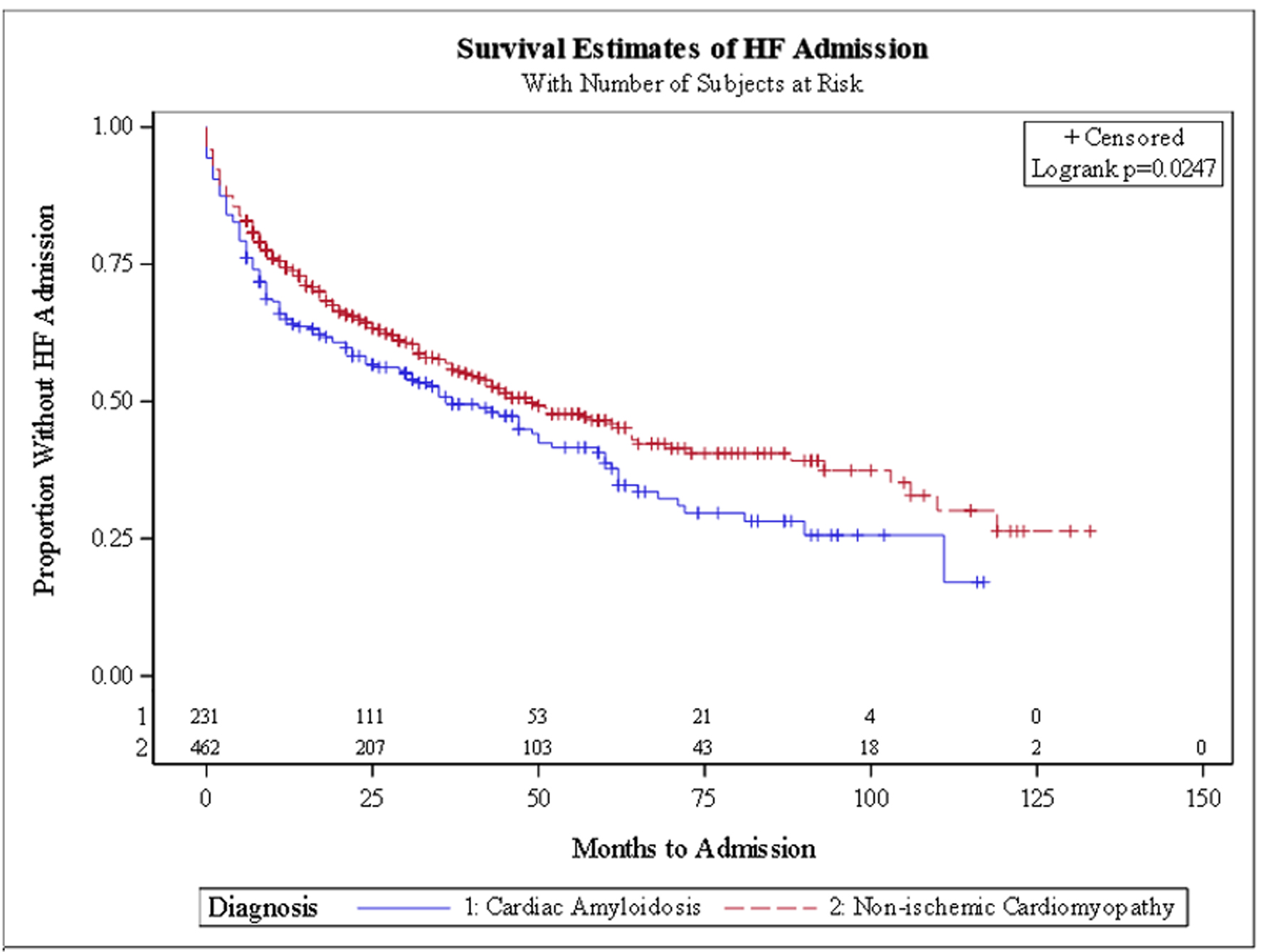
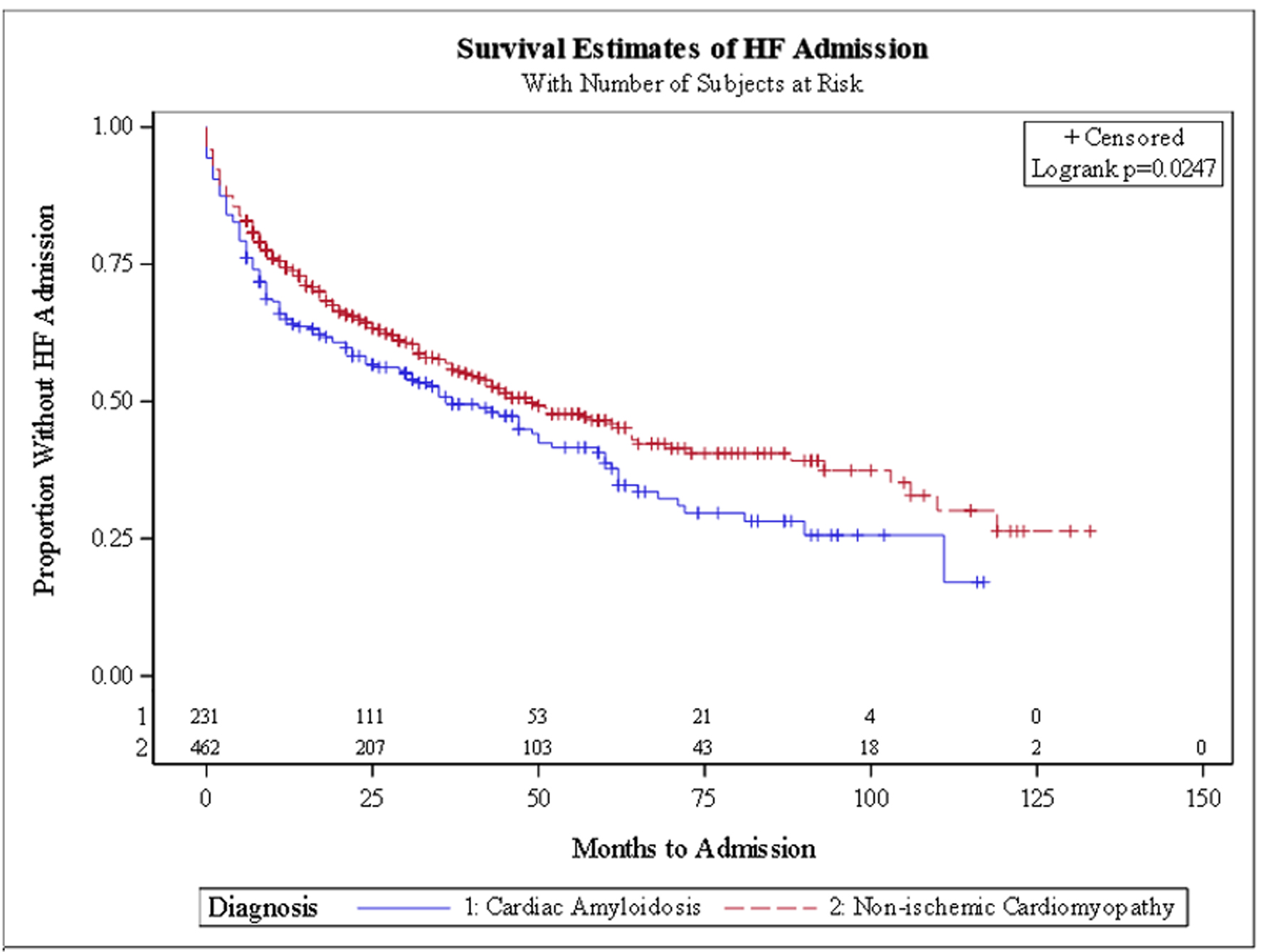
Figure 1. Kaplan-Meier curve for heart failure hospitalization.
| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 16, Number 2, April 2025, pages 102-109
Long-Term Clinical Outcomes in Patients With Transthyretin Cardiac Amyloidosis Versus Non-Ischemic Cardiomyopathy
Figures
Tables
| Characteristics | Cardiac amyloidosis (n = 231) | Non-ischemic cardiomyopathy (n = 462) | P-value |
|---|---|---|---|
| *P values < 0.05. SD: standard deviation. | |||
| Demographics | |||
| Age, mean (SD) | 73.4 (11.8) | 73.1 (11.8) | - |
| Race/ethnicity, n (%) | |||
| White | 172 (74.5%) | 344 (74.5%) | - |
| Black | 50 (21.6%) | 100 (21.6%) | - |
| Other | 9 (3.9%) | 18 (3.9%) | - |
| Male, n (%) | 117 (50.6%) | 234 (50.6%) | - |
| Baseline clinical comorbidities | |||
| Smoker, n (%) | 30.5 (48.9%) | 30.6 (44.2%) | 0.39 |
| Diabetes, n (%) | 80 (34.6%) | 175 (37.9%) | 0.17 |
| Hypertension, n (%) | 88 (38.1%) | 151 (32.7%) | 0.06 |
| Dyslipidemia, n (%) | 181 (78.4%) | 332 (71.9%) | < 0.0001 |
| Sleep apnea, n (%) | 116 (50.2%) | 159 (34.4%) | 0.11 |
| Atrial fibrillation, n (%) | 57 (24.7%) | 89 (19.3%) | 0.001* |
