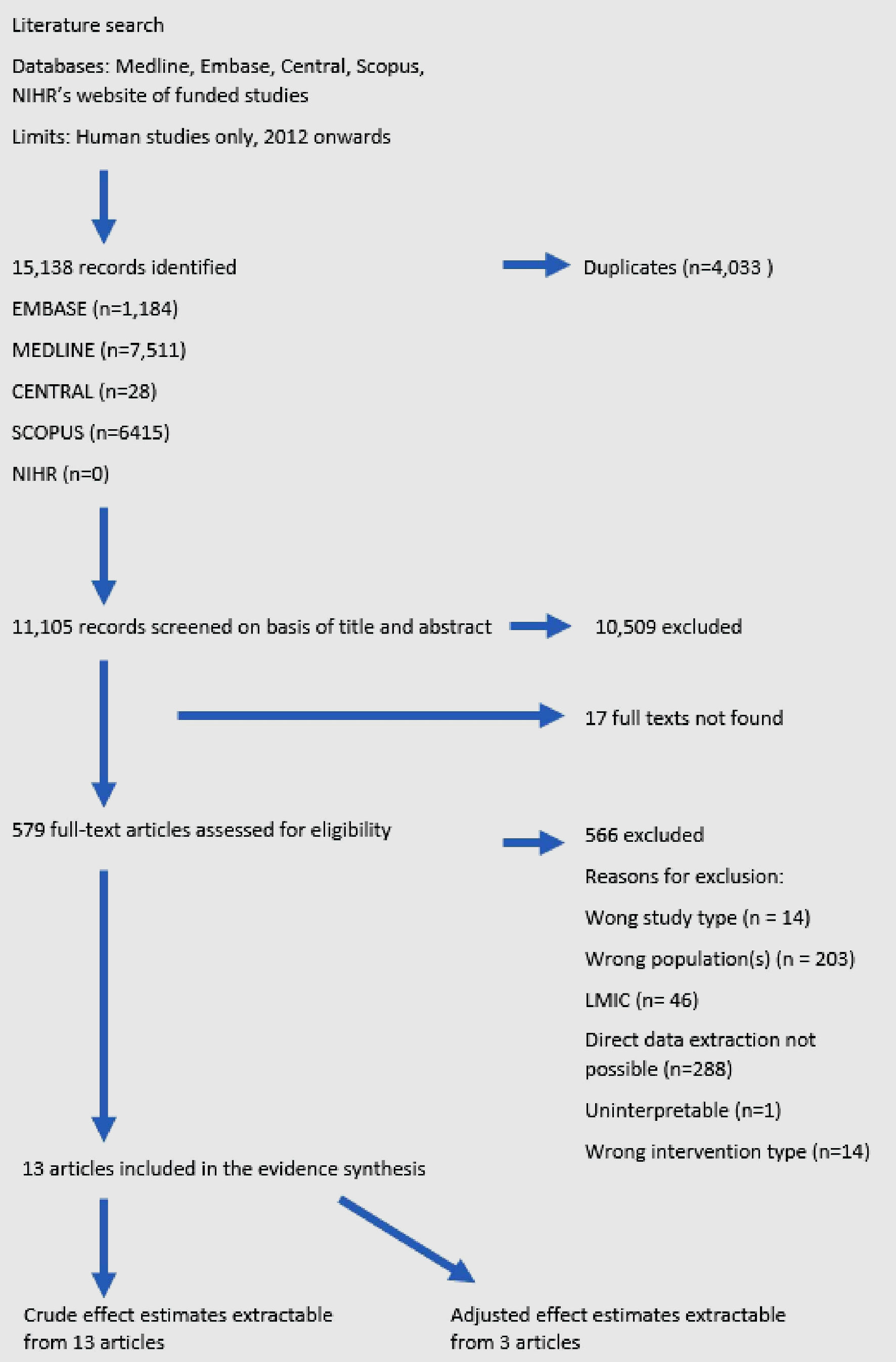
Figure 1. Flowchart of study selection.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 15, Number 6, December 2024, pages 425-438
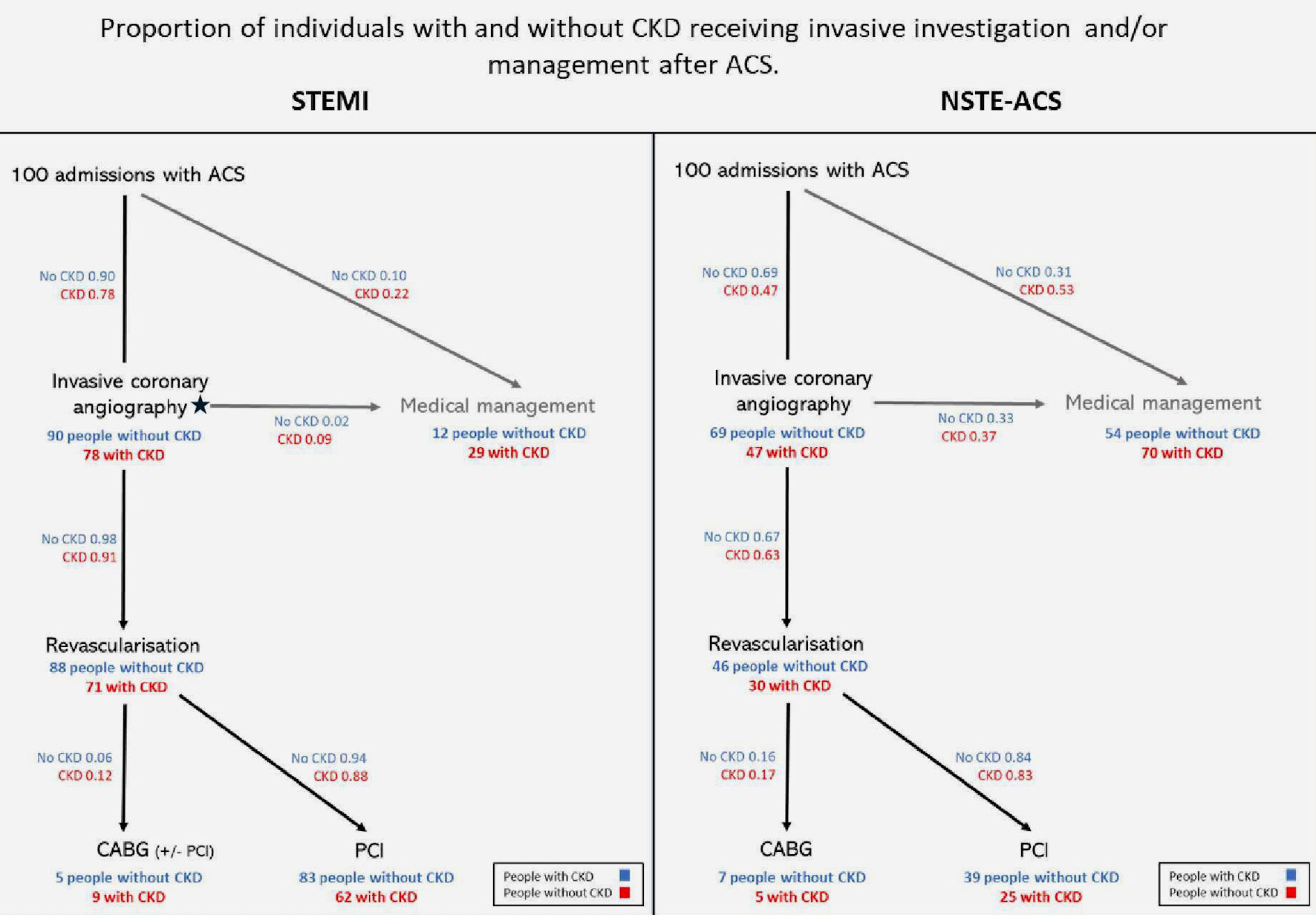
Does Chronic Kidney Disease Influence Revascularization Strategy After Acute Coronary Syndrome? A Systematic Review and Meta-Analysis
Figures
Tables
| Study design, country | Hospital PCI capability | N | Dates | Definition of impaired CKD function | Definition of control group | ACS type(s) | Age range | Crude figures | Effect estimates, OR (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|
| PCI: percutaneous coronary intervention; ACS: acute coronary syndrome; CKD: chronic kidney disease; eGFR: estimated glomerular filtration rate; ICD: international classification of diseases; NSTE-ACS: non-ST-elevation acute coronary syndrome; NSTEMI; non-ST-elevation myocardial infarction; OR: odds ratio; CI: