| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 16, Number 6, December 2025, pages 525-532
Total Regurgitant Fraction to Predict Aortic Valve Surgery in Patients With Concomitant Aortic and Mitral Regurgitation
Alvaro Montesa, Alberto Cecconia, i, Albert Teisb, Juan Lacalzada-Almeidac, Beatriz Lopez Melgara, Paloma Caballerod, Susana Hernandez Munizd, Carmen Benavidesd, Dafne Vilianie, Mauro Di Silvestrec, Cesar Jimenez Mendezf, Maria Manuela Izquierdo-Gomezc, Flor Baeza Garzonc, Claudia Escabiab, Fernando Alfonsoa, g, h, Luis Jesus Jimenez-Borregueroa, f
aCardiology Department, University Hospital of La Princesa, Madrid, Spain
bCardiology Department, Institut del Cor. Hospital Germans Trias i Pujol Hospital, Badalona, Spain
cCardiology Department, University Hospital of the Canaries, Santa Cruz De Tenerife, Spain
dRadiology Department, University Hospital of La Princesa, Madrid, Spain
eCardiology Department, Santa Chiara Hospital in Trento, Trento, Italy
fCardiology Department, University Hospital Puerta del Mar, Cadiz, Spain
gCentro de Investigacion Biomedica en Red de Enfermedades Cardiovasculares (CIBERCV), Madrid, Spain
hIIS-IP, Universidad Autonoma de Madrid, Madrid, Spain
iCorresponding Author: Alberto Cecconi, Cardiology Department, University Hospital of La Princesa, Madrid, Spain
Manuscript submitted June 29, 2025, accepted September 27, 2025, published online December 20, 2025
Short title: TRF and Surgery Risk in Patients With CAMR
doi: https://doi.org/10.14740/cr2068
| Abstract | ▴Top |
Background: Concomitant aortic and mitral regurgitation (CAMR) is associated with poorer outcome compared with isolated aortic regurgitation (AR). Current prognostic assessment of AR does not include the magnitude of mitral regurgitation (MR). Cardiac magnetic resonance (CMR) can integrate volumetric data to obtain a novel combined parameter, total regurgitant fraction (TRF), which could have the potential ability to measure the combined effects of AR and MR on left ventricle (LV) overload. The aim of our study was to explore the usefulness of TRF in predicting the future need of aortic valve surgery in patients with CAMR.
Methods: Patients with CAMR and prior CMR studies were retrospectively recruited. A total of 45 patients were included, of whom 10 (22%) developed surgery indications. At the median follow-up time point (3.2 years), survival without surgery indication was 95% in the group with TRF < 40% compared to 90% in the group with aortic regurgitant fraction (ARF) < 29%. In contrast, 67% of patients with TRF ≥ 40% developed surgery indications after 3.2 years compared to 55% of patients with ARF ≥ 29%. In the multivariate analysis, the model including binary TRF had the highest hazard ratio of 13.846 (2.822 to 67.939, P = 0.001).
Conclusions: TRF is a promising CMR parameter that could improve the prediction of the need for surgery in patients with CAMR. Further studies with larger populations should be performed to confirm these findings.
Keywords: Aortic regurgitation; Mitral regurgitation; Cardiac magnetic resonance; Total regurgitation fraction
| Introduction | ▴Top |
Chronic aortic regurgitation (AR) and mitral regurgitation (MR) are common valvular heart diseases that can lead to heart failure. Both conditions are associated with left ventricle (LV) enlargement and dysfunction secondary to diastolic volume overload. Concomitant aortic and mitral regurgitation (CAMR) is not uncommon, with a prevalence of moderate or severe MR in 14-25% of patients with moderate or severe AR. This coexistence is associated with poorer outcomes compared with isolated AR [1, 2].
When both regurgitations are concomitant, the overload of the LV is conditioned by the excess of volume produced by the sum of the aortic regurgitant volume (ARV) and mitral regurgitant volume (MRV). However, current prognostic assessment of AR does not consider the presence and magnitude of concomitant MR. As a result, there are no specific recommendations for management of patients with these combined valvular regurgitations [3]. Therefore, in patients with CAMR, we may underestimate the risk of cardiac remodeling and cardiac events and, possibly, delaying the optimal timing for valve surgery.
