| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 000, Number 000, June 2025, pages 000-000
History of COVID-19 as a Risk Factor for Cardiac Arrhythmias: A Case-Control Study
Miriam Elizabeth Miranda-Corralesa , Joselyn Elizabeth Begazo-Paredesb
, Barbara Alejandra Garcia-Tejadac
, Giancarlo Alvarez-Cervantesd
, Jose Alfredo Sulla-Torresa
, Herbert Jesus Del Carpio Beltrane
, Jerry K. Benites-Mezaf, g
, Agueda Munoz-del-Carpio-Toiah, i
aEscuela de Postgrado, Vicerrectorado de Investigacion, Universidad Catolica de Santa Maria, Arequipa, Peru
bHospital III Yanahuara, Arequipa, Peru
cHospital III Goyeneche, Arequipa, Peru
dEscuela de Farmacia y Bioquimica, Escuela de Enfermeria, Vicerrectorado de Investigacion, Universidad Catolica de Santa Maria, Arequipa, Peru
eFacultad de Ingenieria y Arquitectura, Escuela Profesional de Ingenieria Industrial, Universidad Continental, Arequipa, Peru
fSociedad Cientifica de Estudiantes de Medicina de la Universidad Nacional de Trujillo, Trujillo, Peru
gNova Evidence Research Group, Trujillo, Peru
hVicerrectorado de Investigacion, Escuela de Postgrado, Estudios Generales, Universidad Catolica de Santa Maria, Arequipa, Peru
iCorresponding Author: Agueda Munoz-del-Carpio-Toia, Vicerrectorado de Investigacion, Escuela de Postgrado, Estudios Generales, Universidad Catolica de Santa Maria, Arequipa, Peru
Manuscript submitted January 5, 2025, accepted April 17, 2025, published online June 9, 2025
Short title: COVID-19 and Risk of Cardiac Arrhythmias
doi: https://doi.org/10.14740/cr2042
| Abstract | ▴Top |
Background: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was responsible for the coronavirus disease 2019 (COVID-19) pandemic and generated high morbidity and mortality rates worldwide, as well as several sequelae that persist and need to be evaluated. The aim of this study was to evaluate the association between a history of COVID-19 infection and the occurrence of cardiac arrhythmias in outpatients from a private clinic in Arequipa.
Methods: We conducted a retrospective, analytical, unmatched case-control study in a private cardiology clinic in Arequipa, Peru. A total of 252 adult patients who underwent 24-h Holter monitoring between October and December 2023 were included. Cases were defined as patients with documented cardiac arrhythmias; controls had no arrhythmic findings. The main exposure was a confirmed history of COVID-19. Age, sex, and additional Holter findings were also analyzed. Logistic regression was used to estimate crude and adjusted odds ratios (ORs) with 95% confidence intervals (CIs), adjusting for age and sex.
Results: Of the total sample, 68 patients were classified as cases and 184 as controls. A history of COVID-19 was more frequent among cases (70.6%) than among controls (50.5%) (P = 0.004). In unadjusted analysis, patients with prior COVID-19 had more than twice the odds of presenting arrhythmias (OR: 2.35; 95% CI: 1.29 - 4.26; P = 0.005). After adjusting for age and sex, the association remained statistically significant (OR: 2.12; 95% CI: 1.10 - 4.11; P = 0.025).
Conclusion: A prior history of COVID-19 was significantly associated with increased odds of cardiac arrhythmias. These findings highlight the importance of structured cardiac evaluation in patients with prior SARS-CoV-2 infection.
Keywords: COVID-19; Sequelae; Cardiac arrhythmia; Holter
| Introduction | ▴Top |
Since its emergence in late 2020, the coronavirus disease 2019 (COVID-19) pandemic has been devastating in Latin America, with high morbidity and mortality rates [1]. In addition to its acute effects, this disease has resulted in multiple sequelae [2, 3] and has been linked to new hematological [4], pulmonary, cardiovascular [5, 6], renal, endocrine, gastrointestinal, dermatological, neuropsychiatric diseases, among others [7, 8].
