| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 000, Number 000, June 2025, pages 000-000
Effect of Hyperperfusion on Successful Collection of Arterial Blood Gas Specimens in Patients With Acute Heart Failure
Mei Zhanga, c, Yi Hang Shib, c, Ji Min Qiaoa, d, Ying Qian Zhoua, Huan Wanga, Wen Xin Fanga
aDepartment of Emergency, Nanjing First Hospital, Nanjing Medical University, Nanjing, China
bDepartment of Cardiology, Nanjing First Hospital, Nanjing Medical University, Nanjing, China
cMei Zhang and Yi Hang Shi were co-first authors who contributed equally to this work.
dCorresponding Author: Ji Min Qiao, Department of Emergency, Nanjing First Hospital, Nanjing Medical University, Nanjing, China
Manuscript submitted April 21, 2025, accepted June 5, 2025, published online June 16, 2025
Short title: Hyperperfusion and ABG Success in Acute HF
doi: https://doi.org/10.14740/cr2076
| Abstract | ▴Top |
Background: This study aimed to explore the effect of radial artery flow hyperperfusion on the successful collection of radial artery blood gas specimens in patients with acute heart failure.
Methods: From February 2023 to December 2024, 548 patients with acute heart failure in the database of the emergency rescue room of our hospital were divided into two groups: non-hyperperfusion group and hyperperfusion group. In the hyperperfusion group, arterial blood gas was collected using the radial artery hyperinfusion method (improving radial artery perfusion by blocking arteries other than the radial artery in the forearm using a customized sphygmomanometer with a double-airbag hollow cuff). The primary endpoint was the success rate of one-time puncture and the success rate of total puncture. Secondary endpoints included puncture frequency of > 3 times, puncture time, pain, puncture site hematoma, puncture site bruise, and patients’ satisfaction.
Results: In total, 548 patients were included, including 325 in the non-hyperperfusion group and 223 in the hyperperfusion group. The hyperperfusion group exhibited a significantly higher success rate of one-time puncture (63.4% vs. 83.4%, P< 0.001) and success rate of total puncture (82.5% vs. 94.6%, P < 0.001) compared to the non-hyperperfusion group. Additionally, the hyperperfusion group experienced a significantly reduced number of patients with puncture frequency > 3 times (26.2% vs. 9.9%, P < 0.001) and puncture time (48.59 ± 7.83 s vs. 26.43 ± 6.44 s, P < 0.001). This approach also effectively decreased the risk of puncture site hematoma (2.2% vs. 0.0%, P = 0.045), arm puncture place bruise (5.5% vs. 0.4%, P<0.001), and pain (3.0 (3.0, 4.0) vs. 2.0 (1.0, 2.0), P <0.001) and improved patients’ satisfaction after adopting the radial artery hyperinfusion method.
Conclusions: Radial artery hyperperfusion improved the success rate of puncture for radial artery blood specimen collection in patients with acute heart failure, reduced puncture complications, and improved patients’ satisfaction.
Keywords: Radial artery; Hyperperfusion; Blood gas specimen collection; Sphygmometer; Puncture success rate
| Introduction | ▴Top |
Patients with acute heart failure and acute and critical conditions need to undergo rapid bedside arterial blood gas analysis to detect arterial blood pH, lactate, PaO2, PaCO2, potassium, and other indicators. These indicators can help estimate the patient’s respiratory function and metabolic status, guide oxygen therapy, and correct acid-base imbalance and electrolyte disorders [1]. It is preferred to collect arterial blood gas from the radial artery because of its superficial position, ease of palpation, and absence of major nerves [2, 3]. However, patients with acute heart failure have a reduced cardiac output and stroke volume, which makes puncture based on the touch-blind puncture method more difficult [4, 5].
A study [6] reported that the success rates of one-time puncture and total puncture were only 60% and 80.8% among critically ill patients, respectively. The success rate of puncture is even lower in stressful situations, where the diameter of the radial artery is relatively lower [7, 8]. Repeated puncture of the radial artery can lead to arterial spasm and injury, leading to failure of radial artery puncture, puncture site hematoma, and vasovagal reflexes, increasing patients’ pain and nurse workload and decreasing patients’ satisfaction. Although ultrasound-guided blood gas analysis of the radial artery for blood sample collection can improve the success rate of one-time radial artery puncture and decrease patients’ pain and complications [9], the technology has not been popularized in clinical settings due to the high price of ultrasound machines and lack of ultrasound qualifications among nurses in China.
