| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 16, Number 3, June 2025, pages 202-211
Progression of Atherosclerosis and Hypothesis on the Relationship Between Microvascular Dysfunction, Cardiovascular Risk, and Cancer
Ansgar Adamsa, d, Waldemar Bojarab, Michel Romanensc
aB·A·D Health Care and Safety Technology Centre GmbH, Koblenz, Germany
bCommunity Clinic Mittelrhein, Kemperhof II, The Cardiology Clinic, Koblenz, Germany
cVascular Risk Foundation (Varifo), Olten, Switzerland
dCorresponding Author: Ansgar Adams, B·A·D Gesundheitsvorsorge und Sicherheitstechnik GmbH Zentrum Koblenz, Bubenheimer Bann 4, 56070 Koblenz, Germany
Manuscript submitted January 17, 2025, accepted March 31, 2025, published online April 11, 2025
Short title: Microvascular Dysfunction, Heart Risk and Cancer
doi: https://doi.org/10.14740/cr2049
| Abstract | ▴Top |
Background: The extent of atherosclerosis in healthy men and women was measured using ultrasound in the carotid artery and whether the progression could be predicted using the classic risk factors was investigated. A hypothesis was also formulated as to how microvascular dysfunction and atherosclerosis, on the one hand, and cardiovascular disease and cancer, on the other hand, might be related. To describe the relationship between atherosclerosis and cancer, the classic risk factors and plaque burden were compared.
Methods: From 2009 to 2024, 10,597 subjects (44% women) aged 20 - 65 years without signs of cardiovascular disease were examined using ultrasound of the carotid artery. The sum of all plaque areas (total plaque area (TPA)) and the maximum plaque thickness were measured. Follow-up examinations were carried out on 4,520 subjects (42% women) aged 40 - 65 years. In 2,397 men without cancer or cardiovascular events during follow-up, the classic risk factors and plaque burden were compared between 55 men who had a solid tumor and 188 men who had a cardiovascular event, and whether patients with cancer and a cardiovascular event exhibited different risk profiles was examined.
Results: In the age group of 35 - 65 years, 12% of men and 4.2% of women had advanced atherosclerosis (types III and IVb). In the age group of 40 - 65 years, 2,592 men and 1,928 women were followed up. Low to moderate atherosclerosis was present in 2,052 (79.2%) men and 1,761 (91.3%) women. Advanced atherosclerosis developed in 139 (6.8%) men and 39 (2.2%) women, which could not be predicted by the classical risk factors (P > 0.05). The mean follow-up time was 73 months (6.1 years) for men and 75 months (6.3 years) for women. Patients without cancer or cardiovascular disease have lower risk factors and lower plaque burden compared to men with cancer or cardiovascular events. Patients with cancer have very similar high-risk factors and high plaque burden compared to patients with cardiovascular disease.
Conclusion: By measuring the plaque burden on the carotid artery, a good risk stratification can be achieved in every age group. A follow-up examination every 3 - 5 years is advisable, as a rapid progression of the disease cannot be predicted taking into account the classic risk factors. Early treatment of advanced atherosclerosis improves the prognosis for cardiovascular diseases and possibly also for certain types of cancer. Patients with cancer and cardiovascular events show a similar risk profile and plaque burden.
Keywords: Microvascular dysfunction; Atherosclerosis; Cardiovascular risk; Cancer; Carotid ultrasound
| Introduction | ▴Top |
Atherosclerosis is the most common cause of death in industrialized countries. It is a systemic disease of the arteries that manifests itself in the entire vascular system. Cardiovascular diseases such as heart attacks, strokes, and peripheral arterial disease (PAD) are the most common. The small vessels can also be affected, which manifests itself in the heart through coronary microvascular dysfunction [1]. There is evidence that cancer is also associated with atherosclerosis and impaired microcirculation [2-10]. In every age group, there are people with a high plaque burden and rapid progression of the disease within a few years.
Ultrasound examination of the carotid artery can detect people with advanced disease in the subclinical stage and treat them early, which can improve the prognosis [10]. The extent of the disease can be easily determined by measuring plaque area (total plaque area (TPA)) and maximum plaque thickness with ultrasound. The aim of the study was to investigate the extent of atherosclerosis by sex and age group and whether the individual course of the disease can be predicted. Furthermore, the classic risk factors and plaque burden were compared in men with new cardiovascular events and cancer.