The population has been affected by a growing number of cardiovascular complications among patients experiencing post-acute sequelae of COVID-19 [9]. Myocardial damage may be caused by direct viral involvement with a local inflammatory response or by an exaggerated systemic reaction characterized by cytokine release and a prothrombotic state. Along with vascular involvement, these factors can trigger thrombotic and ischemic events due to microvascular damage or destabilization of preexisting atheroma plaques [5].
Currently, there is an increasing number of myocarditis, arrhythmias, and myocardial injury cases, underscoring the urgent need for further research [10-12]. COVID-19 infection can worsen cardiovascular health, particularly in vulnerable groups such as pregnant women or patients with pre-existing cardiovascular disease [13]. Several mechanisms have been proposed to explain how severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) affects the heart, including direct viral cytotoxicity and an excessive immune response [14]. It has also been studied that the virus enters cells through angiotensin-converting enzyme 2 (ACE2) receptors, causing direct myocardial injury [15]. Another theory suggests that ACE2 downregulation prevents the cardioprotective effects of angiotensin 1-7, triggering an inflammatory cascade with tumor necrosis factor-alpha (TNF-α) production that may ultimately damage cardiomyocytes [16]. Likewise, the myocardial inflammation caused by SARS-CoV-2 may trigger cardiac arrhythmias through electrophysiological and structural remodeling or ion channel dysfunction [17]. The aim of this study was to evaluate the association between a history of COVID-19 infection and the occurrence of cardiac arrhythmias in outpatients from a private clinic in Arequipa.
| Materials and Methods | ▴Top |
Study design
An observational, analytical, and retrospective unmatched case-control study was conducted, based on the review of medical records and 24-h Holter cardiac monitoring reports from a private cardiology clinic in the city of Arequipa, Peru.
Population, sample, and sampling
The study population consisted of 252 adult patients who attended outpatient cardiology consultations during the specified period. All patients had been referred for 24-h Holter monitoring due to symptoms suggestive of cardiac arrhythmias, including palpitations, dizziness, syncope, atypical chest pain, or a prior history of cardiovascular disease. The arrhythmic findings were verified and confirmed by a qualified cardiologist. A non-probabilistic convenience sampling method was used, including all patients who met the eligibility criteria.
Eligibility criteria
Cases were defined as patients aged 18 years or older, of either sex, with documented evidence of cardiac arrhythmia in their Holter reports, based on established electrocardiographic criteria. All arrhythmic findings were verified and confirmed by a qualified cardiologist. Controls were defined as patients whose Holter reports showed no evidence of arrhythmia, according to the interpretation of the same cardiologist. Patients were excluded from the study if they had a permanent pacemaker or an implantable cardioverter-defibrillator (ICD), due to the inability of Holter devices to accurately assess intrinsic cardiac activity in such cases. Additionally, those with incomplete or technically invalid Holter data, or with missing essential clinical information, were also excluded.
Variables, instruments, and procedures
The dependent variable was the diagnosis of cardiac arrhythmia, based on findings reported in the 24-h Holter recording. Standard electrocardiographic criteria were used to classify arrhythmic events. Holter monitoring was performed using a three-channel device, and the recordings were analyzed using manufacturer-validated automated software, followed by manual verification by an experienced cardiologist. Only complete and clinically validated reports were included.
The exposure variable was a history of confirmed COVID-19 infection, defined exclusively through documentation in the patients’ medical records, based on positive results of either molecular (reverse transcription polymerase chain reaction (RT-PCR)) or antigen tests recorded during the clinical course.