There is evidence that ARV and aortic regurgitant fraction (ARF), calculated by cardiac magnetic resonance (CMR), are powerful predictors of outcome in patients with AR [4-6]. Moreover, there is growing evidence supporting MRV and mitral regurgitant fraction (MRF), also calculated by CMR, as the most accurate parameters to assess MR severity [7, 8]. Indeed, CMR is used as a highly reliable method to separately calculate the regurgitation fractions of the aortic and mitral valves. In patients with CAMR, data from cine and velocity-encoded phase contrast (VEPC) imaging could be integrated by adding the ARV and MRV to obtain combined parameters as total regurgitant volume (TRV) and total regurgitant fraction (TRF), as depicted in Figure 1.
 Click for large image | Figure 1. Obtention of the mentioned volumes and regurgitant fractions in velocity encoding phase contrast imaging (left) and its schematic representation in left cardiac chambers. ARF: aortic regurgitant fraction; ARV: aortic regurgitant volume, FV: forward volume; LA: left atrium; LVEDV: left ventricular end-diastolic volume; LVESV: left ventricular end-systolic volume; LVSV: left ventricular stroke volume; MRF: mitral regurgitant fraction; MRV: mitral regurgitant volume; TRF: total regurgitant fraction; TRV: total regurgitant volume; VR: venous return. |
TRV and TRF have not been previously described or evaluated in this scenario. These novel parameters could have the potential to measure the combined effects of AR and MR on LV overload and, therefore, have a prognostic value in patients with CAMR.
Against this background, the aim of our study was to explore the usefulness of CMR-calculated TRF in predicting the future need for aortic valve surgery in patients with CAMR, and to compare it with the established conventional assessment of evaluating solely ARF, without considering the mitral regurgitant volume.
| Materials and Methods | ▴Top |
Study population and outcome
Consecutive patients aged 18 years or older with concomitant moderate or severe AR and any grade of MR diagnosed by standard transthoracic echocardiography (TTE) assessment were retrospectively recruited from three tertiary centers: Hospital Universitario de La Princesa (Madrid) which acted as the coordinating center, Hospital Universitario Germans Trias i Pujol (Badalona) and Complejo Hospitalario Universitario de Canarias (La Laguna, Santa Cruz de Tenerife). The study was approved by the Institutional Review Board (approval number 4131) (Supplementary Material 1, cr.elmerpub.com) of the recruiting centers according to the Spanish legislation.
Exclusion criteria were: 1) previous history of severe aortic or mitral stenosis, LV dysfunction or other cardiomyopathy, including cardiac or extracardiac shunts; 2) formal indication at enrollment of valve surgery according to European Society of Cardiology (ESC)/European Association for Cardio-Thoracic Surgery (EACTS) clinical practice guidelines [3]; 3) history of previous cardiac surgery; and 4) indication of valve surgery due to other reason (such as aortic aneurysm).
The primary endpoint was defined as the development of any current ESC/EACTS practice guideline-based indication of aortic valve surgery due to AR, including symptomatic severe AR, severe LV dilatation (LV end-diastolic diameter > 70 mm or LV end-systolic diameter > 50 mm), or reduced (< 50%) left ventricular ejection fraction (LVEF) during follow-up.
Clinical and TTE characteristics were collected at each center at the closest time within 6 months prior to the first eligible CMR. CMR studies were anonymized and centrally analyzed in a core CMR lab by expert personnel blinded to clinical and echocardiographic data. In patients with more than one CMR, the first eligible study was used as baseline for the analysis. If the CMR results constituted an indication for surgery, the patient was removed from the analysis.
Patients were clinically followed with reassessment of LV diameters, volumes and function mainly by TTE at local sites following clinical guidelines recommendations [3].
CMR protocol
CMR images were performed on 1.5 T clinical scanners. The CMR data acquisition protocol is described (Supplementary Material 2, cr.elmerpub.com). Sequences were performed as described in expert consensus statements [9, 10].
Quantitation of LV and regurgitation parameters with CMR
Ventricular volumes and ejection fraction were quantified in the short-axis cine stack of steady-state free precession (SSFP) cine images using Circle Cardiovascular Imaging (cvi42). Papillary muscles were included in the LV blood volume. Left ventricular stroke volume (LVSV) was calculated by Simpson method as the difference between LV end-diastolic volume (LVEDV) and end-systolic volume (LVESV).