A hypothesis was formulated as to how microvascular dysfunction and atherosclerosis on the one hand and cardiovascular disease and cancer on the other hand could be related.
| Materials and Methods | ▴Top |
Study design
This was a retrospective study. All described investigations and evaluations on humans were conducted with the approval of the responsible ethics committee. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Study population
Between 2009 and 2024, an ultrasound examination of the carotid artery was offered as part of occupational health screening in companies in various sectors (chemicals, glass, pharmaceuticals, administration, metal, social services, paper, printing, ceramics, IT, university, university of applied sciences, and retail) in the region around Koblenz.
A total of 10,597 subjects (44% women) aged 20 - 65 years without signs of cardiovascular disease were examined by ultrasound of the carotid artery, and the sum of all plaque areas (TPA) and the maximum plaque thickness were measured.
A portable ultrasound device from Kontron Medical, type Imagic Agile, with a 10 MHz linear scanner was used.
Carotid plaque measurements
The measurement method was performed as previously published [10]. The classification of ultrasound findings was developed in an independent population of patients who were examined 1 day before a planned coronary angiography.
A low risk corresponds to ultrasound findings types I and IIa, a medium risk to findings types IIb and IVa, and a high risk to findings types III and IVb.
Follow-up examinations were carried out on 3,813 subjects (42% women) with a low to medium risk aged 40 - 65 years (follow-up men 57.8%, women 51.1%).
Baseline and follow-up examinations
At baseline and follow-up examinations, history of previous cancer and cardiovascular disease (myocardial infarction, stroke, coronary artery bypass grafting (CABG), and percutaneous transluminal coronary angioplasty (PTCA)) was obtained. Follow-up examinations were carried out on 3,813 subjects (42% women) with a low to medium risk aged 40 - 65 years (follow-up men 57.8%, women 51.1%). The proportion of subjects who changed from a low and medium risk of plaque to a high risk was determined and whether this was predictable taking into account the classic risk factors (lipids, hypertension, diabetes, smoking, familial risk, and body mass index).
In 2,397 men without cancer or cardiovascular events during follow-up, the classic risk factors and plaque burden were compared between 55 men who had a solid tumor and 188 men who had a cardiovascular event, and whether patients with cancer and a cardiovascular event exhibited different risk profiles was examined. Due to the low cancer incidence in women with 15 cases, a statistical evaluation was not carried out.
Myocardial infarction, stroke, CABG, and PTCA or angiographically proven coronary stenosis > 50% were classified as cardiovascular events.
Clinical intervention and patient management
Patients at high risk (types III and IVb ultrasound findings) received a letter to their family doctor to start treatment with a statin, for example, atorvastatin. Two hundred fifty-nine (47.9%) men and 98 (58.7%) women received a statin. In 15 subjects, statin use was irregular. If the duration of use was less than 50% of the follow-up period, it was considered no treatment, and vice versa. In 11 subjects, statins were not tolerated and had to be discontinued. The statin dose remained constant between the first and second visits and was adhered to by the patients.
Statistical analysis
The baseline characteristics of all subjects by risk group were described (continuously scaled: mean, standard deviation; categorically scaled: absolute and relative frequencies) and compared using t-test.
For each age group from 20 to 65 years, percentile curves of the plaque area (TPA) were created for men and women and the percentage of subjects with advanced atherosclerosis (type III-IVb findings) was shown.
| Results | ▴Top |
To better evaluate the factors associated with carotid atherosclerosis at baseline, the population was divided into two groups: low to moderate atherosclerosis (types I, IIa, IIb, and IVa findings in ultrasound) and high risk (types III and IVb) (Table 1).
 Click to view | Table 1. Baseline Characteristics of All Subjects by Risk Groups |
Figures 1 and 2 show the percentile curves of TPA in men and women by age group (20 - 65 years).