In addition, the following covariates were obtained from the clinical records and Holter reports: age (years), sex (male/female), and additional Holter findings, including the number and type of ventricular and supraventricular events, as described above. Ventricular extrasystoles (VEs) were defined as premature beats with wide QRS complexes (≥ 120 ms) and no preceding P wave [18]. Supraventricular extrasystoles (SVEs) were defined as premature beats with narrow QRS complexes (< 120 ms), preceded by an abnormal P wave of different morphology from the baseline rhythm [18]. Ventricular tachycardia (VT) was defined as three or more consecutive ventricular beats with a heart rate ≥ 100 beats per minute (bpm) and wide QRS complexes and further classified as sustained (> 30 s) or non-sustained (< 30 s) [18]. Comorbidities and clinical indications for Holter monitoring were not consistently available and were therefore not included in the analysis.
Statistical analysis
The information from the cardiac Holter was extracted into a database of the Microsoft Excel 2019 program to be subsequently verified by a cardiologist. Then, it was exported to the statistical program STATA v16.0 (StataCorp, TX) for their respective analyses. First, in the univariate analysis, qualitative variables were reported using frequencies and percentages. Quantitative variables were reported using measures of central tendency and dispersion after evaluation of their normality. Second, bivariate analyses were performed according to the presence of a history of COVID-19. When comparing categorical variables, the Chi-square test or Fisher’s exact test was used. The Student’s t-test was used to compare numerical variables according to the groups formed.
Additionally, binary logistic regression was performed to estimate crude and adjusted odds ratios (ORs) with 95% confidence intervals (CIs), evaluating the association between a history of COVID-19 and the presence of arrhythmia. The model was adjusted for age and sex. Statistically significant differences were considered to exist if the P-value was less than 0.05.
Ethical guidelines
This study was approved by the favorable opinion 160-2023 of the Institutional Research Ethics Committee of the Universidad Catolica de Santa Maria in Arequipa, for adhering to the ethical standards of the institution, as well as to the principles established in the Declaration of Helsinki.
| Results | ▴Top |
A total of 68 cases of adult patients with a diagnosis of cardiac arrhythmia and 184 controls without cardiac arrhythmia were included. Patients with cardiac arrhythmias were significantly older than those without arrhythmias (mean age: 62.97 ± 19.13 vs. 44.69 ± 15.32 years; P < 0.001). There were no significant differences in sex distribution between cases and controls (P = 0.329). A history of COVID-19 was more common among cases than controls (70.59% vs. 50.54%, respectively; P = 0.004) (Table 1).
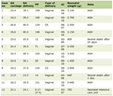 Click to view | Table 1. General Characteristics According to Diagnosis of Arrhythmia in Cardiac Patients in Arequipa |
When evaluating the findings in cardiac Holter monitoring according to the history of COVID-19, we found that when evaluating heart rate variability, the maximum heart rate was significantly lower for those who had a history of COVID-19 compared to those who did not (P = 0.046). Likewise, no statistically significant differences were found for any other variable (Table 2).
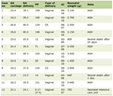 Click to view | Table 2. Findings in Cardiac Holter Monitoring According to the History of COVID-19 in Cardiac Patients in Arequipa |
When evaluating the association between a history of COVID-19 infection and cardiac arrhythmia, the crude model showed that patients with a history of COVID-19 infection were significantly more likely to have arrhythmia compared to those without such a history (OR: 2.35; 95% CI: 1.29 - 4.26; P = 0.005). Then, after adjusting for age and sex, the association remained statistically significant (OR: 2.12; 95% CI: 1.10 - 4.11; P = 0.025) (Table 3).
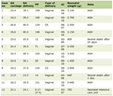 Click to view | Table 3. Association Between a History of COVID-19 and Cardiac Arrhythmias in Cardiac Patients in Arequipa |
| Discussion | ▴Top |
Main findings
Our findings showed that patients with arrhythmias had a higher proportion of previous COVID-19 infection (70.6% vs. 50.5%). Logistic regression analysis showed that a history of COVID-19 was associated with more than twice the odds of presenting arrhythmias, even after adjusting for age and sex. Additionally, maximum heart rate was significantly lower in patients with a COVID-19 history.