Previous studies [10] have shown that selective blockade of the ulnar artery by a double airbag hollow cuff can improve radial artery perfusion, enhance radial artery pulsation, and thicken the diameter. This study aimed to explore the effect of hyperperfusion on the success rate of radial artery blood specimen collection in patients with acute heart failure, thereby reducing puncture complications and improving patients’ satisfaction.
| Materials and Methods | ▴Top |
Participants
In total, 548 patients with acute heart failure in the database of our emergency department from February 2023 to December 2024 were selected for this study. Patients undergoing blood gas collection from February 2023 to December 2023 were assigned to the non-hyperperfusion group (325 patients), and patients undergoing blood gas collection from January 2024 to December 2024 were assigned to the hyperperfusion group (223 patients). The study protocol was approved by the hospital ethics committee. All 548 patients provided informed consent. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
The inclusion criteria were as follows: 1) age more than 14 years; 2) experiencing acute heart failure episodes; 3) meeting the criteria for pre-screening triage level I-II [11]; 4) first radial artery blood specimen collection; 5) peak systolic flow velocity in radial artery < 35 cm/s; 6) radial artery puncture using a 22G BD Preset™ 3 mL arterial blood sampler; and 7) being conscious and co-operative.
The exclusion criteria were as follows: 1) absence or occlusion of the radial artery; 2) radial artery with hematoma and bruising before puncture; 3) forearm trauma; 4) arteriovenous fistula; and 5) coagulation abnormalities.
Withdrawal criteria were as follows: 1) incidence of vasovagal reflexes; and 2) death.
Non-hyperperfusion group
For the non-hyperperfusion group, the nurse used the traditional radial artery touch-blind puncture method to collect radial artery blood specimens. 1) The middle finger and index finger of the left hand fixed the radial artery pulsation at the strongest position of (approximately one finger from the transverse carpal stripe and approximately 0.5 - 1 cm from the lateral forearm) blood vessels. 2) The right hand held the BD artery blood collector in a pen position from the positioning of the index finger 0.5 - 1 cm, the needle beveled upward, and the skin was 30-45° reverse-punctured. 3) The radial artery blood returned after fixing the blood collector, and the nurse waited until blood filled automatically. Then, the nurse pulled out the needle, and pressed the puncture site to fully stop bleeding. Close attention was paid to the patient’s vital signs during radial artery blood specimen collection, and the patient was monitored for vasovagal reflex.
Hyperperfusion group
In the hyperperfusion group, the nurse conducted radial artery blood collection from the patient using a custom sphygmomanometer with the freedom to set cuff pressure and compression time and cycle (Fig. 1a) to increase radial artery flow. Before radial artery blood gas collection, 1) the Bestman BV-520T+ ultrasonic Doppler flow detector was employed to detect the radial artery flow echo, precisely localize, and mark the radial artery course in the forearm. 2) The 2 × 12 cm airless section in the middle of the custom-made 80° angular dual-bladed hollow cuff (Fig. 1b) was placed above the radial artery marking place (close to the elbow) to tie up the forearm in a circle (loosened or tightened so that one finger can be inserted). 3) Connecting a customized sphygmomanometer to a PDA via Bluetooth. 4) The sphygmomanometer was pre-set using the app on the PDA side (Fig. 1c). The cuff inflation pressure was 30 mm Hg higher than the patient’s systolic blood pressure, the cuff inflation and compression time was 5 min, and the compression cycle was set to 1 [10, 12]. 5) After clicking one button to start, the sphygmomanometer automatically inflated and pressurized the cuff pressure to 30 mm Hg higher than the patient’s systolic pressure for 5 min, and then the cuff pressure was automatically reduced to 0 mm Hg after 5 min. During the period of high-pressure compression of the forearm with dual airbags, the sensors automatically sensed when the cuff pressure was lower than the pre-set pressure value of 1 mm Hg and automatically increased the pressure to the pre-set pressure value to maintain the stability of the cuff pressure during high-pressure compression. During high-pressure compression of the dual airbag hollow cuff at an angle of 80°, the blood flow of the radial recurrent artery, ulnar recurrent artery, common interosseous artery, and ulnar artery of the forearm was blocked. After the inflation and pressurization of the dual airbag cuff, the hollow airbag-free section was in a suspended state, and the radial artery directly under the airbag-free section showed increased perfusion and thickened vascular diameter. Then, radial artery blood gas specimen collection was conducted when the hollow cuff maintained a hyperperfusion of radial artery blood flow for 20 to 30 s. Specific radial artery blood gas collection methods and precautions were the same as those in the non-hyperperfusion group.