ARV and ARF were quantified in phase-contrast (PC) sequences, as shown in Figure 1. The following volumetric parameters are also represented: MRV was calculated as the difference between LVSV and aortic PC forward volume (FV). MRF was calculated as MRV divided by LVSV minus ARV, as recommended in current valvular regurgitation guidelines and state of the art reviews [8, 11]. TRV was calculated as ARV plus MRV. TRF was calculated as TRV divided by LVSV.
Statistical analysis
Basic statistical analyses are described here (Supplementary Material 3, cr.elmerpub.com).
Receiver operating characteristic (ROC) curve and corresponding area under the curve (AUC) were used to determine the sensitivity and specificity of CMR valve regurgitation. AUC differences between parameters were compared with DeLong’s test. Best cutoff point to predict the indication for aortic valve intervention at 1, 2 and 3 years of follow-up was calculated using the method of Youden. Kaplan-Meier (KM) analysis was performed, and the log-rank test was used for variables with the best discriminatory ability in the ROC analysis.
Initially, univariable Cox proportional hazards regression was used to examine the association between the regurgitation variables and the primary clinical endpoint events. Subsequently, significant associations were adjusted using multivariable analysis. Variables which showed trend towards statistically significant differences (P < 0.10) between the two groups at baseline were included in the model, while variables with collinearity were omitted.
Statistical analysis was performed with IBM SPSS Statistics, version 25.
| Results | ▴Top |
A total of 45 patients with concomitant moderate or severe AR and any grade of MR were included in the study. During a mean time of 3.9 years, 10 patients (22%) developed surgery indications and were intervened: nine underwent isolated aortic valve replacement, and one underwent mitral and aortic valve replacement.
The main clinical baseline characteristics are summarized in Table 1. No significant differences were found between groups concerning clinical characteristics. The mean age was 61.5 years. Numerically, there were more men and patients with dyslipidemia and chronic kidney disease in the valve surgery group, but the differences were not statistically significant. All patients were free of symptoms related to their valvular disease at the beginning of follow-up.
 Click to view | Table 1. Main Clinical Baseline Characteristics |
AR was due to bicuspid aortic valve (BAV) in 21 patients (46.7%), degenerative in 12 patients, and functional in eight patients. In four patients, the underlying etiology of AR was unclear. Nineteen patients had organic MR, nine functional and one mixed. In 16 patients, the etiology of the MR was unclear.
Indications of surgery were due to the development of symptoms in seven patients (70%), severe LV dilatation in one patient (10%), and reduced LVEF in two patients (20%).
One patient in the non-surgery indication group died during follow-up, due to neurological complications from a severe status epilepticus.
CMR findings are displayed in Table 2. Patients in the surgery indication group had significant higher MRF (21.6±9.8% vs. 14.9±7.9%), ARV (32.2 ± 14.6 mL vs. 20.3 ± 11.8 mL), ARF (29.5±10.1% vs. 21.0±8.1%), TRV (50.7 ± 19.0 mL vs. 33.2 ± 16.8 mL) and TRF (41.2±9.4% vs. 30.4±9.2%) at baseline, as compared to patients without surgery indications. MRV was higher in the surgery indication group but did not reach statistical significance. However, LVEDV and LVESV were similar in both groups. Due to the acquisition angle of PC sequences, descendent aorta flow reversal (DAFR) analysis was feasible in only 29 patients. All patients with surgery indications had DAFR.
 Click to view | Table 2. Comparison Between Patients Without and With Surgery Indication During Follow-Up |
ROC curve data of CMR regurgitation parameters with reasonable significant discriminatory ability (AUC > 0.70, P < 0.05) are shown in Table 3, with ARF and TRF having the highest AUC values. ROC curves comparing ARF and TRF to predict the development of surgery indications at 1, 2, 3 years and at the end of follow-up are plotted in Figure 2. Although TRF had a trend towards superiority compared to ARF, the difference between both parameters did not reach the statistical signification in DeLong’s test (P = 0.67).
