| Need for pre-dilatation for stenting, n (%) | 257 (88.9) | 260 (90.0) | 0.6842 |
| Need for lesions debulking, n (%) | 67 (23.2) | 85 (29.4) | 0.3924 |
| Cutting balloon | 27 (9.3) | 34 (11.8) | |
| Scoring balloon | 23 (7.9) | 39 (13.5) | |
| Intravascular lithotripsy | 11 (3.8) | 8 (2.8) | |
| Rotablation | 8 (2.8) | 8 (2.8) | |
| Calcification, n (%) | 106 (36.7) | 138 (47.8) | 0.0804 |
| Proximal RVD, mm (mean ± SD) | 3.2 ± 0.6 | 3.3 ± 0.6 | 0.0456 |
| Distal RVD, mm (mean ± SD) | 2.8 ± 0.5 | 2.9 ± 0.6 | 0.0456 |
| Lesion length, mm (mean ± SD) | 29.4 ± 13.8 | 32.0 ± 13.7 | 0.0234 |
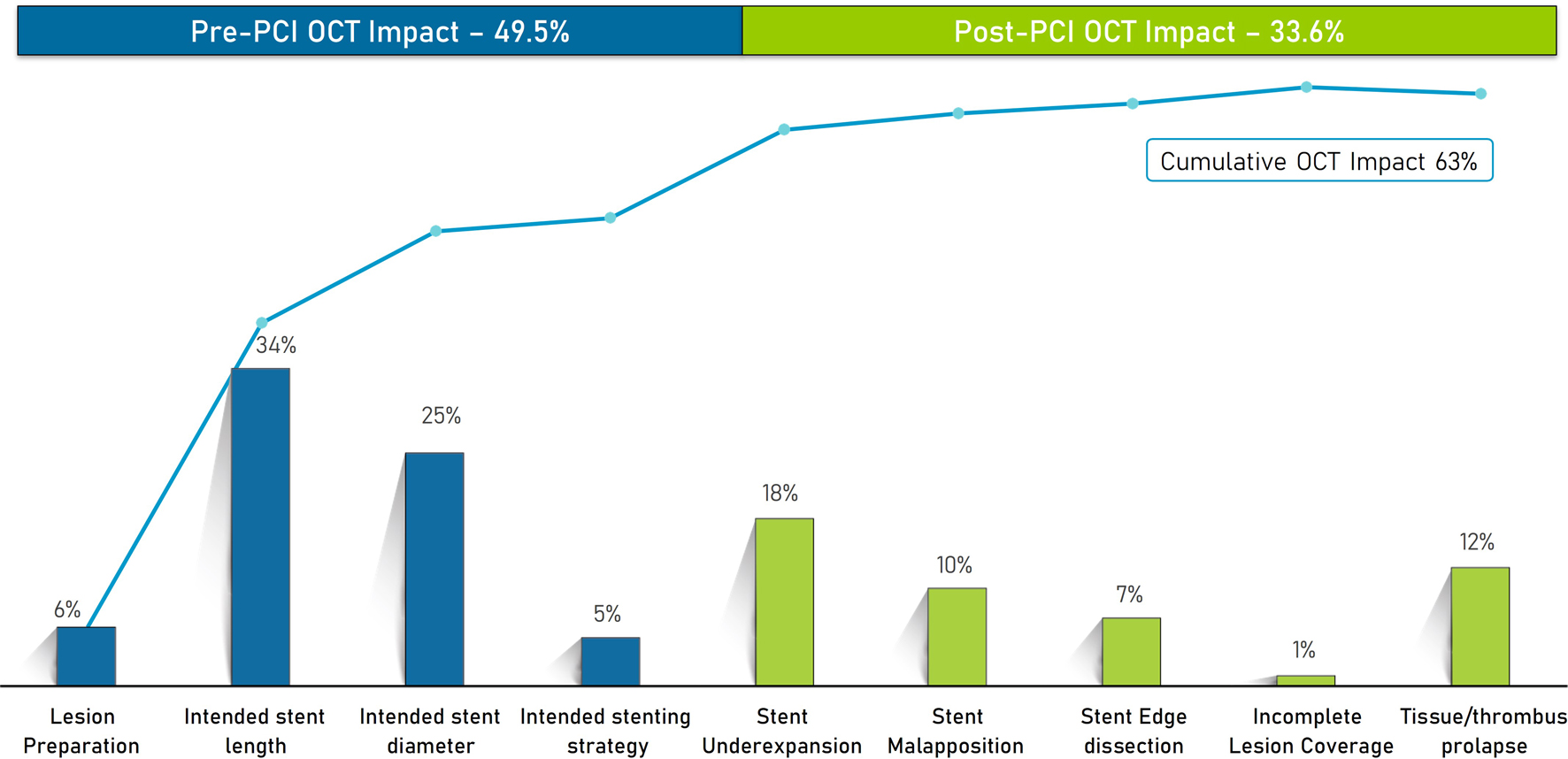
| Intended stent length, mm (mean ± SD) | 33.7 ± 14.6 | 35.5 ± 14.2 | < 0.0001 |
| Intended stent diameter, mm (mean ± SD) | 2.9 ± 0.4 | 3.0 ± 0.5 | 0.0082 |
| Intended number of stents, n (%) | | | |
| One | 250 (86.5) | 250 (86.5) | - |
| Two | 39 (13.5) | 39 (13.5) | - |