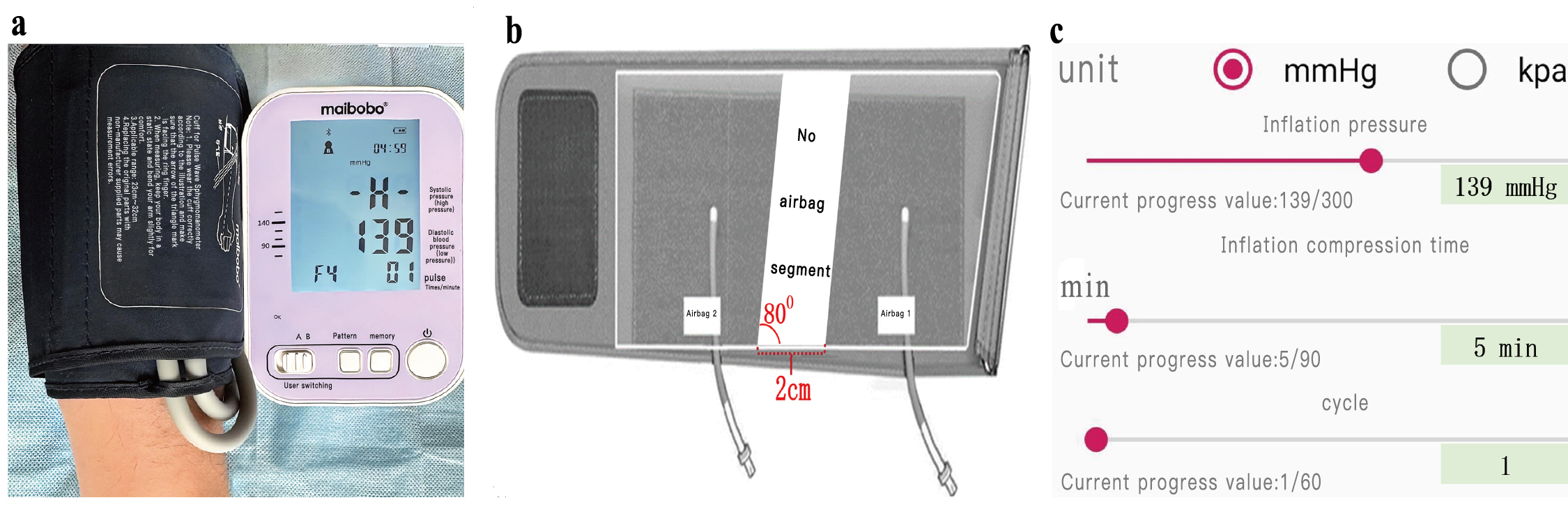 Click for large image | Figure 1. Related equipment and operating procedures. (a) Custom sphygmomanometer. (b) Custom dual airbag hollow cuff. (c) Pre-set use of the app. |
Endpoints, definitions, and quality control
Endpoints
The primary endpoint was the success rate of one-time puncture and the success rate of total puncture. Secondary endpoints included puncture frequency of > 3 times, puncture time, pain, puncture site hematoma, puncture site bruise, and patients’ satisfaction.