 Click to view | Table 3. ROC Data (Comparison of the Ability of Each Parameter to Identify the Patients Who Develop Indications for Surgery at the End of Follow-Up) |
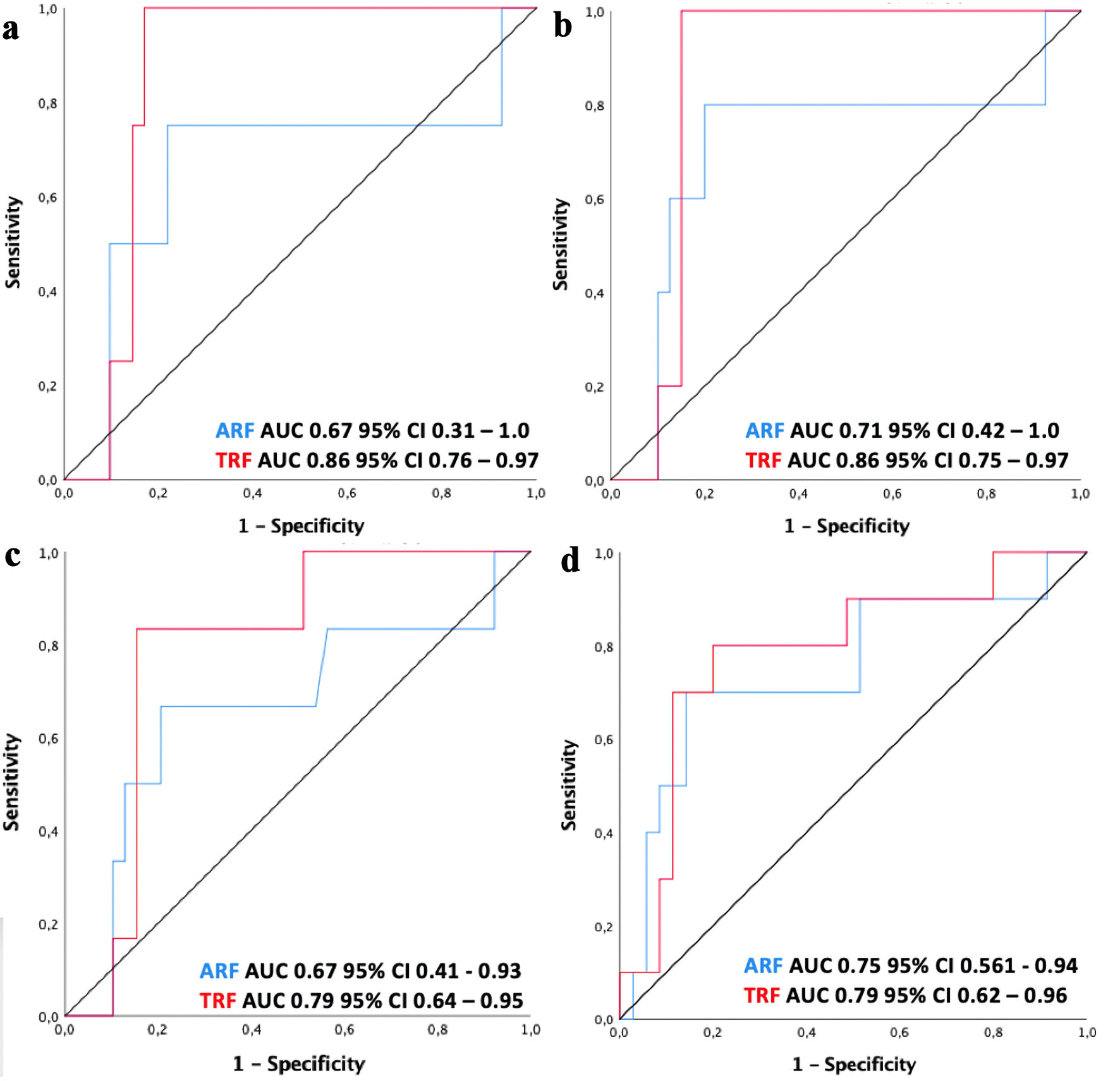 Click for large image | Figure 2. ROC curve representing capacity of ARF (blue line) and TRF (red line) to identify patients at risk of developing surgery indications at 1 year (a), 2 years (b), 3 years (c) and at the end of follow-up (d). ARF: aortic regurgitant fraction; TRF: total regurgitant fraction; CI: confidence interval; AUC: area under the curve; ROC: receiver operating characteristic. |
KM curves were built stratified by ARF and TRF cut-offs and are represented in Figure 3. There was a progressive and significant separation of the groups over time (ARF ≥ 29% log rank P = 0.001, TRF ≥ 40% log rank P = 0.000). At the median follow-up time point (3.2 years), survival without surgery indication was 95% in the group with TRF < 40% compared to 90% in the group with ARF < 29%. In contrast, 67% of patients with TRF ≥ 40% developed surgery indications after 3.2 years compared to 55% of patients with ARF ≥ 29%.