confidence interval; STEMI: ST-elevation myocardial infarction; UA: unstable angina; PD: peritoneal dialysis; HD: hemodialysis; ESRD: end-stage renal disease; ICD-9 CM: International Classification of Diseases, Ninth Revision, Clinical Modification. | ||||||||||
| Alushi et al, 2021 [29] | Prospective, Germany | All | 438 | 2012 - 2017 | eGFR < 30 or dialysis duration > 30days at the time of MI | eGFR > 90 | NSTEMI, UA | Not specified | NSTE-ACS 25/222 CKD vs. 18/216 non-CKD | Crude OR NSTE-ACS 1.36 (0.75 - 2.46) |
| Adjusted OR NSTE-ACS 3.20 (1.28 - 8.00) | ||||||||||
| Bagai et al, 2018 [7] | Retrospective, USA | All | 615,425 | 2007 - 2015 | eGFR < 60 | eGFR ≥ 60 | NSTEMI, STEMI | Not specified | All ACS 21,191/171,140 CKD vs. 49,707/444,285 non-CKD | Crude OR all ACS 1.12 (1.10 - 1.14) |
| NSTE-ACS 16,344/91,021 CKD vs. 37,087/216,244 non-CKD | Crude OR NSTE-ACS 1.12 (1.10 - 1.14) | |||||||||
