| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Case Report
Volume 15, Number 6, December 2024, pages 467-471
Intraoperative ST Segment Depression During General Anesthesia in a Child: Early Detection of Hypertrophic Cardiomyopathy
Joshua Gadelsayeda, Tariq Wanib, c, Saif Rehmanb, c, Joseph D. Tobiasb, c, d
aOhio University Heritage College of Osteopathic Medicine, Athens, OH, USA
bDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
cDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
dCorresponding Author: Joseph D. Tobias, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
Manuscript submitted August 26, 2024, accepted October 29, 2024, published online November 7, 2024
Short title: ECG Changes During Surgery in a Child
doi: https://doi.org/10.14740/cr1722
| Abstract | ▴Top |
Continuous electrocardiographic (ECG) monitoring remains crucial during surgery in infants and children. Although generally uncommon in pediatric-aged patients, ECG changes may occasionally be indicative of a variety of myocardial pathologies including anomalous origin of coronary arteries, ventricular hypertrophy, myocarditis, hypothermia, drug effects, electrolyte abnormalities, acid-base disturbances or conduction system disorders such as Wolff-Parkinson-White and Brugada syndrome. Distinguishing between pathologic and non-pathologic conditions impacting the ECG must be considered so that appropriate interventions are provided to prevent perioperative morbidity and mortality. We report a case of a 2-year-old child who exhibited ST segment depression and increased R wave amplitude during general anesthesia. Although the anesthetic care was uneventful and the patient was otherwise asymptomatic, immediate postoperative workup including echocardiogram revealed previously undiagnosed hypertrophic cardiomyopathy. The occurrence of intraoperative ST-T wave changes in this patient underscores the need for a high index of suspicion for underlying cardiac pathology, even in the absence of overt clinical manifestations. This case highlights the importance of intraoperative ECG monitoring in pediatric patients, explores the causes of ST-T wave changes, reviews similar cases in the literature, and proposes a pathway for perioperative evaluation.
Keywords: ST-T wave; ST segment; T wave; Electrocardiography; General anesthesia; Pediatric hypertrophic cardiomyopathy
| Introduction | ▴Top |
Given that majority of pediatric-aged patients do not have co-morbid cardiac diseases that may predispose them to the development of intraoperative coronary ischemia or arrhythmias, a three-lead electrocardiogram (ECG) is typically used as a routine part of intraoperative monitoring. Lead II is typically used, as it provides the P-wave morphology as well as identification and analysis of potential arrhythmias. In rare instances, where pediatric patients are at risk for ischemia, a five-lead ECG is used with monitoring of leads II and V5. Intraoperative ECG changes may be otherwise benign or indicative of a variety of myocardial pathologies (e.g., anomalous origin of coronary arteries, ventricular hypertrophy, myocarditis), hypothermia, drug effects, electrolyte abnormalities, acid-base disturbances, or conduction system disorders like Wolff-Parkinson-White and Brugada syndrome [1-5].
Distinguishing between pathologic and non-pathologic conditions impacting the ECG must be considered so that appropriate interventions are provided to prevent perioperative morbidity and mortality. Particular attention must be given to ST segment changes as they may be indicative of aberrations in the balance of myocardial oxygen demand and delivery, resulting in myocardial ischemia or infarction. In this report, we describe a 2-year-old patient who developed intraoperative ST segment depression and increased R wave amplitude. The role of intraoperative ECG monitoring in infants and children is discussed, the etiology of ST segment changes is presented, and previous reports of such events are reviewed.