Definitions
The definitions were as follows. The success rate of one-time puncture: radial artery blood collection success rate after the first puncture. Success rate of total puncture: radial artery blood collection success rate after the final puncture. Puncture frequency > 3 times: frequency of needle insertion for successful collection of radial artery blood specimen > 3 times. Puncture time: total time taken from the start of puncture site sterilization to the successful collection of the radial artery blood specimen. Pain: pain during radial artery puncture was assessed using a numerical rating scale of 0 to 10, with no pain receiving 0 scores and severe pain receiving 7 to 10 scores [13]. The patient’s highest pain score was recorded. Hematoma and bruising. Patients’ satisfaction: the department’s own percentage-based satisfaction questionnaire was used to assess satisfaction with radial artery blood gas specimen collection in patients with acute heart failure. The questionnaire was developed with reference to existing clinical arterial puncture satisfaction questionnaires and incorporated the clinical experience and research needs of our department [14]. The questionnaire included four dimensions of first aid quality, nursing quality, puncture technique, and service attitude, with a scale Cronbach’s α coefficient of 0.916. When using the questionnaire, 90 - 100 points indicated very satisfied, 80 - 89 points indicated satisfied, 60 - 79 points indicated basically satisfied, and < 60 points indicated dissatisfied.
Quality control
A blood gas collection research team was set up, with the project leader as the team leader, six provincial specialist nurses as the deputy team leaders, and 10 charge nurses as team members. The team leader was responsible for operational training and guided the use of the customized sphygmomanometer, dual-bag hollow cuff, Bestman BV-520T+ ultrasonic Doppler flow detector, and radial artery blood gas collection. The team members were proficient in training. The deputy team leader was responsible for quality control, and the team members were responsible for enrolling patients. A deputy team leader and a team member were present for patient assessment, blood gas collection, and data collection to ensure the scientific rigor of the study.
Statistical analysis
All statistical analyses were conducted using SPSS 25.0 (IBM Corp, Armonk, NY, USA). Count data are described as frequencies and percentages and were compared using the χ2 test and Fisher’s exact probability method. Quantitative data with normal distribution are presented as mean ± standard deviation and were analyzed using the independent samples t-test. Data without a normal distribution are expressed as median and quartiles and were analyzed using the Mann-Whitney U test. Differences were considered statistically significant at P < 0.05.
| Results | ▴Top |
Baseline characteristics
In total, 548 patients were included in this study. There were no significant differences between the two groups in terms of age (70.83 ± 10.54 vs. 71.25 ± 10.61, P = 0.648), male gender (61.2% vs. 67.3%, P = 0.149), and platelet count (201.28 ± 32.52 vs. 197.87 ± 31.63, P = 0.223) (Table 1). Additionally, there were no significant differences between the two groups in terms of the prevalence of atrial fibrillation (18.8% vs. 15.7%, P = 0.352), hypertension (72.0% vs. 65.0%, P = 0.082), and diabetes (21.5% vs. 16.6%, P = 0.151).
 Click to view | Table 1. Comparison of General Information Between the Two Groups |
Comparison of puncture frequency > 3 times and puncture time between the two groups
As shown in Table 2 and Figure 2, the non-hyperperfusion group reported higher puncture frequency > 3 times (26.2% vs. 9.9%, P < 0.001) and puncture time (48.59 ± 7.83 s vs. 26.43 ± 6.44 s, P < 0.001).