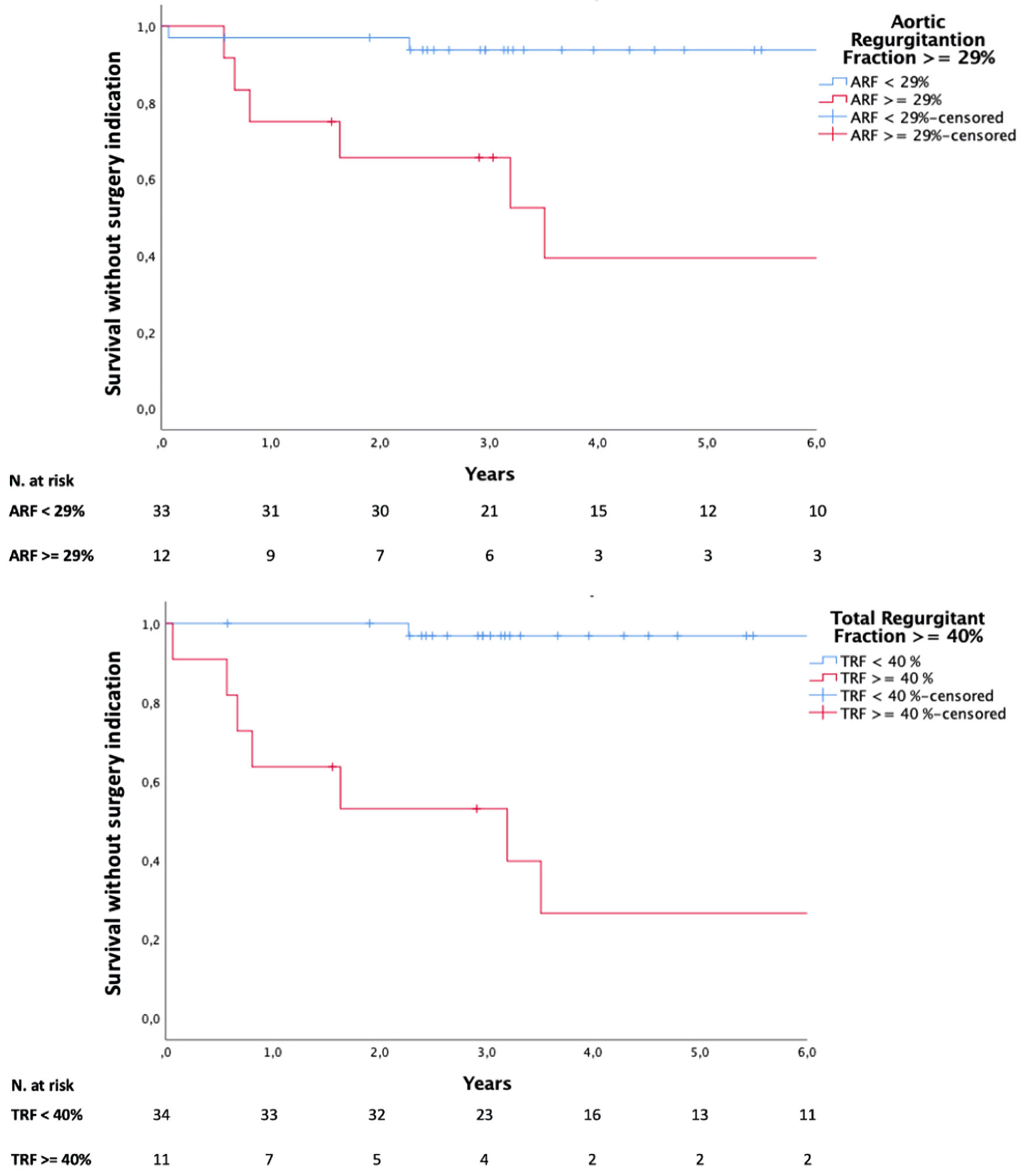 Click for large image | Figure 3. Surgery-indication free survival by ARF (superior panel) and TRF (inferior panel) best cut-offs determined by Youden method in ROC analysis. ARF: aortic regurgitant fraction; TRF: total regurgitant fraction; ROC: receiver operating characteristic. |
Binary Cox regression analyses comparing groups above and below thresholds identified on ROC analysis are depicted in Table 4. Hazard ratio for TRF was the highest: 15.802 (3.256 to 76.692, P = 0.001). Multivariate Cox regression analysis was adjusted for LVEF, the only covariable which showed a trend towards statistically significant differences between groups and had no collinearity. Regurgitant volumes, regurgitant fractions and left ventricular volumes were not included in the same model due to significant collinearity. DAFR was not included in the model due to missing values in the cohort. The model including binary TRF had the highest hazard ratio: 13.846 (2.822 to 67.939, P = 0.001), as shown in Table 4.