| Case Report | ▴Top |
At the time of surgery, the patient was 2 years and 10 months old, weighing 18.6 kg. He was scheduled for left tympanoplasty to correct a left-sided tympanic membrane hemangioma. His past medical history was significant for snoring and adenoid hypertrophy. His previous general anesthesia encounters included magnetic resonance imaging (MRI) of the internal auditory canals, examination under anesthesia (EUA) of the ears, adenoidectomy, and tube insertion of the right ear - all without complications. A preoperative physical examination was unremarkable, with normal vital signs, and he was classified as American Society of Anesthesiologists (ASA) physical status 1. After being nil per os (NPO) for 6 h, the patient was transported to the operating room where standard ASA monitors were placed. Following the inhalation of increasing increments of sevoflurane in nitrous oxide, a peripheral intravenous cannula was placed. Propofol (60 mg) and morphine (2 mg) were administered, and his trachea was intubated. Shortly after induction, ST depression was noted in the three-lead ECG (Fig. 1). Lead placement was confirmed, and the patient was placed on 100% oxygen. His vital signs remained stable with normal sinus rhythm, and no hypotension or tachycardia. The procedure was paused, and a second anesthesiologist was consulted. A five-lead ECG was placed, and blood pressure was elevated by 15-25% with incremental doses of phenylephrine (5 - 15 µg), but the ST depression persisted. A serum troponin level was obtained. Given the absence of additional symptoms, the decision was made to continue with the surgery. The surgical procedure was completed without incident. The total anesthetic time was 94 min. At the completion of the procedure, the patient’s trachea was extubated, and he was transferred to the post-anesthesia care unit (PACU). Due to the severity of the ECG changes, a 12-lead ECG and an echocardiogram were obtained. The ECG demonstrated normal sinus rhythm, left axis deviation, left ventricular hypertrophy, ST elevation in inferior leads, ST depression in lateral leads, and borderline QT interval (Fig. 2). The echocardiogram showed severe non-obstructive hypertrophic cardiomyopathy (HCM), asymmetric hypertrophy of the interventricular septum, no valvular abnormalities, mildly dilated left atrium, impaired