| Implantable defibrillator, n (%) | 61 (26.4%) | 180 (39.0%) | - |
| Pacemaker, n (%) | 0 | 42 (9.1%) | 0.001* |
| History of stroke, n (%) | 10 (4.3%) | 60 (13.0%) | 0.06 |
| History of myocardial infarction, n (%) | 82 (35.5%) | 132 (28.6%) | 0.04* |
| Coronary artery disease, n (%) | 24 (10.4%) | 28 (6.1%) | 0.001* |
| Peripheral vascular disease, n (%) | 112 (48.5%) | 164 (35.5%) | 0.02* |
| Chronic lung disease, n (%) | 44 (19.0%) | 57 (12.3%) | 0.32 |
| Chronic kidney disease, n (%) | 66 (28.6%) | 116 (25.1%) | 0.20 |
| CA (n = 231) | NICM (n = 462) | P-value | |
|---|---|---|---|
| *P values < 0.05. ACE: angiotensin-converting enzyme; BNP: B-type natriuretic peptide; CA: cardiac amyloidosis; IQR: interquartile range; NICM: non-ischemic cardiomyopathy. | |||
| Labs | |||
| BNP (median, IQR) | 453 (232 - 1,135) | 376 (173 - 930) | 0.06 |
| Creatinine (median, IQR) | 1.20 (0.86 - 1.74) | 1.09 (0.90 - 1.50) | 0.07 |
| Hemoglobin (median, IQR) | 12.5 (11.0 - 13.6) | 12.6 (11.1 - 14.1) | 0.02* |
| Troponin (median, IQR) | 0.03 (0.015 - 0.11) | 0.03 (0.02 - 0.07) | 0.56 |