 Click to view | Table 4. Cox Proportional Hazard Regression for the Variables With Significant Discriminatory Ability on ROC Analysis |
Six patients (11.3%) had dilated ascending aorta (DAA), defined as an aortic diameter divided for corporal surface ≥ 21. A subgroup analysis was performed including patients with and without DAA. In patients with DAA, none of the parameters reached a significant AUC. In patients without DAA, TRF had an AUC of 0.84 (with 95% confidence interval (CI) of 0.52 - 0.97, P = 0.003), compared to ARF AUC of 0.75 (with 95% CI of 0.70 - 0.97, P = 0.028), but the difference between both AUCs did not reach statistical signification (P = 0.43).
| Discussion | ▴Top |
Our data demonstrate the potential prognostic value of quantifying TRF with CMR in patients with CAMR. Importantly, these novel CRM parameters showed a significant association with the future need for valve surgery.
CMR-measured ARV-ARF [4-6] and MRV-MRF [7, 8] have proved to be reliable and accurate parameters for separately quantifying AR and MR. Nevertheless, this evidence was based on studies that excluded patients with CAMR. Therefore, there was a lack of data regarding the usefulness of these parameters in patients with CAMR. Our study aimed to mend this gap in evidence and also to evaluate TRF, a novel quantitative parameter with capacity to measure the combined effect of both valvular heart diseases, and its predictive and prognostic value.
The proposed ARF cut-off for severity in our study of 29% is lower than previously described [4, 5, 12]. This suggests that conventional thresholds for evaluating ARF alone in patients with CAMR may have reduced sensitivity to detect patients at risk of developing surgical indications. In fact, conventional ARF threshold of 33% had a sensitivity of 40% in our CAMR cohort.
As pointed by Vejpongsa et al [12], a significant proportion of patients with AR who undergo surgery present an ARF below the TTE-based thresholds for severity of 50%. In concordance with previous studies, CMR-quantified ARF cut-offs in our cohort are also lower than current TTE-based thresholds, lending support to the more accurate prognostic value of CMR-quantified regurgitation fractions.
The capability of TRF to predict the development of surgery indications was higher (AUC 0.79, P = 0.006) compared to ARF (AUC 0.75 P = 0.018), but the difference between the two parameters did not reach the statistical signification (P = 0.67), probably due to the limited number of patients. TRF had a similar sensitivity (70%) but higher specificity (89% vs. 85%) compared to ARF. In our study, the mean MRF was 16.4%, which corresponds to mild-to-moderate MR. This might explain the slight difference between TRF and ARF. It is likely that in patients with more severe MR, TRF could have even better prognostic capability than ARF alone.
Survival without surgery indication at the median follow-up time point (3.2 years) was 95% in the group with TRF < 40%, compared to 90% in the group with ARF < 29%. In contrast, 67% of patients with TRF ≥ 40% developed surgery indications after 3.2 years, compared to 55% of patients with ARF ≥ 29%. The hazard ratios of patients with TRF ≥ 40% were also higher (15.8 and 13.8 in univariate and multivariate analyses, respectively) than those of patients with ARF ≥ 29% (6.9 and 5.4 in univariate and multivariate analyses, respectively), identifying TRF as the best independent predictor of the need for surgery in our population.