left ventricular relaxation with increased left atrial pressure, and hyperdynamic left ventricular systolic function. With these findings, a diagnosis of severe non-obstructive cardiomyopathy and severe asymmetric hypertrophy of the interventricular septum was made. Upon further discussion with the patient’s mother, it was discovered that two of the patient’s siblings had been diagnosed with HCM, though the patient himself had not been screened. Additionally, there was a family history of sudden death on his father’s side (great aunts). The father was not present, and the mother was unsure if he had ever been screened. The patient had no history of syncope and was asymptomatic except for pain in the epigastric region, which occurs with activity and rarely at rest. HCM genetic testing identified the pathological variant, MYH7, to be the cause of his HCM. It was recommended that all his first-degree relatives receive genetic testing for this condition. The patient was discharged home with a Holter monitor for 48 h, which was unremarkable. His activities were restricted to low static, low dynamic sports, and follow-up echocardiogram was scheduled for 3 months later. The follow-up echocardiogram showed persistent left ventricular hypertrophy but was otherwise stable.
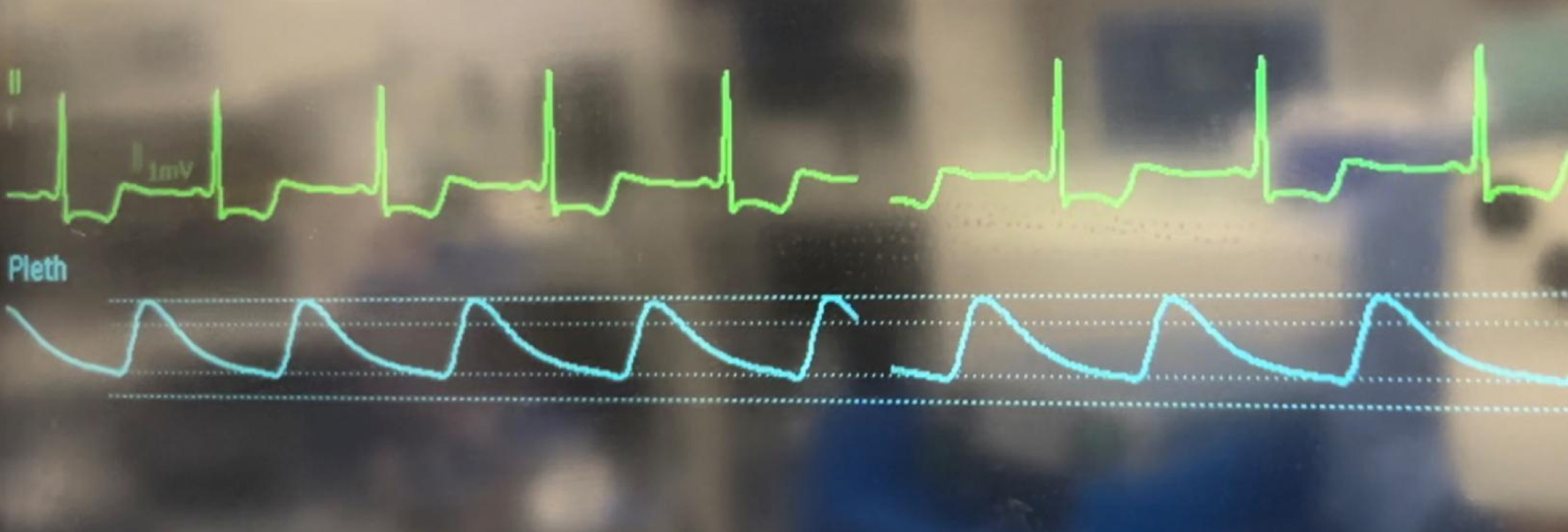 Click for large image | Figure 1. Photograph of the operating room monitor demonstrating ST segment depression. |
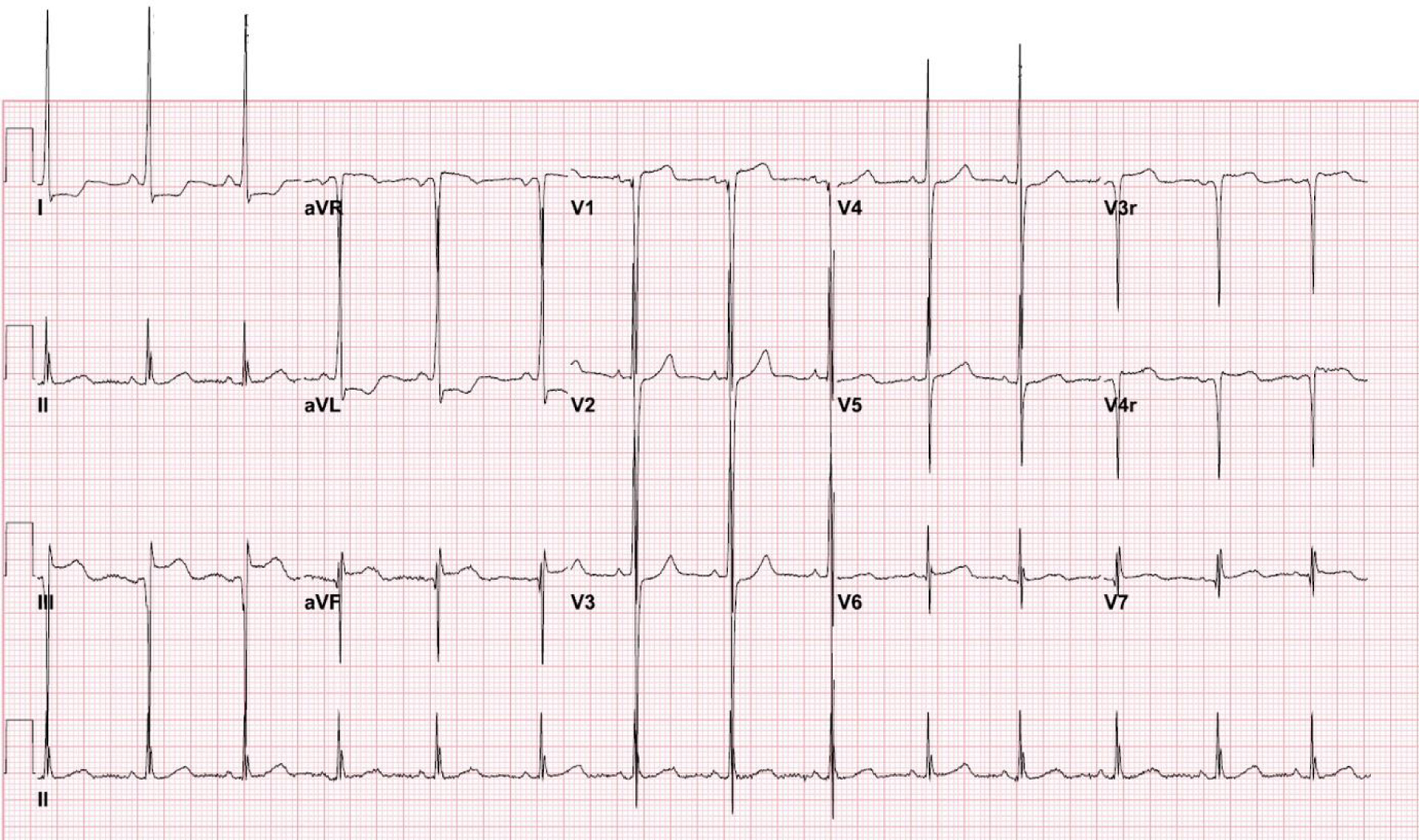 Click for large image | Figure 2. Postoperative electrocardiogram showing sinus rhythm, left axis deviation, left ventricular hypertrophy, ST elevation in inferior leads, ST depression in lateral leads, increased R wave amplitude, and borderline QT interval prolongation. |
| Discussion | ▴Top |
As the majority of pediatric-aged patients are free from co-morbid cardiac diseases that may predispose the development of intraoperative coronary ischemia or arrhythmias, a three-lead ECG is typically used as a routine part of intraoperative monitoring during general anesthesia with monitoring of lead II for P-wave morphology identification and arrhythmia analysis. In contrast, the adult population, where the risk of intraoperative ischemia is higher, a five-lead ECG is used to monitor the anterior and inferior myocardium, allowing for early detection of ischemic changes [6-8].