| STEMI 4,847/80,119 CKD vs. 37,087/228,041 non-CKD | Crude OR STEMI 1.10 (1.06 - 1.14) | |||||||||
| Blicher et al, 2013 [28] | Retrospective, Denmark | Mixed | 34,722 | 2000 - 2009 | Code for CKD/dialysis [4] | No CKD code [5] | NSTEMI, STEMI [2] | > 25 years | All MI 239/904 CKD vs. 6,337/33,818 non-CKD | Crude OR all ACS 1.56 (1.34 - 1.81) |
| Kawsara et al, 2022 [33] | Retrospective, USA | Mixed | 69,281 | 2016 - 2019 | Dialysis code | No dialysis code | STEMI | ≥ 18 years | STEMI 37/522 CKD vs. 3,438/68,759 non-CKD | Crude OR STEMI 1.45 (1.04 - 2.03) |
| Khan et al, 2020 [34] | Retrospective, USA | Mixed | 149,983 | 2012 - 2017 | ICD-9 CM code for ESRD | Other | STEMI | ≥ 18 years | STEMI 251/1,753 CKD vs. 63,675/12,735/148,230 non-CKD | STEMI OR 1.78 (1.55 - 1.03) |
| Kotwal et al, 2017 [35] | Retrospective, Australia | Mixed | 12,662 | 2004 - 2008 | ICD-10 code for CKD | No CKD code | NSTEMI, STEMI | ≥ 18 years | All ACS 272/811 CKD vs. 1,741/11,851 non-CKD | All ACS OR 2.93 (2.51 - 3.42) |