To the best of our knowledge, this is the first attempt to describe TRF as a concept and therefore to demonstrate its prognostic and predictive value in patients with CAMR. This could help identify patients with CAMR who are more likely to require aortic valve surgery in the future, thereby allowing for closer clinical monitoring.
Unlike other studies, LVEDV and LVESV were not independent predictors of surgery in our cohort. Myerson et al [4] found that after a median follow-up of 21 months, 35% of patients developed an indication for surgery. These patients had a mean LVEDV and LVESV values of 301 and 113 mL, respectively. Postigo et al [5] described an incidence of 39% after a median follow-up of 33 months. Full cohort LVEDV and LVESV values were 213 and 87 mL in this study. Compared with these populations, our patients had lower ventricular volumes and a lower proportion of events (22%). This suggests that in our study, CMR was performed at an earlier stage of remodeling and thus, LVEDV and LVESV had a limited predictive value in these patients.
A significant percentage (46.7%) of patients had BAV. At the participating centers, most CMR were indicated due to difficulties in evaluation with convectional echocardiographic criteria in such patients. This reflects the real clinical practice in our environment and might explain why patients had baseline CMR performed at earlier stages compared to other studies. Nevertheless, results might differ in a prospective study where CMR is performed in a more representative, unselected population. Such a design would likely provide a more accurate estimate of the utility and diagnostic performance of TRF across the full spectrum of aortic insufficiency severity and etiologies.
Patients with DAA can present helical flow patterns at the level of the aortic root, with a theoretical risk of loss of precision in the quantification of volumes by conventional two-dimensional (2D) VEPC imaging due to its dependency on the flow intercept angle. In this scenario, four-dimensional (4D) flow imaging is believed to be more accurate than conventional 2D VEPC [13]. Nevertheless, there is discordant evidence in the literature regarding this matter [14], and more research is needed to establish the role of 4D flow imaging in patients with CAMR. However, trying to overcome this potential limitation, we performed a subgroup analysis of patients with and without DAA. Patients without DAA presented similar results to the entire cohort, with an AUC for TRF of 0.84 compared to AUC for ARF of 0.75, also with a trend towards superiority without reaching the statistical signification.
DAFR was present in all baseline CMR studies of patients who developed surgery indications, showing a high sensitivity, as previously described by Kammerlander et al [15]. Nevertheless, its specificity might be improved with additional quantitative measurements that, due to the acquisition angle of the PC sequences, were not feasible in our study.
Limitations
Our study has some limitations. Considering the sample size and the lack of significant differences with conventional ARF measurements, our results are inadequate to prove a significant benefit, should be considered as hypothesis-generating, and require confirmation in further studies including a larger population. In addition, most of the patients had MR with low grade of severity. Nevertheless, our hypothesis - that the measurement of LV overload of combined valvular regurgitant volumes and fractions is a better predictor of prognosis than the isolated measurement of the dominant valvulopathy, in our case AR - is highly appealing from a pathophysiological standpoint. Therefore, our findings in this population with mild-to-moderate MR should be reproduced in future larger studies including patients with more severe grades of MR.
Conclusions
TRF is a promising novel CMR parameter that may predict the need for surgery in patients with CAMR compared to ARF alone. Conventional CMR-calculated ARF thresholds may have some limitations to predict the need for surgery in patients with CAMR. Further studies with larger populations should be performed to confirm these findings. Moreover, our work adds evidence of the usefulness of CMR in a thorough evaluation of MR and AR. In this scenario, CMR should be considered as a first-line modality in future studies.
Acknowledgments
None to declare.
Financial Disclosure
The authors received no funding or grants for this work.
Conflict of Interest
None of the authors has any conflict of interest related to this work.
Informed Consent
Patient consent for publication was deemed unnecessary because the study does not involve identifiable human data.