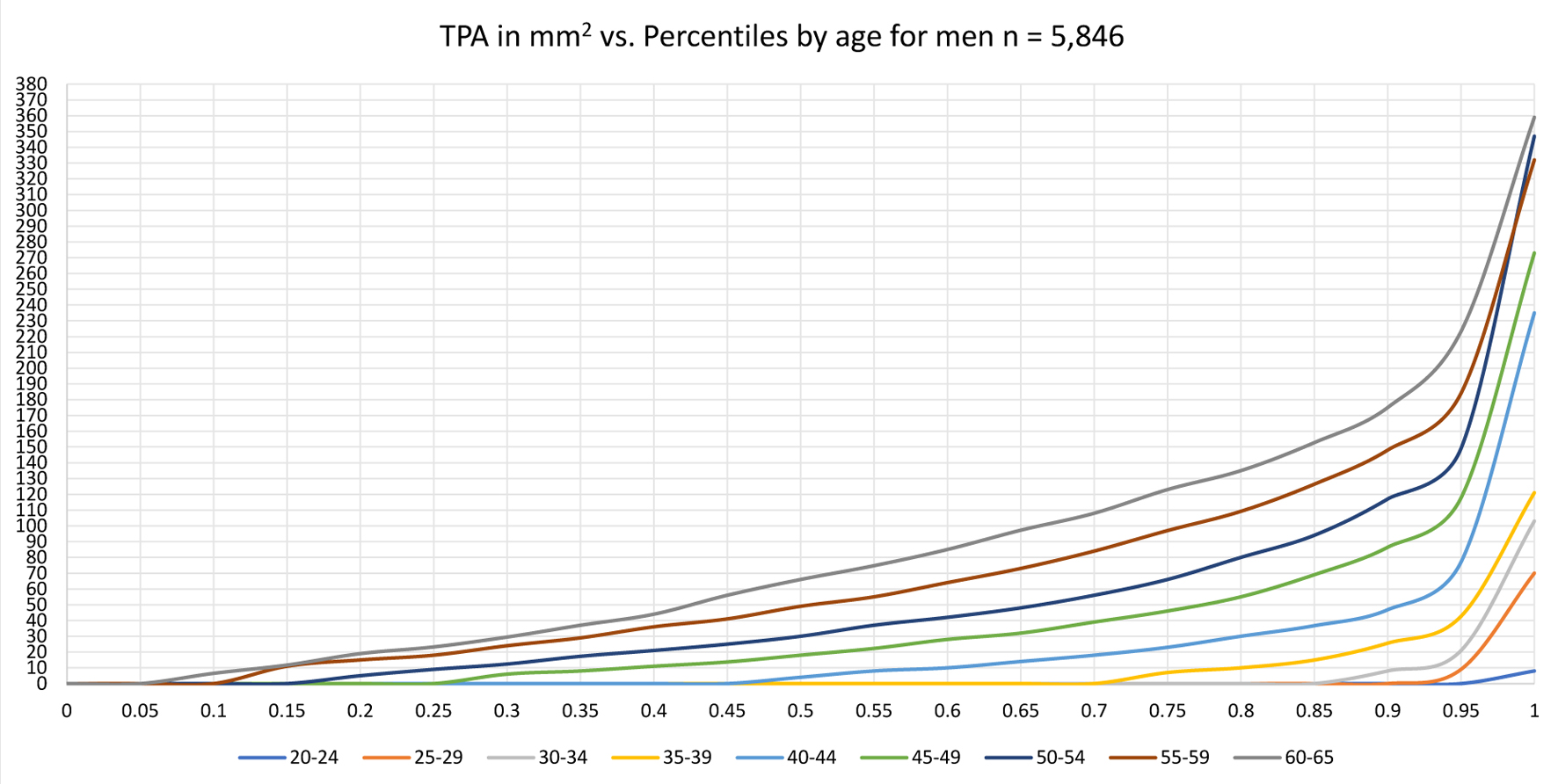 Click for large image | Figure 1. TPA percentiles by age for men. TPA: total plaque area. |
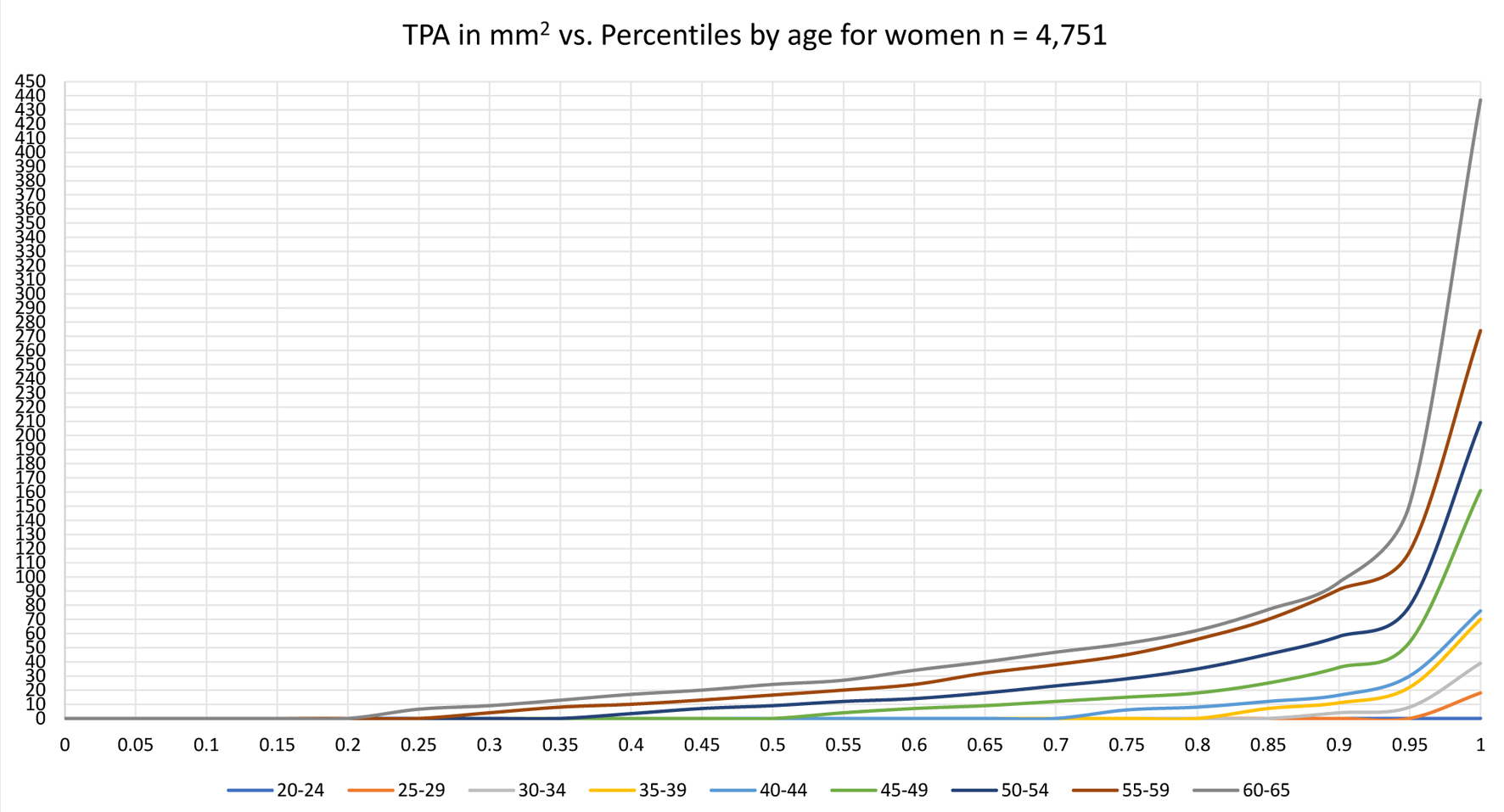 Click for large image | Figure 2. TPA percentiles by age for women. TPA: total plaque area. |
In the age group 25 - 65 years, 5,672 men and 4,652 women were examined.
The proportion of men and women with advanced arteriosclerosis (types III and IVb) is shown in Figure 3. Five hundred eighty-four (10.3%) men and 180 (3.9%) women have advanced atherosclerosis type III/IVb.