| Cardiac medications, n (%) | |||
| Anti-coagulant | 87 (37.7%) | 208 (45.0%) | 0.07 |
| Anti-platelet | 68 (29.4%) | 141 (30.5%) | 0.77 |
| Aspirin | 155 (67.1%) | 305 (66.0%) | 0.77 |
| ACE inhibitor | 62 (26.8%) | 92 (19.9%) | 0.04* |
| Angiotensin receptor blocker | 175 (75.8%) | 287 (62.1%) | 0.0003* |
| Beta-blocker | 197 (85.3%) | 394 (85.3%) | 1.0 |
| Class I anti-arrhythmic | 3 (1.3%) | 14 (3.0%) | 0.17 |
| Class III anti-arrhythmic | 37 (16.0%) | 97 (21.0%) | 0.12 |
| Calcium channel blocker | 143 (61.9%) | 206 (44.6%) | < 0.001* |
| Diuretic | 191 (82.7%) | 345 (74.7%) | 0.02* |
| Statin | 173 (74.9%) | 278 (60.2%) | < 0.001* |
| CA (n = 231) | NICM (n = 462) | P-value | |
|---|---|---|---|
| *P values < 0.05. CA: cardiac amyloidosis; NICM: non-ischemic cardiomyopathy. | |||
| Heart failure hospitalization | 133 (57.6%) | 213 (46.1%) | 0.005* |
| Right bundle branch block | 23 (10.3%) | 15 (3.3%) | < 0.001* |
| Left bundle branch block | 8 (3.5%) | 33 (7.6%) | 0.08 |
| Second-degree heart block | 2 (0.9%) | 5 (1.1%) | 0.79 |