Author Contributions
Conceptualization: J. Jimenez-Borreguero, A. Cecconi. Methodology: J. Jimenez-Borreguero, A. Cecconi, F. Alfonso, A. Montes. Project administration: J. Jimenez-Borreguero, A. Cecconi. Supervision: J. Jimenez-Borreguero, A. Cecconi, F. Alfonso. Data analysis: A. Montes, A. Cecconi. Data collection and CMR image adquisition: A. Montes, A. Cecconi, A. Teis, J. Lacalzada, B. Lopez Melgar, P. Caballero, S. Hernandez Muniz, C. Benavides, M. Di Silvestre, C. Jimenez Mendez, MM Izquierdo-Gomez, F. Baeza Garzon, C. Escabia. Manuscript original draft writing: A. Montes. Review and editing: all authors.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Yang LT, Enriquez-Sarano M, Scott CG, Padang R, Maalouf JF, Pellikka PA, Michelena HI. Concomitant mitral regurgitation in patients with chronic aortic regurgitation. J Am Coll Cardiol. 2020;76(3):233-246.
doi pubmed - Pai RG, Varadarajan P. Prognostic implications of mitral regurgitation in patients with severe aortic regurgitation. Circulation. 2010;122(11 Suppl):S43-47.
doi pubmed - Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561-632.
doi pubmed - Myerson SG, d'Arcy J, Mohiaddin R, Greenwood JP, Karamitsos TD, Francis JM, Banning AP, et al. Aortic regurgitation quantification using cardiovascular magnetic resonance: association with clinical outcome. Circulation. 2012;126(12):1452-1460.
doi pubmed - Postigo A, Perez-David E, Revilla A, Raquel LA, Gonzalez-Mansilla A, Prieto-Arevalo R, Espinosa MA, et al. A comparison of the clinical efficacy of echocardiography and magnetic resonance for chronic aortic regurgitation. Eur Heart J Cardiovasc Imaging. 2022;23(3):392-401.
doi pubmed - Harris AW, Krieger EV, Kim M, Cawley PJ, Owens DS, Hamilton-Craig C, Maki J, et al. Cardiac magnetic resonance imaging versus transthoracic echocardiography for prediction of outcomes in chronic aortic or mitral regurgitation. Am J Cardiol. 2017;119(7):1074-1081.
doi pubmed - Le Goffic C, Toledano M, Ennezat PV, Binda C, Castel AL, Delelis F, Graux P, et al. Quantitative evaluation of mitral regurgitation secondary to mitral valve prolapse by magnetic resonance imaging and echocardiography. Am J Cardiol. 2015;116(9):1405-1410.
doi pubmed - Uretsky S, Argulian E, Narula J, Wolff SD. Use of cardiac magnetic resonance imaging in assessing mitral regurgitation: current evidence. J Am Coll Cardiol. 2018;71(5):547-563.
doi pubmed - Schulz-Menger J, Bluemke DA, Bremerich J, Flamm SD, Fogel MA, Friedrich MG, Kim RJ, et al. Standardized image interpretation and post-processing in cardiovascular magnetic resonance - 2020 update : Society for Cardiovascular Magnetic Resonance (SCMR): Board of Trustees Task Force on Standardized Post-Processing. J Cardiovasc Magn Reson. 2020;22(1):19.
doi pubmed - Sutton DC, Kluger R, Ahmed SU, Reimold SC, Mark JB. Flow reversal in the descending aorta: a guide to intraoperative assessment of aortic regurgitation with transesophageal echocardiography. J Thorac Cardiovasc Surg. 1994;108(3):576-582.
pubmed - Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, Hahn RT, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the american society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance. J Am Soc Echocardiogr. 2017;30(4):303-371.
doi pubmed - Vejpongsa P, Xu J, Quinones MA, Shah DJ, Zoghbi WA. Differences in cardiac remodeling in left-sided valvular regurgitation: implications for optimal definition of significant aortic regurgitation. JACC Cardiovasc Imaging. 2022;15(10):1730-1741.
doi pubmed - Weigang E, Kari FA, Beyersdorf F, Luehr M, Etz CD, Frydrychowicz A, Harloff A, et al. Flow-sensitive four-dimensional magnetic resonance imaging: flow patterns in ascending aortic aneurysms. Eur J Cardiothorac Surg. 2008;34(1):11-16.
doi pubmed - Alvarez A, Martinez V, Pizarro G, Recio M, Cabrera JA. Clinical use of 4D flow MRI for quantification of aortic regurgitation. Open Heart. 2020;7(1):e001158.
doi pubmed - Kammerlander AA, Wiesinger M, Duca F, Aschauer S, Binder C, Zotter Tufaro C, Nitsche C, et al. Diagnostic and prognostic utility of cardiac magnetic resonance imaging in aortic regurgitation. JACC Cardiovasc Imaging. 2019;12(8 Pt 1):1474-1483.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.