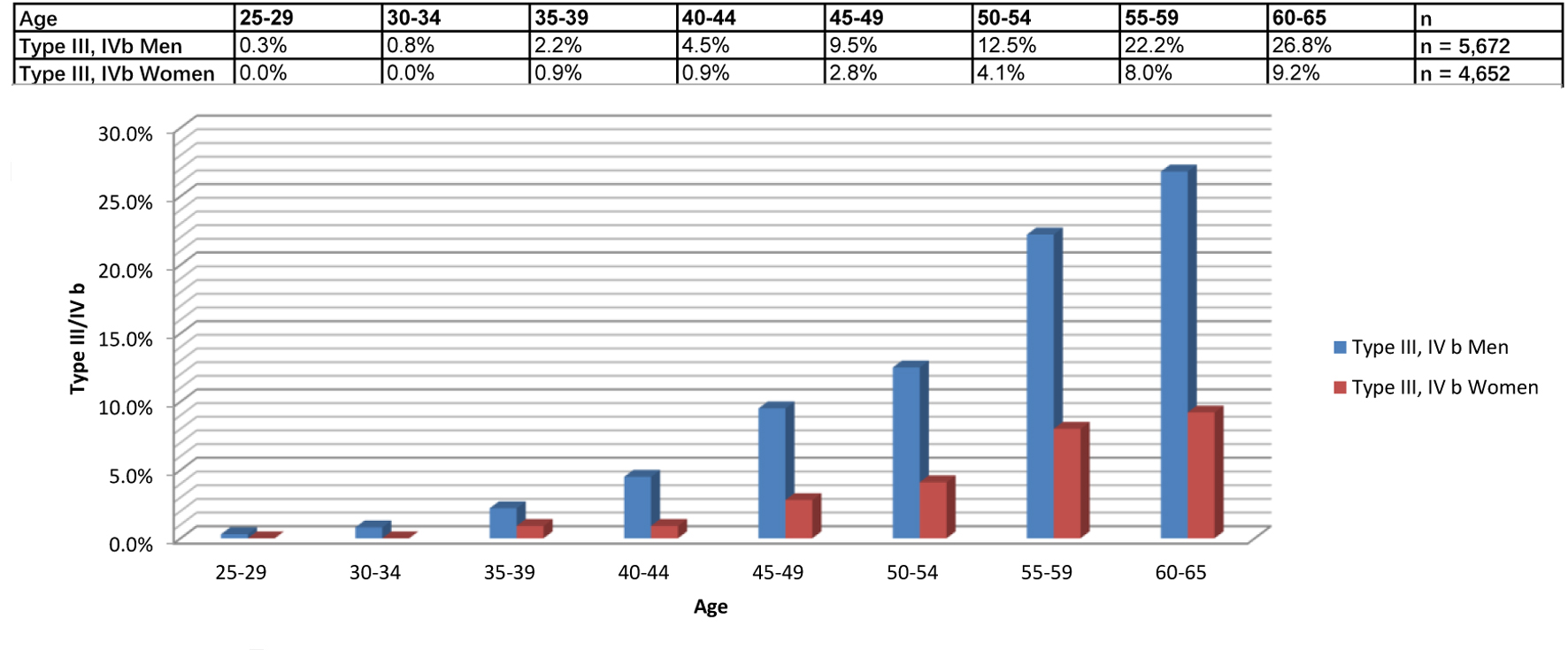 Click for large image | Figure 3. Proportion of men and women with advanced atherosclerosis. |
In the age group of 40 - 65 years, 2,592 men and 1,928 women were followed up.
Low to moderate atherosclerosis (types I, IIa, IIb, and IVa findings in ultrasound) was present in 2,052 (79.2%) men and 1,761 (91.3%) women. During follow-up, 139 (6.8%) men and 39 (2.0%) women developed advanced atherosclerosis type III or IVb (Tables 2-4), which could not be predicted by the classic risk factors (P > 0.05). The mean follow-up time was 73 months (6.3 years) for men and 75 months (5.8 years) for women.