| Lin et al, 2022 [13] | Retrospective, Taiwan | Mixed | 67,534 | 2001 - 2013 | Code for CKD/dialysis | No code for CKD or dialysis | NSTEMI, STEMI | ≥ 20 years | All ACS 2,433/16,477 CKD vs. 4,894/51,057 non-CKD | All ACS OR 1.62 (1.55 - 1.72) |
| Murray et al, 2018 [36] | Retrospective, USA | Mixed | 236,284 | 2001 - 2012 | ICD-9 code for CKD1-5 or dialysis | No code for CKD or dialysis | NSTEMI | ≥ 18 years | NSTE-ACS 7,227/22,891 CKD vs. 47,517/208,293 non-CKD | NSTE-ACS OR 1.18 (1.14 - 1.21) |
| Panchal et al, 2021 [37] | Retrospective, USA | Mixed | 87,883 | 2012 - 2014 | ICD-9 code for CKD1 - 5, unspecified CKD, or dialysis | No code for CKD or dialysis | STEMI | Not specified | STEMI 838/7,476 CKD vs. 5,734/80,407 non-CKD | STEMI OR 1.67 (1.55 - 1.81) |
| Sakhuja et al, 2016 [38] | Retrospective, USA | Mixed | 141,838 | 2006 - 2010 | ICD-9 code for ESRD or OPCS codes for PD or HD, without a code for CKD | No ESRD/PD/HD code | STEMI | ≥ 20 years | STEMI 292/1,248 CKD vs. 13,746/140,590 non-CKD | STEMI OR 1.67 (1.43 - 1.95) |
| Sanchis et al, 2021 [32] | Retrospective, Spain | Not specified | 7,211 (total study size) | 2002 - 2017 | eGFR < 60 calculated from admission creatinine | Admission eGFR ≥ 60 | NSTEMI, UA | ≥ 70 years | Crude figures not available | Crude OR NSTE-ACS 0.85 (0.70 - 1.03) |
| Adjusted OR NSTE-ACS 1.11 (0.92 - 1.35) | ||||||||||
| Shaw et al, 2014 [6] | Retrospective, England & Wales | Mixed | 9,732 | 2008 - 2010 | eGFR < 60 calculated from admission creatinine | Admission eGFR ≥ 60 | NSTEMI, UA | Not specified | NSTE-ACS 274/2,318 CKD vs. 679/7,414 non-CKD | Crude OR NSTE-ACS 1.32 (1.15 - 1.54) |
| Smilowitz et al, 2017 [19] | Retrospective, USA | Mixed | 388,592 | 2007 - 2012 | ICD9 codes for CKD3 - 5 or HD | No code for CKD3 - 5 or HD | NSTEMI, STEMI | Not specified | All ACS 9,775/43,242 CKD vs. 55,389/345,350 non-CKD | Crude OR all ACS 1.53 (1.49 - 1.57) |