 Click to view | Table 2. Comparison of Puncture Success Rate, Puncture Frequency > 3 Times, and Puncture Time Between the Two Groups |
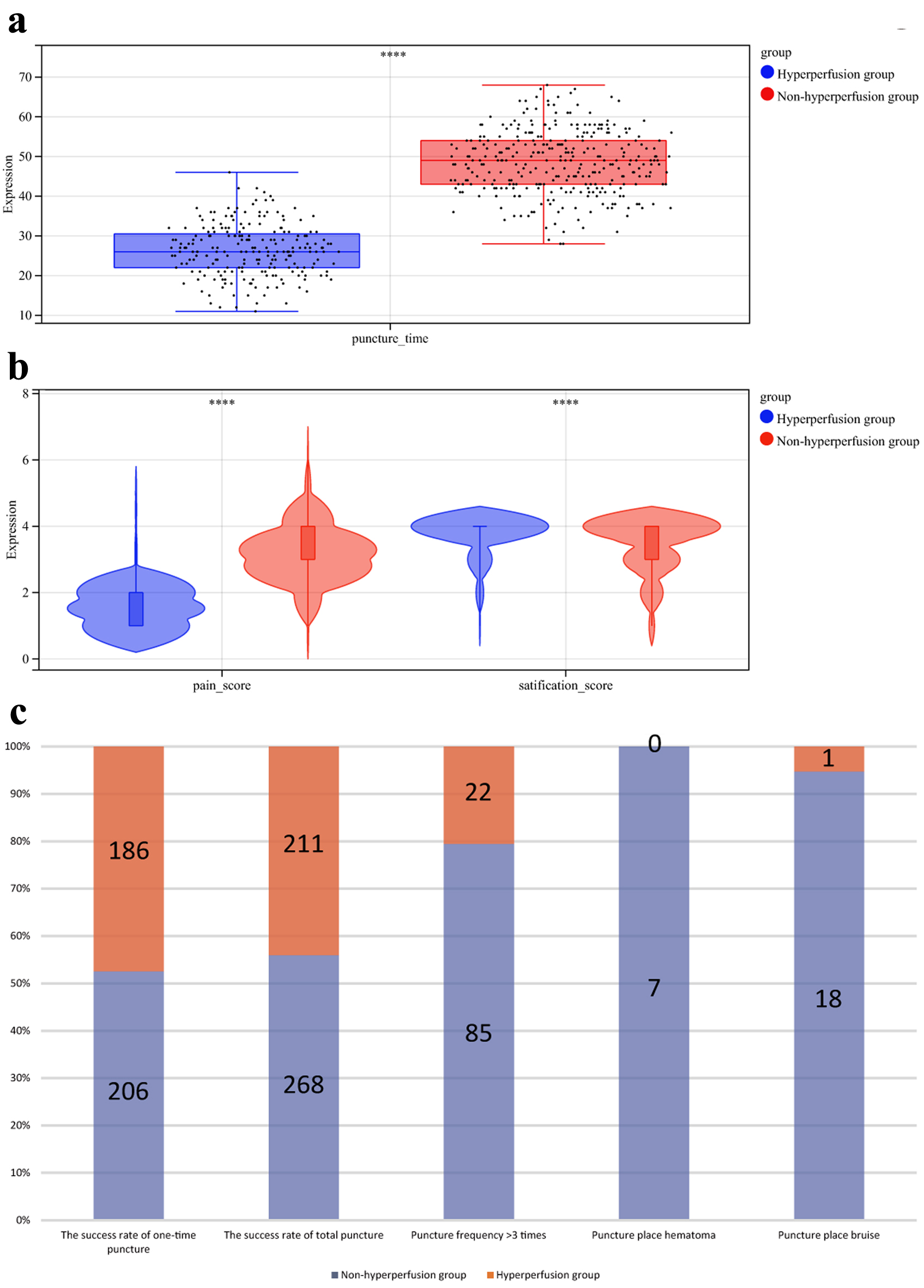 Click for large image | Figure 2. Comparison of puncture times (a), pain scores and satisfaction score (b), and different puncture results (c). |
Comparison of puncture site pain, hematoma, and bruising and patients’ satisfaction between the two groups
As shown in Tables 3, 4 and Figure 2, the hyperperfusion group showed significantly lower pain scores (3.0 (3.0, 4.0) vs. 2.0 (1.0, 2.0), P < 0.001), puncture site hematoma (2.2% vs. 0.0%, P = 0.045), and puncture site bruise (5.5% vs. 0.4%, P < 0.001) (Table 3). Additionally, patients’ satisfaction was significantly improved in the hyperperfusion group (Table 4).
 Click to view | Table 3. Comparison of Puncture Place Pain, Hematoma, and Bruise between the Two Groups |
 Click to view | Table 4. Comparison of Satisfaction Between the Two Groups |
Comparison of primary endpoints, one-time puncture success rate, and total puncture success rate
As shown in Table 2 and Figure 2, the hyperperfusion group exhibited a significantly higher one-time puncture success rate (63.4% vs. 83.4%, P < 0.001) and total puncture success rate (82.5% vs. 94.6%, P < 0.001) compared to the non-hyperperfusion group.
| Discussion | ▴Top |
Implementation of the radial artery hyperperfusion method before radial artery blood gas specimen collection in patients with acute heart failure using a customized sphygmomanometer with a dual-bladder hollow cuff improves the success rate of puncture for blood gas specimen collection, reduces puncture complications, and improves patients’ satisfaction. These findings suggest that radial artery blood gas specimen collection under hyperperfusion is safe and effective.