 Click to view | Table 2. Proportion of Men With Progression to High Plaque Risk |
 Click to view | Table 3. Proportion of Women With Progression to High Plaque Risk |
 Click to view | Table 4. Proportion of Men and Women With Progression to High Plaque Risk by Age Group |
Patients with cancer and a cardiovascular event have a significantly higher risk profile and greater plaque burden than men without cancer or cardiovascular events (Tables 5 and 6), whereas patients with cancer and cardiovascular events have a very similar risk profile and plaque burden (Table 7). The following cancers have occurred: nine bronchial, six colon, two bladder, three brain, four stomach, two renal, three pancreas, 17 prostate, one base of the tongue, one esophagus, four unknown, one gallbladder, one larynx, and one lymphoma.
 Click to view | Table 5. Comparison of Risk Factors in Men With Cancer and Without Cancer, CVD |
 Click to view | Table 6. Comparison of Risk Factors in Men With CVD and Without Cancer, CVD |
 Click to view | Table 7. Comparison of Risk Factors in Men With CVD and With Cancer |
| Discussion | ▴Top |
Atherosclerosis is an inflammatory disease of the arteries and remains the most common cause of death in industrialized nations. The first plaques can be found in men at the age of 24 and in women at the age of 26. There are men and women in every age group who already have advanced atherosclerosis, which is associated with a high risk of cardiovascular disease [10]. This proportion increases with age. This means that in every age group, there is a further proportion of test subjects who develop rapid progression of atherosclerosis within a few years. It can be seen that the expected percentage of subjects with rapid progression of the disease is in good agreement with the actual percentage (Table 4). For example, in the age group of 40 - 44 years, 4.5% of men have advanced atherosclerosis types III and IVb; in the age group of 45 - 49 years, it is already 9.5%. It is therefore to be expected that approximately 4% of men in the age group of 40 - 44 years have a rapid progression of atherosclerosis and switch to high risk. In this group, 477 subjects with a low-medium risk of plaque (types I, IIa, IIb, and IVa) were followed up. Of the 477 subjects, 24 (5%) developed rapid progression. Who is affected cannot be predicted with the classic risk factors (all P-values > 0.05 except for systolic blood pressure P < 0.05 in men). This is probably also the reason why the classic risk scores only work to a very limited extent [11, 12].
It is therefore important to look at the disease and not just the classic risk factors. As advanced or rapidly progressing atherosclerosis is associated with a high risk of cardiovascular disease, which can be significantly reduced with early treatment with a statin, it is useful to measure the plaque burden on the carotid artery with ultrasound in men and women from the age of 35 or 45 and to repeat this examination after 3 - 5 years, so that test subjects with rapid progression of atherosclerosis are not overlooked. The examinations are offered to employees at companies every 3 years. This means that employees are examined without selection, but unfortunately not all of them. Participation in the study is voluntary. Therefore, the follow-up is not complete. In some companies, the examination only took place once.
In addition, there is evidence that advanced atherosclerosis and microvascular dysfunction are not only associated with an increased risk of cardiovascular events, but also with an increased risk of cancer [2-10]. Men with cancer and cardiovascular events show a very similar risk profile and a significantly increased plaque burden compared to men without events (Tables 5-7). Microvascular dysfunction probably affects not only the prearterioles and arterioles of the coronary vessels, but also other organs [13, 14].
Structural (obstruction and perivascular fibrosis) and functional changes (increased vascular tone caused by increased production of endothelin, prostacyclin, peptide Y or decreased production of nitric oxide NO) occur [1]. Hypoxia affects the proliferation and expression of the genes hypoxia-inducible factor-1-alpha (HIF-1α) and JMJD1A in head and neck tumor cells [8]. Natural killer (NK) cells are the first line of defense against infections and cancer cells. Hypoxia upregulates the transcription factor-1α (HIF-1α), which slows down the activity of NK cells in tumor defense [15]. Rashid et al consider HIF-1α to be an important transcription factor in cancer development. Hypoxia acts as an overarching driver and master regulator of cancer development [16].
