et al, 2023 [29] | Retrospective | 340 noncardiac ICU patients | 44 (12.9) | Pneumonia, thyroid disease | The mortality rate of patients with NOAF was 21%. OR of the presence of NOAF and mortality (P < 0.05; OR: 2.378, CI: 1.104 - 5.16) |
| Wang et al, 2023 [15] | Retrospective | 21,538 sepsis patients | 78 (0.53), 6,759 total AF patients (31.4) | Older age, MI, CHF, HTN, HLD, PAD, cerebrovascular disease, dementia, chronic pulmonary disease, renal disease, diabetes | 28-day mortality (HR: 1.07, 95% CI: 0.99 - 1.15) |
| Fernando et al, 2020 [16] | Retrospective | 15,014 ICU patients, 1,944 sepsis patients | 1,541 (10.3), 208 sepsis patients (10.7) | Older age, higher MODS, higher comorbidities burden (CHF, PAD, HTN, COPD, DM, CKD, liver disease, malignancy, psychosis, depression) | In-hospital mortality for sepsis patients: adjusted OR = 1.28 (95% CI: 1.09 - 1.36)) |
| Steinberg et al, 2019 [28] | Prospective | 27 septic shock patients | 9 (33.3) | High SOFA score | Overall mortality AF vs. SR: 66.7% vs. 11.1%, P = 0.024 |
| Desai et al, 2019 [17] | Retrospective | 5,808,166 sepsis patients | 1,126,433 (19.4) | Older age, White race, male sex, cardiovascular disease, pulmonary disease, diabetes, hypothyroidism, cerebrovascular disease, renal failure, fluid and electrolyte disorders | All-cause mortality rate for AF vs. non-AF with sepsis: 18.4% and 11.9%, P = 0.001 |
| Makrygiannis et al, 2018 [18] | Prospective | 133 noncardiac ICU patients | 20 (15) | Age > 65, arterial HTN, SIRS, sepsis, left atrial dilatation, diastolic dysfunction | NOAF is not an independent predictor of ICU mortality. Sepsis and age > 65 years were statistically significant an independent predictor of ICU mortality. |
| Launey et al, 2019 [30] | Prospective | 261 patients with septic shock | 57 (22) | Lower risk with low dose hydrocortisone | ICU mortality in hydrocortisone group vs. non-hydrocortisone group: 37% vs. 24% (P = 0.018). 28-day mortality in hydrocortisone group vs. non-hydrocortisone group: 38% vs. 26% (P = 0.036) |
| Moss et al, 2017 [19] | Retrospective | 8,356 ICU patients | 749 (8.96) | Older age, acute respiratory failure, sepsis | Hospital mortality: OR = 1.63, 95% CI: 1.01 - 2.63 |
| Liu et al, 2016 [31] | Retrospective | 503 sepsis patients | 240 (47.7) | Older age, LVEF < 45%, HTN, CHF, CAD, cerebrovascular disease | Failure of restored SR was independently associated with increased in-hospital mortality in patients with sepsis and NOAF. |
| Guenancia et al, 2015 [20] | Prospective | 66 patients with septic shock | 29 (43.9) | Older age, LVEF < 45% | ICU mortality rate in septic shock patients with and without new-onset AF was 24% vs. 19%, P = 0.61. Mortality did not differ between these two groups at 28 days (22% vs. 28%, NOAF vs. SR respectively, P = 0.58) and at 90 days (41% vs. 43% respectively, P = 0.88). |
| Shaver et al, 2015 [10] | Prospective | 1,770 ICU patients | 123 (7), 13% of sepsis patients, 10% of patients without sepsis | Older age, shock, hypotension, advanced organ failure, positive fluid balance, antecedent vasopressor use, increased left atrial dimension, more diastolic dysfunction, mitral regurgitation | OR for death in sepsis patients with any AF: 1.29 (0.85 - 1.94), P = 0.228 |
| Wells et al, 2011 [21] | Retrospective | 465 MICU patients with sepsis/septic shock | 132 | Older age, CAD, White race | Sepsis + NOAF is 5.7 times more likely to die compared to the Neither group. |
| Chen et al, 2015 [22] | Retrospective | 741 MICU patients | 53 (7.15) | Older age, APACHE II score, systolic BP, MAP, heart rate | In-hospital mortality: adjusted OR = 2.21, 95% CI: 1.07 - 4.54, P = 0.032 |
| Walkey et al, 2014 [23] | Retrospective | 138,722 sepsis patients | 9,540 (6.9) | Older age, male sex, White race, comorbid conditions (chronic lung disease, heart failure, ischemic heart disease, valvular heart disease), acute organ failure | Greater 5-year risks of hospitalization for heart failure compared NOAF vs. control group (11.2% vs 8.2%). Multivariable-adjusted HR: 1.25, 95% CI: 1.16 - 1.34. Ischemic stroke (5.3% vs. 4.7%; HR: 1.22, 95% CI: 1.10 - 1.36). Death (74.8% vs. 72.1%; HR: 1.04, 95% CI: 1.01 - 1.07). |
| Walkey et al, 2013 [24] | Retrospective | 60,209 sepsis patients | 4,320 (7.2) | Older age, White race, acute organ dysfunction, ICU admission, mechanical ventilation, right heart catheterization, diagnosis of endocarditis, and coronary artery bypass graft surgery. | |
| Walkey et al, 2011 [25] | Retrospective | 49,082 sepsis patients | 2,896 (5.9) | Older age, obesity, CHF, metastatic/hematologic malignancy, prior stroke, organ dysfunction, respiratory, abdominal, skin or soft tissue infection, bacteremia | In-hospital mortality: RR = 1.13 (95% CI: 1.08 - 1.19) |
| Meierhenrich et al, 2010 [26] | Prospective | 629 noncardiac ICU patients → 64 septic shock patients | 49 in ICU patients → 23 in septic shock patients | Older age, arterial HTN, higher SOFA | ICU mortality in septic shock patients with new-onset AF was 10/23 (44%) compared with patient that had SR: 6/27 (22%) (P = 0.14). The median length of ICU stay among surviving patients was longer in patients with new-onset AF compared to those with maintained SR (30 vs. 17 days, P = 0.017). Failure to restore SR was associated with increased ICU mortality (71.4% vs. 21.4%, P = 0.015). |