Hyperperfusion of radial artery blood flow increased the success rate of blood specimen collection and reduced the frequency of puncturing
Arterial blood gas analysis is one of the most common tests conducted in the emergency room, which can objectively reflect the oxygenation status of patients with acute heart failure, the type of expiratory failure, and acid-base balance, guide clinical decisions, and help assess the prognosis of the disease. Radial artery blood specimen collection is an important skill that nurses in the emergency room need to master. However, the success rate of the traditional radial artery touch-blind puncture method mainly depends on the nurse’s puncture experience, the patient’s radial artery pulsation strength, and vascular diameter. Enhancing the radial artery pulsation strength and increasing the radial artery diameter of patients with acute heart failure through nursing interventions have been a hot spot in clinical nursing research.
This study showed that the one-time puncture success rate, total puncture success rate, puncture frequency > 3 times, and puncture time for radial artery blood specimen collection were better in the hyperperfusion group than in the non-hyperperfusion group (P < 0.05). Our results were consistent with the results of previous studies [10, 15]. Some patients with acute heart failure in the non-hyperperfusion group had radial artery pulsations that were not easily palpable and arterial diameters that were thinner due to obesity, edema, atrial fibrillation, and peripheral hypoperfusion, which made radial artery puncture more difficult. Some studies [16, 17] have shown that when the puncture needle damages the radial artery wall, radial artery smooth muscle stress contraction can easily lead to radial artery spasm, vasoconstriction, and obstruction of blood flow. Subsequently, the antegrade blood flow of the brachial artery will be gradually shunted to branch arteries other than the radial artery, thereby weakening the radial artery blood flow and decreasing the diameter of the vessel and the success rate of radial artery puncture. In the hyperperfusion group, after the custom 80° angle (close to the physiological and anatomical direction of the radial artery at the elbow) double-airbag hollow cuff was inflated and pressurized to a constant pressure. The parallelogram without airbag section with a height of 12 cm in the middle × 2 cm at the bottom was suspended (with the radial artery directly below it having a smooth flow of blood), and the anterior blood flow of the radial recurrent artery, the ulnar recurrent artery, the interosseous common artery, and the ulnar artery was completely blocked, and the brachial artery blood flow completely reached the radial artery completely, leading to its hyperperfusion. Hyperperfusion of the radial artery results in increased filling of the radial artery, increased pulsation, and vasodilation. In this study, the radial artery perfusion and vascular diameter reached the maximum value after maintaining hyperperfusion of radial artery blood flow for 20 to 30 s. At this time, the radial artery was more accurately positioned for touching, and the needle of the blood collector more easily entered into the lumen of the radial artery, increasing the one-time success rate of the radial artery blood specimen collection. Even when puncture failure of the radial artery in the hyperperfusion group led to radial artery spasm, the diameter of the radial artery in the hyperperfusion state was still much higher than that in the low perfusion state due to the blockade of all arteries in the forearm other than the radial artery [18]. The increase in blood flow velocity prevented coagulation at the puncture site, increased the overall success rate of blood specimen collection from the radial artery, and reduced the frequency and duration of puncture. Therefore, hyperperfusion of the radial artery blood flow can improve the success rate of blood specimen collection from the radial artery and reduce the frequency and duration of puncture in patients with acute heart failure.
Hyperperfusion of the radial artery reduced the complications of blood specimen collection and improved patients’ satisfaction
This study showed that pain, hematoma, bruising, and patients’ satisfaction at the puncture site of the radial artery were better in the hyperperfusion group than in the non-hyperperfusion group (P < 0.05). Our findings were consistent with the findings of Mufarrih et al [19] and Liu et al [20]. The success rate of one-time puncture for radial artery blood specimen collection was relatively low in the non-hyperinfusion group. Frequent puncture is more likely to cause mechanical damage to the radial artery wall and induce inflammatory reactions in the local tissues, which aggravates the pain. The increase in radial artery blood perfusion in the hyperperfusion group increased the oxygen supply to local tissues at the radial artery puncture site and took away local inflammatory mediators at the radial artery puncture site. Besides, the increase in the elasticity of the vascular wall of the radial artery can effectively minimize the mechanical damage of the vascular wall due to puncture, thereby maintaining the integrity of the radial artery endothelium and ameliorating patients’ pain.