Haverich and Boyle have written a very interesting book on atherosclerosis pathogenesis and microvascular dysfunction [17]. There is a physiological growth process of the intima starting with 1 - 2 cell layers at birth to 25 - 30 layers at the age of 25 - 30 years. The thin-walled arteries are supplied by diffusion from the lumen. From a critical thickness of 29 lamellae, hypoxic conditions occur in the media and adventitia, triggering angiogenic processes and the formation of vasa vasorum. The vasa vasorum supply the medium and large arteries with nutrients and oxygen from the outside to the inside. Disturbed perfusion of the vasa vasorum leads to neovascularization and immature endothelial structures, which promote the deposition of atherogenic substances and the supply of inflammatory cells and ultimately plaque formation. Atherosclerosis is initiated by impaired microcirculation. Hypertension, smoking, and reduced physical activity are risk factors for the development of functional and structural changes in the prearterioles and arterioles. Hypoxia occurs in the affected organs. Plaque formation occurs in the large and medium-sized arteries (coronary vessels, aorta, carotid artery, and femoral artery are seen as an organ), coronary microvascular dysfunction in the heart leads to a reduction in the coronary flow reserve, and in other organs, microvascular-induced hypoxia may downregulate the immune system, thereby slowing down tumor defense. In addition, there is evidence that there is a connection between neurodegenerative diseases such as glaucoma and Alzheimer’s and impaired microcirculation [18].
Impaired microcirculation could be the key to cardiovascular events and certain cancers and thus premature death.
The good news is that treatment, or prevention, is simple and costs little to nothing compared to later treatment: smoking cessation, 30 min of aerobic endurance training at least three times/week, early treatment of hypertension, and statin therapy for advanced atherosclerosis. There are numerous studies that describe the positive influence of endurance training for the prevention of several types of solid cancer (e.g., bowel, prostate, breast) and cardiovascular diseases [19, 20]. Improved microcirculation through endurance training could explain the positive preventive effect for both disease groups.
Carotid screening with ultrasound opens up a very good opportunity for the prevention of cardiovascular diseases and possibly also cancer.
Conclusion
Ultrasound examination of the carotid artery can identify people with advanced atherosclerosis. A follow-up examination with low or moderate plaque burden after 3 - 5 years is useful, so that subjects with rapid progression of atherosclerosis can be detected at an earlier stage. Early treatment of advanced atherosclerosis improves the prognosis for cardiovascular diseases and possibly also for certain types of cancer.
Limitations
The follow-up in the group with low and medium risk ultrasound in men and women is only 54%. The examinations are offered to employees at companies every 3 years. This means that employees are examined without selection, but unfortunately not all of them. Therefore, the follow-up is not complete. In some companies, the examination only took place once. In total, 1,494 men (42.1%) and 1,684 women (48.9%) were not followed up.
This number is high and may lead to bias, but there is no significant statistical difference between subjects with or without follow-up (Table 8).
 Click to view | Table 8. Baseline Characteristics for All Subjects With Low and Intermediate Risk With and Without Follow-Up |
The link between microvascular dysfunction and certain types of cancer is a hypothesis and needs to be confirmed by further studies.
Acknowledgments
None to declare.
Financial Disclosure
This study has not been supported by any external funding.
Conflict of Interest
The authors confirm that they have no conflict of interest.
Informed Consent
All patients provided informed consent.
Author Contributions
WB and MR discussed the approach and the findings of this study with AA intensively and gave AA valuable feedback. All examinations have been done by AA.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Ullrich-Daub H, Daub S, Olschewski M, Munzel T, Gori T. Diseases of the coronary microcirculation: diagnosis and treatment. Dtsch Arztebl Int. 2023;120(44):739-746.
doi pubmed - Toya T, Sara JD, Corban MT, Taher R, Godo S, Herrmann J, Lerman LO, et al. Assessment of peripheral endothelial function predicts future risk of solid-tumor cancer. Eur J Prev Cardiol. 2020;27(6):608-618.
doi pubmed - Rajai N, Ahmad A, Toya T, Sara JD, Herrmann J, Lerman LO, Lerman A. Coronary microvascular dysfunction is an independent predictor of developing cancer in patients with non-obstructive coronary artery disease. Eur J Prev Cardiol. 2023;30(3):209-216.
doi pubmed - Roubin SR, Cordero A. The two-way relationship between cancer and atherosclerosis. Revista Espanola de Cardiologia (English Edition). 2019;72(6):487-494.