Intraoperative cardiovascular events in pediatric-aged patients are usually triggered by the anesthetic agents such as halothane, blood loss, or electrolyte disturbances [9, 10]. Unlike adults, pediatric-aged patients rarely experience intraoperative ST segment changes. Non-pathologic ST-T wave changes may be seen with J-point depression, early repolarization, or due to sympathetic stimulation related to surgical stimulation or an inadequate depth of anesthesia. However, these changes may also be a sign of significant cardiovascular disease including myocardial ischemia or infarction, left or right ventricular hypertrophy with strain, medication effects, inflammatory processes such as myocarditis and pericarditis, or electrolyte and acid-base disturbances (hypokalemia, hypernatremia, alkalosis). Reports of significant ST segment and T wave changes during intraoperative anesthetic care in infants and children remain limited (Table 1) [2, 4, 5, 11].
 Click to view | Table 1. Previous Reports of Intraoperative ST-T Wave Changes in Infants and Children |
Even though ST-T wave changes are generally of limited consequence in the absence of structural cardiac defects as noted in these case reports, they should not be overlooked and prompt evaluation is suggested given the potential that these changes may be an early warning sign of myocardial pathology including ischemia or even impending cardiac arrest. In our patient, ST depression was noted after induction, during the maintenance phase of anesthesia. As our patient was asymptomatic preoperatively and there were no intraoperative concerns, the surgical procedure was continued. To rule out myocardial ischemia as an etiology, phenylephrine was administered to increase the diastolic blood pressure and augment coronary perfusion. However, no change in the ST depression was noted.
Key components of myocardial oxygen delivery and demand include diastolic blood pressure and heart rate. Blood flow to the myocardium occurs primarily during diastole. It is regulated by the difference between the diastolic blood pressure and end diastolic pressure of the left ventricle, otherwise known as the myocardial perfusion pressure. Coronary blood flow occurs during diastole which is dependent on the heart. Myocardial oxygen demand is dependent on heart rate, end-diastolic pressure, afterload, and myocardial contractility. Given its involvement in both delivery and consumption, heart rate remains the key component of the myocardial oxygen supply-demand ratio.
Identification of potential pathologic causes of ST segment and T wave changes during intraoperative care includes maintenance of baseline vital signs, correction of hypotension, hypoxemia, and hypercarbia. We would also suggest pausing the surgical procedure in consideration of intraoperative cardiology consultation to rule out undiagnosed congenital or acquired cardiac disease with a formal 12-lead ECG and an echocardiogram. Once physiologic causes (hypotension) and anatomic cardiac diseases are eliminated, other causes including medication effect, electrolyte issues, and artifact should be considered.
In summary, we present a 2-year-old child who exhibited ST segment depression during intraoperative care. Regardless of the patient’s age, intraoperative ECG changes warrant a prompt investigation to rule out pathologic causes, most notably coronary ischemia. Supporting the primary determinants of myocardial oxygen delivery includes assurance of adequate oxygenation and blood pressure with control of heart rate. Additional diagnostic workup should be guided by the patient’s history and clinical scenario. This can then provide information on whether the surgical procedure should continue.