Comparison with other studies
According to reviews of previous studies, cardiac complications are typically present in 20% to 30% of COVID-19 patients [19], with arrhythmias reported in approximately 10% to 20% of cases [20], which is consistent with the findings of our study. However, although some reports indicate that atrial fibrillation is the most common arrhythmia in patients with a history of COVID-19 [21], our data showed a higher prevalence of sinus rhythm disturbances and other tachyarrhythmias. Furthermore, Mooren et al [22] found a significant association between SARS-CoV-2 infection and cardiac rhythm disorders, which aligns with our finding of a significantly lower maximum heart rate in individuals with a history of COVID-19 (P = 0.046), supporting the hypothesis of rhythm dysfunction in this population.
Studies using Holter monitoring in convalescent COVID-19 patients have also documented a substantial arrhythmic burden. For example, Ingul et al (2022) reported that 27% of patients had arrhythmias on a 24-h Holter monitor 3 months after hospitalization, with the most common findings being frequent premature ventricular contractions (in 18%) and non-sustained ventricular tachycardia (in 5%) [23]. This high prevalence likely reflects a population with more severe acute illness and more intensive follow-up. In contrast, the Italian ARCA post-COVID registry, which included both hospitalized and non-hospitalized patients, found a lower overall arrhythmia prevalence (about 6% on Holter), suggesting that reported frequencies vary depending on patient selection and timing of evaluation [24].
Interpretation of results
The higher prevalence of arrhythmias in patients with a history of COVID-19 suggests possible direct and indirect myocardial damage, including inflammatory and prothrombotic processes that foster rhythm disturbances [19]. Furthermore, multifactorial toxicity in cardiac tissue may explain the early emergence of arrhythmias as one of the first post-infection complications [19]. This phenomenon can be attributed to the direct infection of cardiomyocytes by SARS-CoV-2 through ACE2 receptors, as well as to indirect injury mediated by an exaggerated immune response, autonomic dysfunction, hypoxemia, and microthrombi formation, all of which can induce fibrosis and electrical instability [19]. Cardiac magnetic resonance imaging (MRI) studies have shown that even patients with mild COVID-19 may exhibit persistent myocardial inflammation weeks after infection [25, 26]. Nevertheless, reasonable doubts remain about the exact impact of COVID-19 on cardiac symptoms, the possible relationship with vaccination [27, 28], and the influence of infection severity [29].
Clinical relevance
Our findings have important clinical implications for the management of post-COVID patients, highlighting the need for rigorous cardiovascular follow-up, even in those who had mild illness but present with persistent symptoms such as palpitations, dizziness, or chest pain. Even patients who were not hospitalized for the infection should not be considered “low risk”; studies have shown that elevated cardiovascular risk is present even in mild cases, though it increases with disease severity [30]. In this context, expert consensus guidelines recommend a comprehensive cardiovascular evaluation in long COVID patients who report cardiac symptoms [31].
Another relevant clinical aspect is the role of COVID-19 vaccination in cardiovascular outcomes. Vaccination has been associated with a lower incidence of post-COVID cardiac complications. Recent large cohort data from the United Kingdom indicate that individuals who contracted COVID-19 after being vaccinated had a significantly lower risk of cardiovascular events in the post-acute phase compared to unvaccinated individuals [32]. In other words, by mitigating the severity of the infection, vaccines appear to indirectly protect against long-term cardiac sequelae of COVID-19. This finding reinforces public health messages promoting widespread vaccination not only to prevent acute COVID-19 hospitalizations and deaths but also to reduce the burden of long COVID [33], including arrhythmias and heart failure [34].