- Li J, Zhao J, Lei Y, Chen Y, Cheng M, Wei X, Liu J, et al. Coronary atherosclerotic disease and cancer: risk factors and interrelation. Front Cardiovasc Med. 2022;9:821267.
doi pubmed - Adams A, Bojara W, Romanens M. Relationship between atherosclerosis and cancer: an observational outcome study. Imaging J Clin Medical Sci. 2022;9(1):001-006.
doi - Nebigil CG, Chan MWY. Editorial: HF2Cancer: Exploring bidirectional interaction between cardiovascular diseases and cancer. Front Cardiovasc Med. 2023;10:1145780.
doi pubmed - Gallucci G, Turazza FM, Inno A, Canale ML, Silvestris N, Fari R, Navazio A, et al. Atherosclerosis and the bidirectional relationship between cancer and cardiovascular disease: from bench to bedside-Part 1. Int J Mol Sci. 2024;25(8):4232.
doi pubmed - Wilhelm C, Hackenberg S, Kleinsasser N, Scherzad A. Einfluss von Hypoxie auf Proliferation und Expression der Gene HIF-1α und JMJD1A in Kopf-Hals-Tumorzellen. Laryngo-Rhino Otologie. 2018;97(S02):10090.
- Adams A, Bojara W, Romanens M. Ultraschalluntersuchung der A. carotis zur verbesserten Vorhersage kardiovaskularer Ereignisse und der Wirkung einer Statinbehandlung bei fortgeschrittener Atherosklerose. Herz. 2024;49:60-68.
- Romanens M, Mortensen MB, Sudano I, Szucs T, Adams A. Extensive carotid atherosclerosis and the diagnostic accuracy of coronary risk calculators. Prev Med Rep. 2017;6:182-186.
doi pubmed - Romanens M, Adams A, Wenger M, Warmuth W, Sudano I. Prognostic impact of carotid plaque imaging using total plaque area added to SCORE2 in middle-aged subjects: the ARteris Cardiovascular Outcome (ARCO) cohort study. Swiss Med Wkly. 2024;154:3735.
doi pubmed - Xu C, Sellke FW, Abid MR. Assessments of microvascular function in organ systems. Am J Physiol Heart Circ Physiol. 2022;322(6):H891-H905.
doi pubmed - Feuer DS, Handberg EM, Mehrad B, Wei J, Bairey Merz CN, Pepine CJ, Keeley EC. Microvascular dysfunction as a systemic disease: a review of the evidence. Am J Med. 2022;135(9):1059-1068.
doi pubmed - Ni J, Wang X, Stojanovic A, Zhang Q, Wincher M, Buhler L, Arnold A, et al. Single-cell RNA sequencing of tumor-infiltrating NK cells reveals that inhibition of transcription factor HIF-1alpha unleashes NK cell activity. Immunity. 2020;52(6):1075-1087.e1078.
doi pubmed - Rashid M, Zadeh LR, Baradaran B, Molavi O, Ghesmati Z, Sabzichi M, Ramezani F. Up-down regulation of HIF-1alpha in cancer progression. Gene. 2021;798:145796.
doi pubmed - Haverich A, Boyle EC. Atherosklerose-Pathogenese und mikrovaskuläre Dysfunktion. Springer. 2023.
- Mroczkowska S, Shokr H, Benavente-Perez A, Negi A, Bentham P, Gherghel D. Retinal microvascular dysfunction occurs early and similarly in mild Alzheimer's disease and primary-open angle glaucoma patients. J Clin Med. 2022;11(22):6702.
doi pubmed - Patel AV, Friedenreich CM, Moore SC, Hayes SC, Silver JK, Campbell KL, Winters-Stone K, et al. American College of Sports Medicine Roundtable Report on physical activity, sedentary behavior, and cancer prevention and control. Med Sci Sports Exerc. 2019;51(11):2391-2402.
doi pubmed - Porter AK, Schilsky S, Evenson KR, Florido R, Palta P, Holliday KM, Folsom AR. The association of sport and exercise activities with cardiovascular disease risk: the atherosclerosis risk in communities (ARIC) study. J Phys Act Health. 2019;16(9):698-705.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.