| NSTE-ACS 7,783/30,657 CKD vs. 38,324/175,921 non-CKD | Adjusted OR all ACS 1.06 (1.03 - 1.09) | |||||||||
| STEMI 1,992/12,585 vs. 17,065/169,429 non-CKD | Crude OR NSTE-ACS 1.22 (1.19 - 1.26) | |||||||||
| Adjusted OR NSTE-ACS 1.02 (0.99 - 1.06) | ||||||||||
| Crude OR STEMI 1.69 (1.60 - 1.77) | ||||||||||
| Adjusted OR STEMI 1.21 (1.14 - 1.28) | ||||||||||
| Finding | No. of studies | No. of participants | Average exposure effect (OR (95% CI)) | Certainty of evidence |
|---|---|---|---|---|
| ACS: acute coronary syndrome; CABG: coronary artery bypass graft; CKD: chronic kidney disease; NSTE-ACS: non-ST-elevation acute coronary syndrome; OR: odds ratio; CI: confidence interval; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction. | ||||
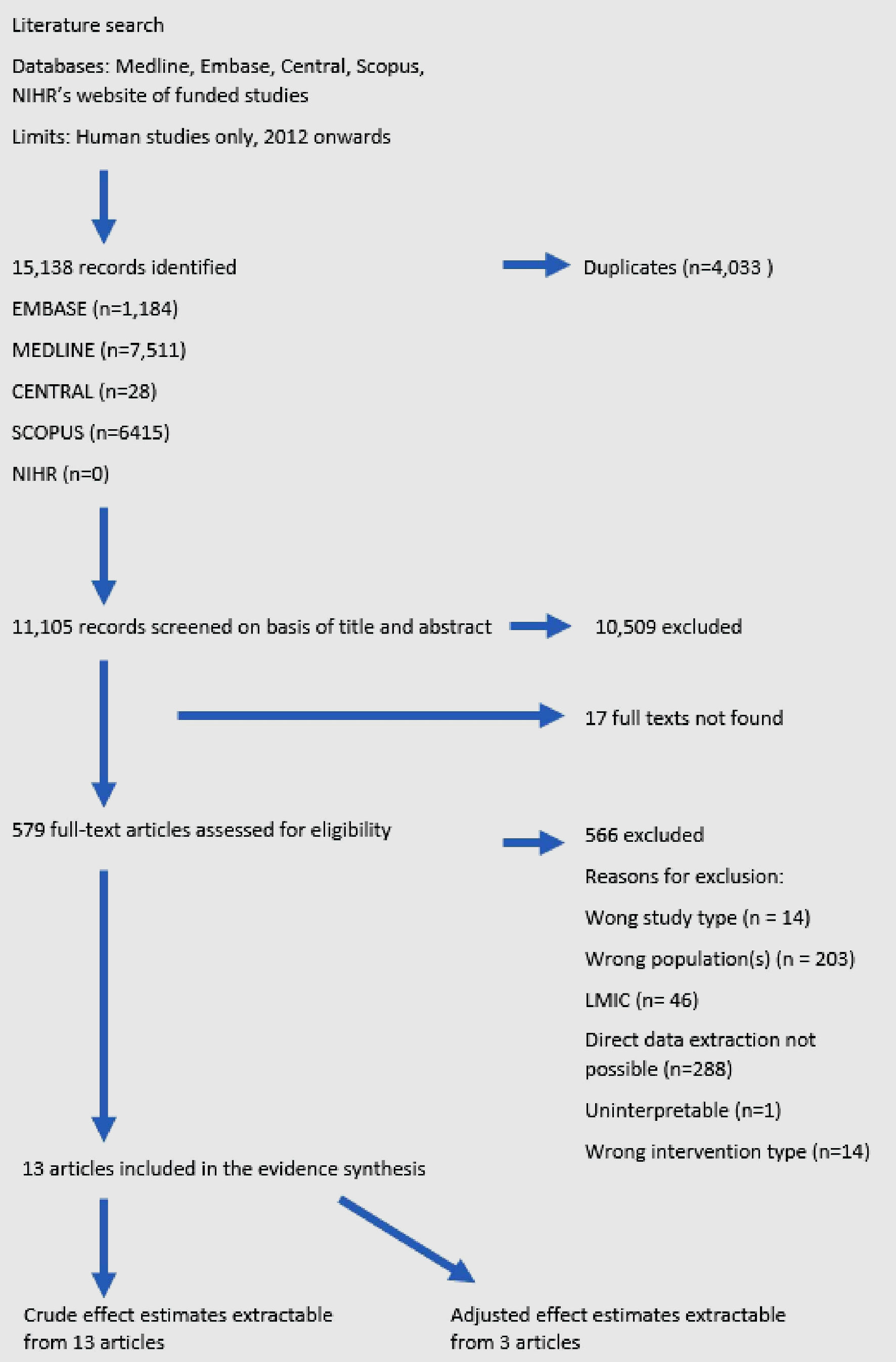