| Third-degree heart block | 11 (4.8%) | 15 (3.4%) | 0.41 |
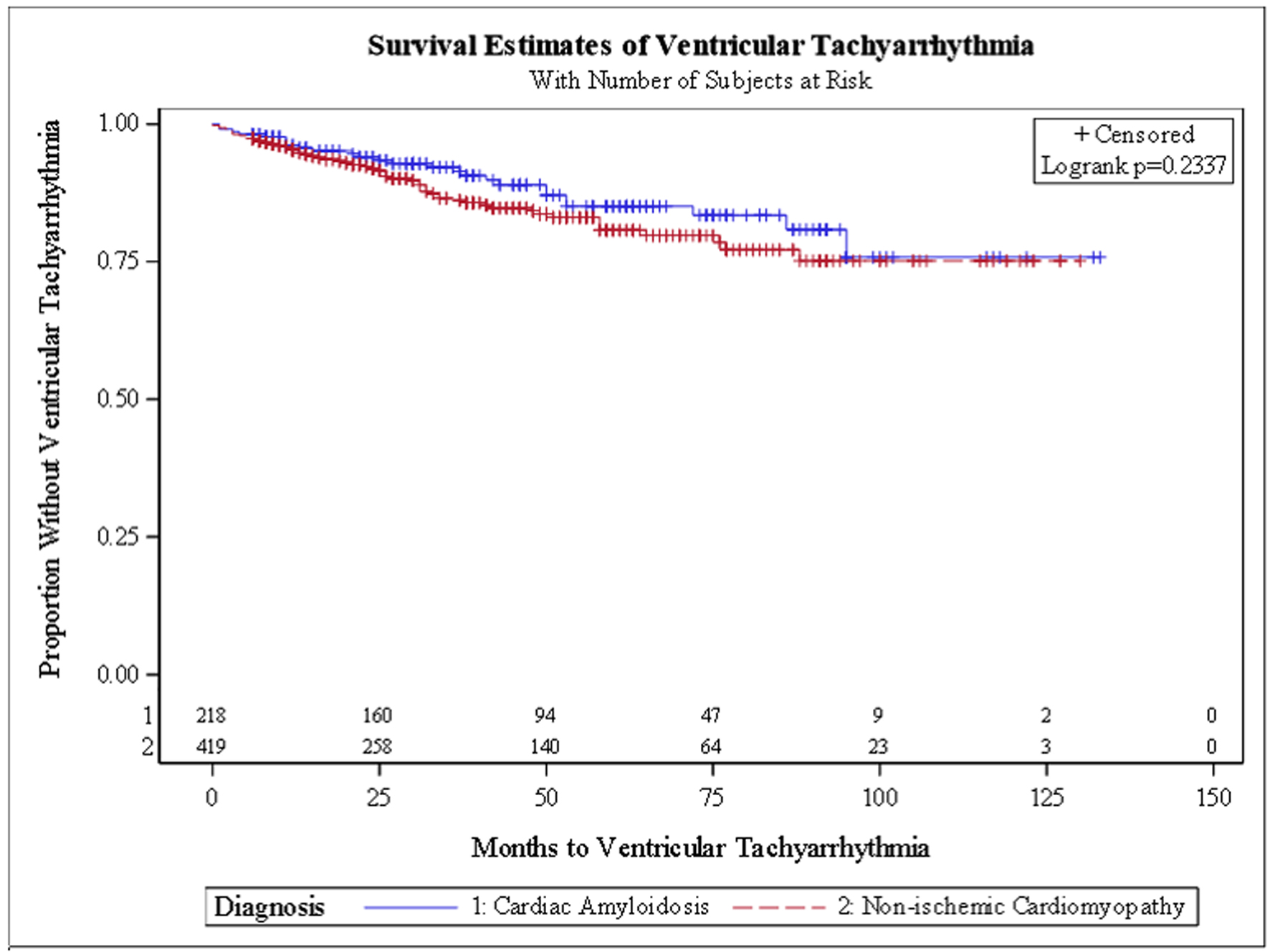
| Ventricular tachyarrhythmias | 26 (11.9%) | 58 (13.8%) | 0.53 |
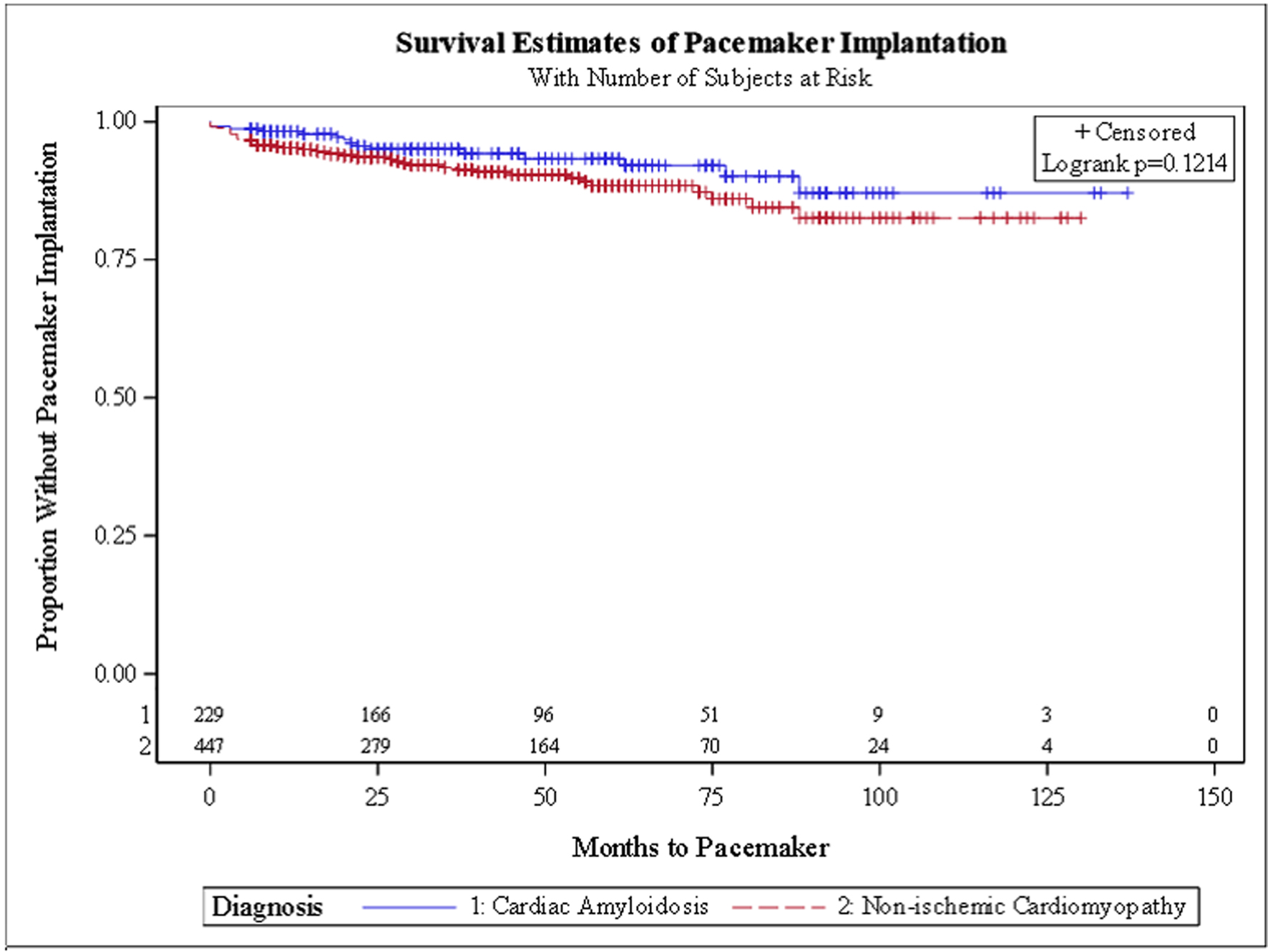
| Pacemaker | 15 (6.6%) | 42 (9.4%) | 0.19 |
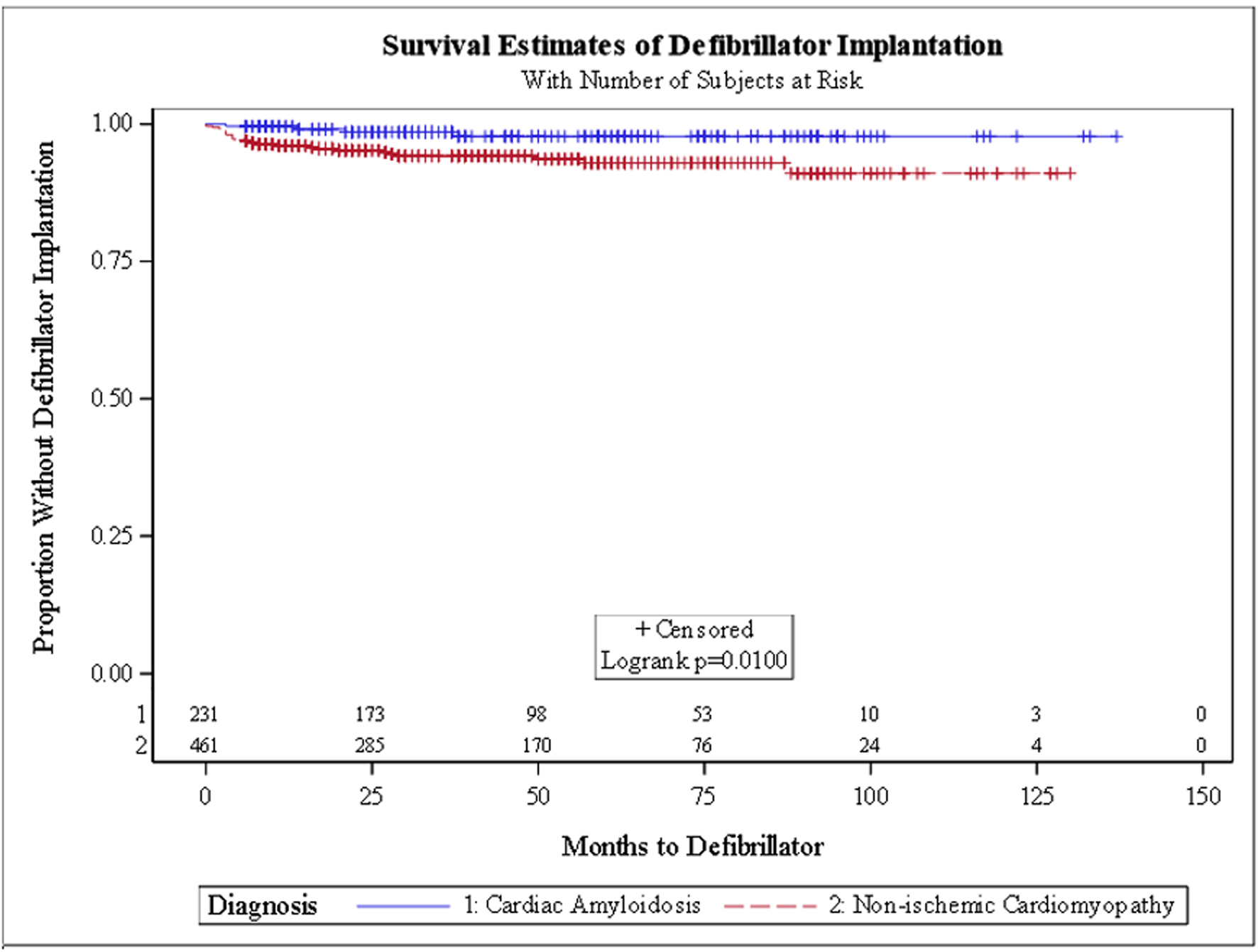
| Defibrillator | 4 (1.7%) | 27 (5.9%) | 0.02* |
| Characteristics | HFH, OR (95% CI) | Defibrillator, OR (95% CI) | Pacemaker, OR (95% CI) | Ventricular tachyarrhythmias, OR (95% CI) |
|---|---|---|---|---|
| *Statistically significant (confidence interval does not include 1). CA: cardiac amyloidosis; CI: confidence interval; HFH: heart failure hospitalization; NICM: non-ischemic cardiomyopathy; OR: odds ratio. | ||||
| CA vs. NICM | 1.86 (1.29 - 2.68)* | 0.06 (0.01 - 0.64)* | 0.64 (0.24 - 1.68) | 0.78 (0.44 - 1.40) |
| Smoker | 1.54 (0.99 - 2.39) | 0.22 (0.02 - 2.19) | 0.24 (0.07 - 0.83)* | 1.93 (0.93 - 4.01) |
| Diabetes | 0.94 (0.61 - 1.46) | 11.36 (1.48 - 87.31) | 1.24 (0.40 - 3.90) | 0.99 (0.50 - 1.94) |
| Hypertension | 1.06 (0.64 - 1.75) | 1.03 (0.16 - 6.76) | 0.91 (0.30 - 2.73) | 0.80 (0.37 - 1.73) |