While it is common to observe ST-T wave changes in children during anesthesia and surgery, the majority of these alterations are benign and do not indicate underlying cardiac pathology. Identification of the abnormal ECG with a subsequent workup resulted in the early diagnosis of HCM in our patient. As illustrated by previous reports, the risk of myocardial ischemia is significantly higher in patients with congenital heart disease (CHD) or during surgery for CHD [9, 12]. HCM, a condition characterized by thickened heart muscle, can often remain asymptomatic or present with subtle signs. The occurrence of ST-T wave changes in this patient emphasizes the need for a high index of suspicion for underlying cardiac pathology, even in the absence of overt clinical manifestations. Given the risk of arrhythmias and sudden death associated with this condition, early identification and intervention may impact long-term outcomes.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained for anesthetic care and the use of de-identified information for publication.
Author Contributions
JG: preparation of initial, subsequent, and final drafts; JDT: concept, writing, and review of all drafts; TW and SR: perioperative care of the patient and review of final draft.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
ASA: American Society of Anesthesiologists; CHD: congenital heart disease; ECG: electrocardiogram; EUA: exam under anesthesia; HCM: hypertrophic cardiomyopathy; MRI: magnetic resonance imaging; NPO: nil per os; PACU: post-anesthesia care unit
| References | ▴Top |
- Landesberg G, Mosseri M, Wolf Y, Vesselov Y, Weissman C. Perioperative myocardial ischemia and infarction: identification by continuous 12-lead electrocardiogram with online ST-segment monitoring. Anesthesiology. 2002;96(2):264-270.
doi pubmed - Bell C, Rimar S, Barash P. Intraoperative ST-segment changes consistent with myocardial ischemia in the neonate: a report of three cases. Anesthesiology. 1989;71(4):601-604.
doi pubmed - Miyake CY, Davis AM, Motonaga KS, Dubin AM, Berul CI, Cecchin F. Infant ventricular fibrillation after ST-segment changes and QRS widening: a new cause of sudden infant death? Circ Arrhythm Electrophysiol. 2013;6(4):712-718.
doi pubmed - Alfirevic A, Mossad E, Niezgoda J. Unexpected ST segment changes in children—a case report. Paediatr Anaesth. 2005;15(1):63-67.
doi pubmed - Girshin M, Parikh SR, Leyvi G, Lakhani P, Lo LW, Wasnick JD. Intraoperative oxygen desaturation and electrocardiographic changes in a patient with Hanhart syndrome. J Cardiothorac Vasc Anesth. 2005;19(4):546-547.
doi pubmed - Morgan CA, Webb RK, Cockings J, Williamson JA. The Australian incident monitoring study. Cardiac arrest—an analysis of 2000 incident reports. Anaesth Intensive Care. 1993;21(5):626-637.
doi pubmed - Webb RK, van der Walt JH, Runciman WB, Williamson JA, Cockings J, Russell WJ, Helps S. The Australian incident monitoring study. Which monitor? An analysis of 2000 incident reports. Anaesth Intensive Care. 1993;21(5):529-542.
doi pubmed - Roy WL, Edelist G, Gilbert B. Myocardial ischemia during non-cardiac surgical procedures in patients with coronary-artery disease. Anesthesiology. 1979;51(5):393-397.
doi pubmed - Bhananker SM, Ramamoorthy C, Geiduschek JM, Posner KL, Domino KB, Haberkern CM, Campos JS, et al. Anesthesia-related cardiac arrest in children: update from the Pediatric Perioperative Cardiac Arrest Registry. Anesth Analg. 2007;105(2):344-350.
doi pubmed - Morray JP, Geiduschek JM, Ramamoorthy C, Haberkern CM, Hackel A, Caplan RA, Domino KB, et al. Anesthesia-related cardiac arrest in children: initial findings of the Pediatric Perioperative Cardiac Arrest (POCA) Registry. Anesthesiology. 2000;93(1):6-14.
doi pubmed - Geyer ED, Cartabuke RS, Schloss B, Tobias JB. Intraoperative ST segment, T wave changes in two infants during general anesthesia. Anaesth Pain Intensive Care. 2018;22(1):112-116.
- Testa L, Tobias JD, Kavanaugh-McHugh A. Hypoplastic left heart syndrome: anesthetic care prior to transplantation or surgical palliation. J Clin Anesth. 1994;6(6):500-504.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.