On the other hand, it is important to recognize and monitor the rare cardiovascular side effects of vaccination. mRNA COVID-19 vaccines have been associated with a small risk of myocarditis in young males, with an approximate incidence of 1 in 25,000 (around 40 cases per million second doses in men under 30 years) [31]. Fortunately, these cases have mostly been mild and self-limiting, with recovery occurring without serious complications [35]. The current consensus remains that the benefit-risk ratio of vaccination is highly favorable in terms of cardiovascular health [31]. Clinicians should be aware of both aspects: promoting preventive vaccination to reduce the long-term cardiac risks of COVID-19 and being prepared to evaluate and manage the rare cases of post-vaccine myocarditis.
Early identification of arrhythmias or cardiac dysfunction allows for timely interventions that can improve outcomes and quality of life in COVID-19 survivors. The results of our study reinforce the growing recognition of long-term cardiovascular problems following COVID-19 and support current recommendations for comprehensive cardiologic care in the post-acute phase.
Limitations and strengths
This study has several limitations. It was conducted in a single private institution in Peru, which may limit the external validity of the findings. The retrospective nature of data collection precluded assessment of infection severity, time since COVID-19 diagnosis, or presence of comorbid conditions such as hypertension or diabetes. Additionally, vaccination status and body mass index were not consistently recorded, preventing adjustment for these potentially relevant variables. Nonetheless, the systematic use of Holter monitoring and the consistency of our results with international literature constitute strengths that highlight the significant impact of COVID-19 on cardiovascular health, emphasizing the need for further investigation into pathophysiological mechanisms, as well as prevention and treatment strategies.
Conclusion
A history of COVID-19 infection was significantly associated with higher odds of cardiac arrhythmias among patients undergoing Holter monitoring. Although the types of arrhythmias did not differ markedly between groups, these findings support the need for targeted cardiac evaluation in post-COVID outpatients to detect potential rhythm disorders early and guide clinical management.
Acknowledgments
None to declare.
Financial Disclosure
This work was funded by CONCYTEC through the PROCIENCIA program, as part of the “Proyectos de Investigacion Aplicada 2022-02” call, under contract [PE501080050-2022]. The results come from the sub study “Sociodemographic, clinical and cardiac monitoring characteristics of patients with a history of cardiac sequelae due to COVID-19 Arequipa, 2023” postgraduate thesis by author Miranda Corrales, Miriam Elizabeth (Vicerrectorado de Investigación, Escuela de Postgrado, Universidad Católica de Santa Maria).
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Informed Consent
All patients consented to be part of the study.
Author Contributions
MEMC and AMdCT conceptualized and designed the study. MEMC, AMdCT, JEBP, BAGT, GAC, JAST, and JKBM were involved in data acquisition, formal analysis, and data interpretation. MEMC, AMdCT, JEBP, BAGT, GAC, JAST, HJDCB, and JKBM contributed to the drafting of the original manuscript and provided input during the revision of the original draft. All authors participated in the review and approval of the final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
ACE2: angiotensin-converting enzyme 2; bpm: beats per minute; CI: confidence interval; COVID-19: coronavirus disease 2019; ICD: implantable cardioverter-defibrillator; MRI: magnetic resonance imaging; OR: odds ratio; RT-PCR: reverse transcription polymerase chain reaction; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; SVEs: supraventricular extrasystoles; TNF-α: tumor necrosis factor-alpha; VEs: ventricular extrasystoles; VT: ventricular tachycardia
| References | ▴Top |
- Prieto-Silva R, Sarmiento-Hernandez CA, Prieto-Silva F. Morbidity and mortality due to COVID-19 in Latin America: Study of three countries-February to July 2020. Rev Salud Publica. 2020;22:1-7.
doi - Pinto Borges L, Gibara Guimaraes A, Camargo Mendonca de Araujo F, Bispo de Souza J, Raguer Valadao Souza D, Fagundes Martins A, et al. Main Clinical sequels in patients affected by COVID-19: a systematic review. Acta Sci Paediatr. 2021;4:42-50.