Some studies [21] have shown that damage to the vascular wall of the radial artery can cause intimal tearing, and aggravate local bleeding at the puncture site, hematoma, and bruise. Increased perfusion of the radial artery in the hyperperfusion group during radial artery puncture minimized mechanical damage to the vascular wall and decreased local bleeding and exudation. In addition, hyperperfusion of the radial artery increased local blood flow velocity, reduced the local pooling of blood in the radial artery puncture site, and decreased the incidence of hematoma and bruising at the puncture site. Improved radial artery one-time puncture success rate and total puncture success rate and reduced puncture frequency, puncture time, puncture complications, pain, anxiety, and discomfort during radial artery puncture can improve patients’ experience of medical treatment, thereby improving patients’ satisfaction [22]. Therefore, radial artery hyperperfusion can reduce the complications of radial artery blood specimen collection in patients with acute heart failure and improve patients’ satisfaction.
Limitations
The inclusion and exclusion criteria were strictly followed in this study to ensure homogeneity of the study population and minimize the effect of enrolment bias on the results. However, it is important to acknowledge the limitations of this study, particularly the relatively modest sample size obtained from a single medical center.
Conclusions
In summary, we used a customized sphygmomanometer combined with an 80° angle dual-bladed hollow cuff to compress the forearm at a constant pressure of 30 mm Hg above the patient’s systolic blood pressure, and radial artery blood was collected after 20 - 30 s of radial artery blood flow hyperperfusion during which constant pressure compression was maintained. This method improved the success rate of radial artery blood specimen collection in patients with acute heart failure, reduced the complication of puncture, and improved patients’ satisfaction.
Acknowledgments
We thank the patients and their families and all colleagues who contributed to this study.
Financial Disclosure
National Natural Science Foundation of China Youth Science Fund Grant Program (82200385); Nanjing Health Science and Technology Development Fund Program (YKK23121); Nanjing First Hospital Spark Cultivation Nursing Development Fund; National Utility Model Patent (ZL201921841348.8).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Informed Consent
The participants gave written informed consent for their personal or clinical details along with any identifying images to be published in this study.
Author Contributions
Mei Zhang designed and refined the entire study. Mei Zhang and Yi Hang Shi entered, integrated, analyzed, and wrote the entire article. Ji Min Qiao was responsible for the clinical study. Ying Qian Zhou, Huan Wang, and Wen Xin Fang collected data in the clinic. All authors have read and suggested revisions to the article, agreeing to the final text.
Data Availability
The data that support the findings of this study are available on request from the corresponding author.
| References | ▴Top |
- Castro D, Patil SM, Zubair M, Keenaghan M. Arterial blood gas. In: StatPearls. Treasure Island (FL) ineligible companies. 2025.
pubmed - Brzezinski M, Luisetti T, London MJ. Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Anesth Analg. 2009;109(6):1763-1781.
doi pubmed - Lakhal K, Robert-Edan V. Invasive monitoring of blood pressure: a radiant future for brachial artery as an alternative to radial artery catheterisation? J Thorac Dis. 2017;9(12):4812-4816.
doi pubmed - Aljohar A, Alhabib K, AlFaleh H, Hersi A, Habeeb WA, Ullah A, Elasfar A, et al. The prognostic impact of pulse pressure in acute heart failure: insights from the HEARTS registry. J Saudi Heart Assoc. 2020;32(2):263-273.
doi pubmed - Mazimba S, Mwansa H, Breathett K, Strickling JE, Shah K, McNamara C, Mehta N, et al. Systemic arterial pulsatility index (SAPi) predicts adverse outcomes in advanced heart failure patients. Heart Vessels. 2022;37(10):1719-1727.
doi pubmed - Wu XL, Wang JJ, Yuan DQ, Chen WT. Ultrasound-guided radial artery catheterization at different sites: a prospective and randomized study. Eur Rev Med Pharmacol Sci. 2022;26(2):415-421.