| Dyslipidemia | 0.89 (0.59 - 1.36) | 8.29 (1.26 - 54.58) | 2.23 (0.79 - 6.32) | 0.89 (0.46 - 1.69) |
| Sleep apnea | 0.71 (0.44 - 1.14) | 0.02 (0.00 - 0.30)* | 0.21 (0.07 - 0.65)* | 1.04 (0.50 - 2.15) |
| Atrial fibrillation | 1.84 (1.19 - 2.85) | 0.65 (0.09 - 4.68) | 2.25 (0.91 - 5.61) | 0.83 (0.41 - 1.66) |
| Implantable defibrillator | 1.18 (0.62 - 2.24) | 5.98 (0.37 - 96.21) | - | 0.52 (0.18 - 1.47) |
| Pacemaker | 0.79 (0.37 - 1.68) | - | 5.41 (0.75 - 38.80) | 0.74 (0.19 - 2.90) |
| History of stroke | 1.05 (0.48 - 2.32) | 37.5 (0.95 - 1,485.6) | 4.33 (0.69 - 27.16) | 1.22 (0.34 - 4.44) |
| Myocardial infarction | 0.95 (0.48 - 1.89) | 0.59 (0.11 - 3.31) | 0.26 (0.04 - 1.71) | 1.20 (0.35 - 4.13) |
| Coronary artery disease | 1.10 (0.64 - 1.88) | 0.13 (0.01 - 1.91) | 0.57 (0.09 - 3.57) | 0.72 (0.33 - 1.59) |
| Peripheral vascular disease | 0.64 (0.40 - 1.03) | 2.64 (0.37 - 18.65) | 2.16 (0.69 - 6.77) | 1.40 (0.63 - 3.09) |
| Chronic lung disease | 2.50 (1.50 - 4.18) | 0.69 (0.12 - 3.96) | 1.22 (0.45 - 3.34) | 1.17 (0.56 - 2.43) |