| CKD is associated with increased odds of receipt of CABG vs. PCI amongst people revascularized following ACS. | 13 | 1,682,207 | 1.50 (1.30 - 1.72) | Moderate |
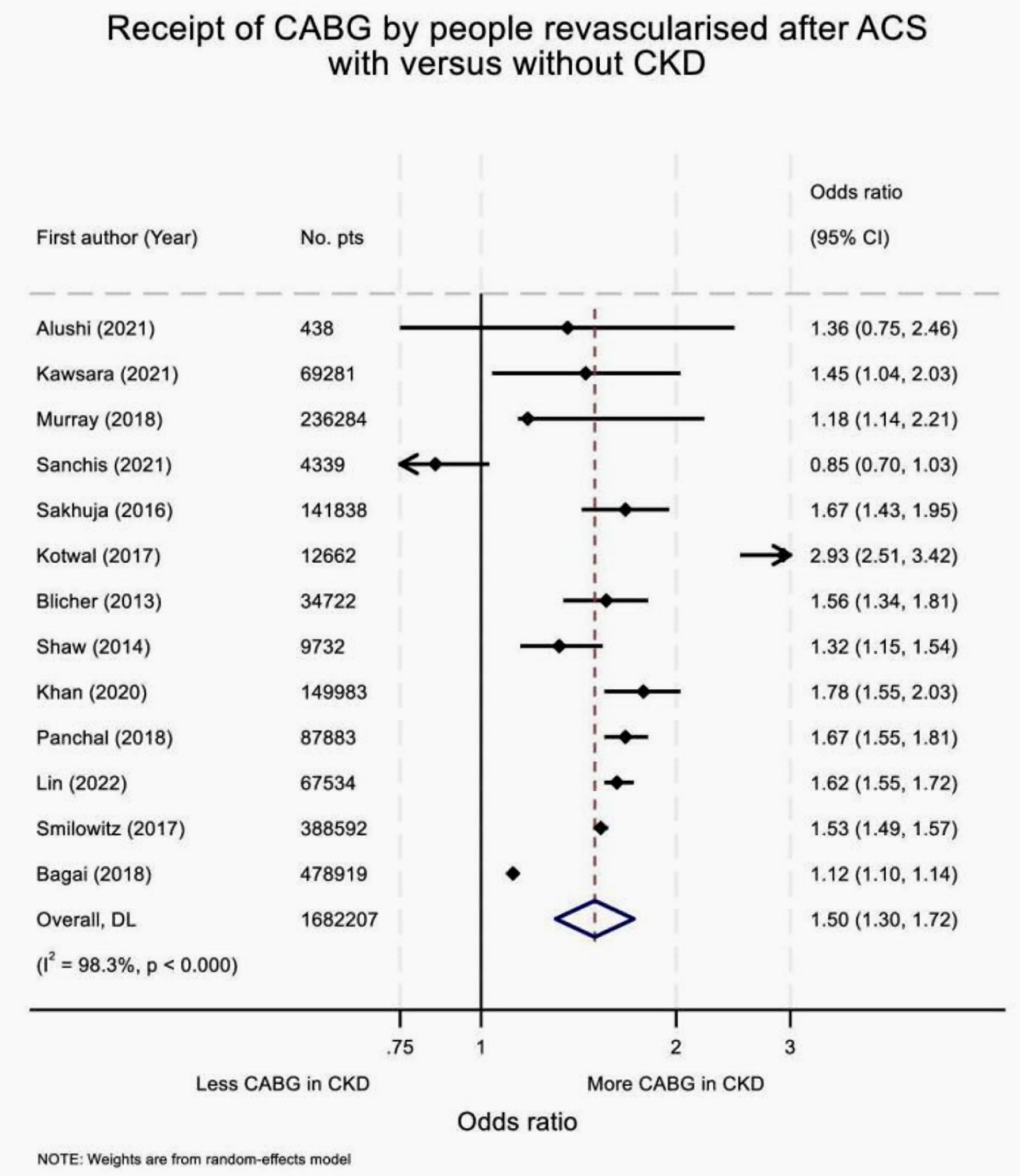
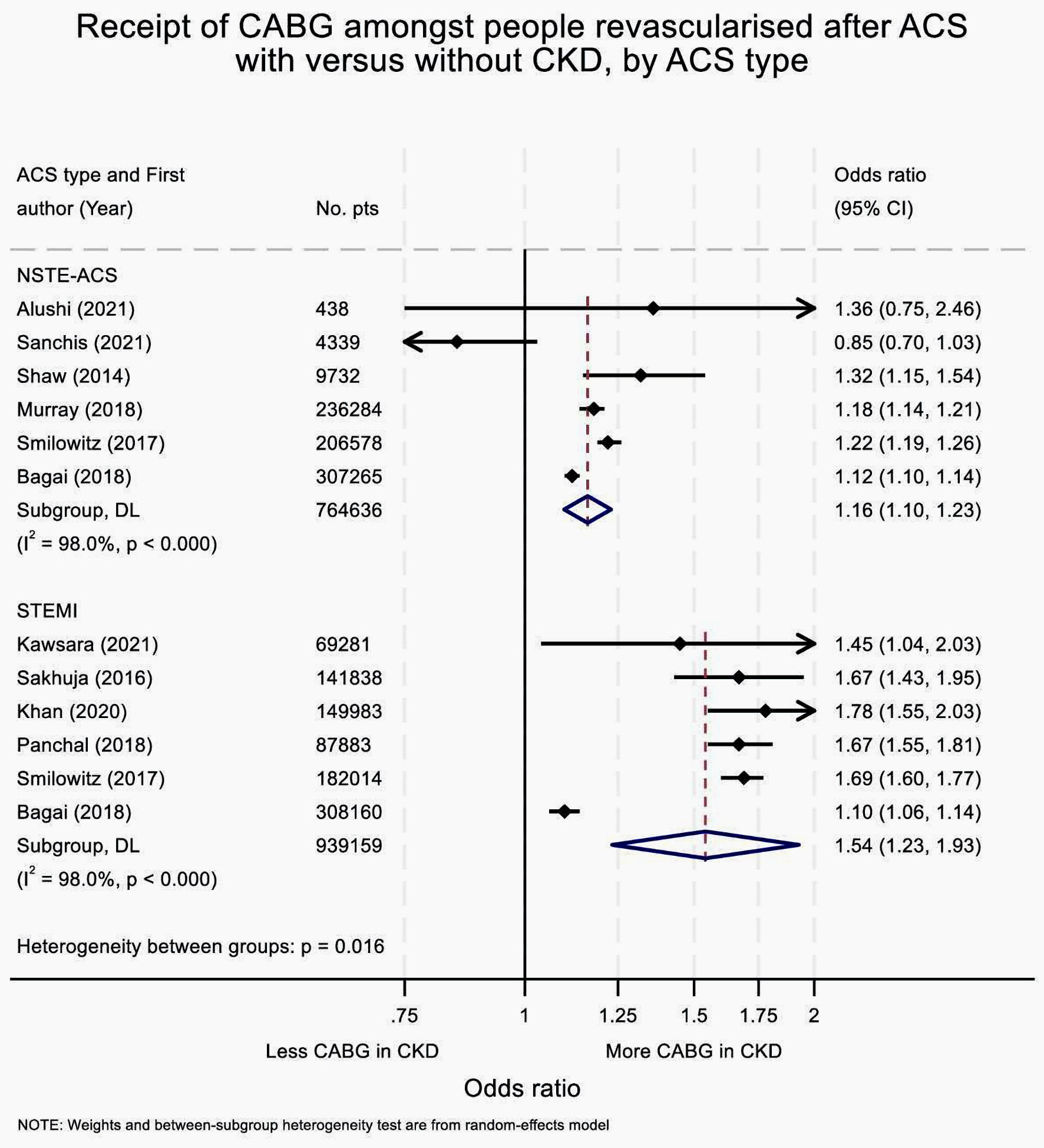
| CKD is associated with increased odds of receipt of CABG vs. PCI amongst people revascularized following NSTE-ACS. | 6 | 764,636 | 1.16 (1.10 - 1.23) | Moderate |
| CKD is associated with increased odds of receipt of CABG vs. PCI amongst people revascularized following STEMI. | 6 | 939,159 | 1.54 (1.23 - 1.93) | Moderate |
| CKD is associated with increased odds of receipt of CABG vs. PCI amongst people revascularized following ACS in people who do not receive dialysis. | 5 | 1,020,773 | 1.44 (1.20 - 1.71) | Low |
| CKD is associated with increased odds of receipt of CABG vs. PCI amongst people revascularized following ACS in people who receive dialysis. | 5 | 838,935 | 1.25 (1.12 - 1.40) | Moderate |