doi pubmed - Moussa Pacha H, Alahdab F, Al-Khadra Y, Idris A, Rabbat F, Darmoch F, Soud M, et al. Ultrasound-guided versus palpation-guided radial artery catheterization in adult population: A systematic review and meta-analysis of randomized controlled trials. Am Heart J. 2018;204:1-8.
doi pubmed - Wu WJ, Goldberg LH, Rubenzik MK, Zelickson BR. Review of the Evaluation and Treatment of Vasovagal Reactions in Outpatient Procedures. Dermatol Surg. 2018;44(12):1483-1488.
doi pubmed - Bhattacharjee S, Maitra S, Baidya DK. Comparison between ultrasound guided technique and digital palpation technique for radial artery cannulation in adult patients: An updated meta-analysis of randomized controlled trials. J Clin Anesth. 2018;47:54-59.
doi pubmed - Zhou X, Qiao J, Li K, et al. Selective ulnar artery continuous circulatory compression to reduce radial artery occlusion in elderly patients undergoing coronary intervention. Journal of Practical Clinical Medicine. 2024;28(3):122-125.130. [in Chinese].
doi - Rao SV, O'Donoghue ML, Ruel M, Rab T, Tamis-Holland JE, Alexander JH, Baber U, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025;151(13):e771-e862.
doi pubmed - Qiao J, Shi Y, Li K, Zhu X, Wang Z. Application of multifunctional pulse wave sphygmomanometer combined with constant temperature ice in patients with forearm hematoma after coronary intervention. BMC Cardiovasc Disord. 2025;25(1):8.
doi pubmed - Duncan JAL, Bond JS, Mason T, Ludlow A, Cridland P, O'Kane S, Ferguson MWJ. Visual analogue scale scoring and ranking: a suitable and sensitive method for assessing scar quality? Plast Reconstr Surg. 2006;118(4):909-918.
doi pubmed - Shi L, Ju Y, Rui N, Cao Y, Shan T, Chen L. The efficacy of ultrasonography on learning curve and inter-subject performance variability in radial artery cannulation in standardized training for residents: a randomized controlled trial. Med Ultrason. 2023;25(2):139-144.
doi pubmed - Coomes EA, Haghbayan H, Cheema AN. Distal transradial access for cardiac catheterization: A systematic scoping review. Catheter Cardiovasc Interv. 2020;96(7):1381-1389.
doi pubmed - Duarte PVF, Cortes LA, de Almeida Sampaio FB, Barroso JM, da Silveira GM, Nascif GB, Filho AO, et al. Feasibility and safety of ipsilateral ulnar access in cases of impossibility or failure of radial access for coronary angiography or percutaneous coronary intervention. J Invasive Cardiol. 2022;34(2):E92-E97.
doi pubmed - Jia DA, Zhou YJ, Shi DM, Liu YY, Wang JL, Liu XL, Wang ZJ, et al. Incidence and predictors of radial artery spasm during transradial coronary angiography and intervention. Chin Med J (Engl). 2010;123(7):843-847.
pubmed - Liang Y, Liu P, Wei C, Li W, Li C, Lai T, Peng S, et al. Ultrasound-guided modified dynamic needle tip positioning technique for distal radial artery catheterization: A randomized controlled trial. J Vasc Access. 2024:11297298241270537.
doi pubmed - Mufarrih SH, Haider S, Qureshi NQ, Khan MS, Kazimuddin M, Akbar MS, Saleem S, et al. Distal versus proximal radial arterial access for percutaneous coronary angiography and intervention: updated meta-analysis of randomized controlled trials. Am J Cardiol. 2024;218:34-42.
doi pubmed - Liu LJ, Zhou HM, Tang HL, Zhou QH. Evaluation of radial and ulnar artery blood flow after radial artery decannulation using colour Doppler ultrasound. BMC Anesthesiol. 2021;21(1):312.
doi pubmed - Alterman CD, Perera AD, Gupta PK, Alterman DM. Feasibility and safety of endovascular interventions via percutaneous access to the axillary artery. Ann Vasc Surg. 2025;111:194-202.
doi pubmed - Zus AS, Crisan S, Luca S, Nisulescu D, Valcovici M, Patru O, Lazar MA, et al. Radial artery spasm-a review on incidence, prevention and treatment. Diagnostics (Basel). 2024;14(17):1897.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.