doi - Han Q, Zheng B, Daines L, Sheikh A. Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens. 2022;11(2):269.
doi pubmed - Bonow RO, Fonarow GC, O'Gara PT, Yancy CW. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5(7):751-753.
doi pubmed - Calvo-Fernandez A, Izquierdo A, Subirana I, Farre N, Vila J, Duran X, Garcia-Guimaraes M, et al. Markers of myocardial injury in the prediction of short-term COVID-19 prognosis. Rev Esp Cardiol (Engl Ed). 2021;74(7):576-583.
doi pubmed - Vitales-Noyola M, Alvarado-Hernandez DL, Sanchez-Gutierrez R, Hernandez-Castro B, Gonzalez-Baranda L, Bernal-Silva S, Comas-Garcia A, et al. Analysis of the blood levels of NK and NKT cells in patients with severe SARS-CoV-2 infection. Iran J Immunol. 2024;21(4):340-352.
doi pubmed - Fernandez Ortega MA, Sanchez Mendez I, Chavez Ciriaco A. Secuelas neurologicas post COVID-19: revision bibliografica. Arch en Med Fam. 2024;26:171-175.
doi - Wong Chew RM, Angel Ambrocio AH, Bautista Carbajal P, Garcia Leon ML, Vite Velazquez X, Cortazar Maldonado LA, et al. Efectos a largo plazo de la COVID-19: una revision de la literatura. Acta Medica Grup Angeles. 2021;19:421-428.
doi - Peramo-Alvarez FP, Lopez-Zuniga MA, Lopez-Ruz MA. Medical sequels of COVID-19. Med Clin (Barc). 2021;157(8):388-394.
doi pubmed - Ballering AV, van Zon SKR, Olde Hartman TC, Rosmalen JGM, Lifelines Corona Research I. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet. 2022;400(10350):452-461.
doi pubmed - Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker-Smith CM, et al. Heart disease and stroke statistics-2023 update: a report from the American Heart Association. Circulation. 2023;147(8):e93-e621.
doi pubmed - Hiscott J, Alexandridi M, Muscolini M, Tassone E, Palermo E, Soultsioti M, Zevini A. The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 2020;53:1-9.
doi pubmed - Falconi Chavez Michel Estephania, Bastidas Jimbo Joel David, Llanga Urquizo Grace Mishell. Efectos a largo plazo de la COVID-19 en la salud pulmonar y cardiovascular: una revision del estado del arte. INVECOM. 2023;4.
- Shao HH, Yin RX. Pathogenic mechanisms of cardiovascular damage in COVID-19. Mol Med. 2024;30(1):92.
doi pubmed - Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259-260.
doi pubmed - Zhao YH, Zhao L, Yang XC, Wang P. Cardiovascular complications of SARS-CoV-2 infection (COVID-19): a systematic review and meta-analysis. Rev Cardiovasc Med. 2021;22(1):159-165.
doi pubmed - Babapoor-Farrokhran S, Rasekhi RT, Gill D, Babapoor S, Amanullah A. Arrhythmia in COVID-19. SN Compr Clin Med. 2020;2(9):1430-1435.
doi pubmed - Goldberger AL, Goldberger ZD, Shvilkin A. Goldberger’s clinical electrocardiography: a simplified approach. Ninth Edit. Elsevier; 2018.
doi - Huseynov A, Akin I, Duerschmied D, Scharf RE. Cardiac arrhythmias in post-COVID syndrome: prevalence, pathology, diagnosis, and treatment. Viruses. 2023;15(2):389.
doi pubmed - Saha SA, Russo AM, Chung MK, Deering TF, Lakkireddy D, Gopinathannair R. COVID-19 and cardiac arrhythmias: a contemporary review. Curr Treat Options Cardiovasc Med. 2022;24(6):87-107.
doi pubmed - Salama AE, Hasanein MT, Gouda M, Abrayik JA, Taha MM. Correlation between left atrial strain and subtle cardiac arrhythmias detected by holter monitoring in non-cardiac individual recovering from COVID-19. Egypt J Hosp Med. 2023;90:1210-1216.
doi - Mooren FC, Bockelmann I, Waranski M, Kotewitsch M, Teschler M, Schafer H, Schmitz B. Autonomic dysregulation in long-term patients suffering from Post-COVID-19 Syndrome assessed by heart rate variability. Sci Rep. 2023;13(1):15814.
doi pubmed - Ingul CB, Grimsmo J, Mecinaj A, Trebinjac D, Berger Nossen M, Andrup S, Grenne B, et al. Cardiac dysfunction and arrhythmias 3 months after hospitalization for COVID-19. J Am Heart Assoc. 2022;11(3):e023473.
doi pubmed - Antoncecchi V, Antoncecchi E, Orsini E, D'Ascenzo G, Oliviero U, Savino K, Aloisio A, et al. High prevalence of cardiac post-acute sequelae in patients recovered from Covid-19. Results from the ARCA post-COVID study. Int J Cardiol Cardiovasc Risk Prev. 2024;21:200267.
doi pubmed - Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, Liu W, et al. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13(11):2330-2339.
doi pubmed - Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265-1273.
doi pubmed - Bikdeli B, Khairani CD, Krishnathasan D, Bejjani A, Armero A, Tristani A, Davies J, et al. Major cardiovascular events after COVID-19, event rates post-vaccination, antiviral or anti-inflammatory therapy, and temporal trends: Rationale and methodology of the CORONA-VTE-Network study. Thromb Res. 2023;228:94-104.
doi pubmed - Jiang J, Chan L, Kauffman J, Narula J, Charney AW, Oh W, Nadkarni G, et al. Impact of vaccination on major adverse cardiovascular events in patients with covid-19 infection. J Am Coll Cardiol. 2023;81(9):928-930.
doi pubmed - Wiemken TL, McGrath LJ, Andersen KM, Khan F, Malhotra D, Alfred T, Nguyen JL, et al. Coronavirus disease 2019 severity and risk of subsequent cardiovascular events. Clin Infect Dis. 2023;76(3):e42-e50.
doi pubmed - Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583-590.
doi pubmed - ACC Issues Clinical Guidance on Cardiovascular Consequences of COVID-19 - American College of Cardiology. Am Coll Cardiol. 2022. https://www.acc.org/About-ACC/Press-Releases/2022/03/16/15/28/ACC-Issues-Clinical-Guidance-on-Cardiovascular-Consequences-of-COVID-19.
- Cezard GI, Denholm RE, Knight R, Wei Y, Teece L, Toms R, Forbes HJ, et al. Impact of vaccination on the association of COVID-19 with cardiovascular diseases: An OpenSAFELY cohort study. Nat Commun. 2024;15(1):2173.
doi pubmed - Fatima S, Ismail M, Ejaz T, Shah Z, Fatima S, Shahzaib M, Jafri HM. Association between long COVID and vaccination: A 12-month follow-up study in a low- to middle-income country. PLoS One. 2023;18(11):e0294780.
doi pubmed - Wang W, Wang CY, Wang SI, Wei JC. Long-term cardiovascular outcomes in COVID-19 survivors among non-vaccinated population: A retrospective cohort study from the TriNetX US collaborative networks. EClinicalMedicine. 2022;53:101619.
doi pubmed - Jain SS, Anderson SA, Steele JM, Wilson HC, Muniz JC, Soslow JH, Beroukhim RS, et al. Cardiac manifestations and outcomes of COVID-19 vaccine-associated myocarditis in the young in the USA: longitudinal results from the Myocarditis After COVID Vaccination (MACiV) multicenter study. EClinicalMedicine. 2024;76:102809.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.