| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 16, Number 5, October 2025, pages 403-412
BEAT-HTN India: Burden, Epidemiology, and Trends of Hypertension - A Nationwide Survey
H.K. Chopraa, gg, Navin C. Nandab, A.K. Dasc, Ashok Kripalanid, Uday Jadhave, G.S. Wanderf, Mangesh Tiwaskarg, Umapati Hegdeh, Niteen Deshpandei, Suhas Hardasj, Ajit Mullasarik, Ajit Bhagwatl, Soumitra Raym, Vikas Singhn, S. Chandrasekharo, Rajasekar Chakravarthip, Dharmesh Solankiq, Sarita Bajajr, Tiny Nairs, C.K. Pondet, Dinesh Khullaru, Viveka Kumarv, Satyendra Tiwariw, Vidyut Jainx, A.K. Pancholiay, J.P.S. Sawhneyz, Rajeev Agarwalaaa, Aparna Jaswalbb, Aditya Kapoorw, Roopali Khannaw, A.K. Bhallacc, Sarita Raodd, Shibba Takkar Chhabraf, Kavita Tyagiz, Namrata Gauree, Anu Groverff, gg
aDepartment of Cardiology, Medanta Moolchand Heart Institute, New Delhi, India
bDivision of Cardiology, University of Alabama at Birmingham, Birmingham, AL, USA
cDepartment of Medicine, Shree Hospital and Maternity Center, Muzaffarpur, India
dProfessor Emeritus, Department of Nephrology, Bombay Hospital & Medical Research Center, Mumbai, India
eDepartment of Cardiology, MGM Hospital, Vashi, India
fDepartment of Cardiology, Dayanand Medical College and Hospital, Ludhiana, India
gShilpa Medical Research Centre, Mumbai, India
hDepartment of Nephrology, MPUH, Nadiad, India
iCardiac Cath Lab, Spandan Hospital, Nagpur, India
jDepartment of Cardiology, Hardas Heart Care, Pune, India
kDepartment of Cardiology, The Madras Medical Mission, Chennai, India
lCardiac Cath Lab, Kamalnayan Bajaj Hospital, Aurangabad, India
mDepartment of Invasive Cardiology, AMRI Hospital, Kolkata, India
nDepartment of Interventional Cardiology, Daksh Heart Care, Patna, India
oDiabetology and General Medicine, Medicine Department, Stanely Medical College, Chennai, India
pDepartment of Nephrology and Transplant Services, Hyderabad, India
qDepartment of Cardiology, Wockhardt Hospital, Rajkot, India
rMLN Medical College, Allahabad, India
sDepartment of Cardiology, PRS Hospital, Trivandrum, Kerala, India
tDepartment of Cardiology, PD Hinduja National Hospital and Medical Research Centre, Mumbai, India
uDepartment of Nephrology and Renal Transplant Medicine, Max Super-speciality Hospital, Delhi, India
vDepartment of Cardiac Sciences, Max Hospital, Delhi, India
wDepartment of Cardiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India
xChoithram Hospital, Indore, India
yDepartment of Clinical and Preventive Cardiology, Arihant Hospital and Research Centre, Indore, India
zDepartment of Cardiology, Sir Gangaram Hospital, Delhi, India
aaJaswant Rai Specialty Hospital, Meerut, India
bbDepartment of Cardiac Pacing and Electrophysiology, Fortis Escorts Heart Institute, Delhi, India
ccDialysis Services, Department of Nephrology, Sir Gangaram Hospital, Delhi, India
ddCath Lab, Apollo Hospital, Indore, India
eeDepartment of Cardio Thoracic and Vascular Surgery, AIIMS Rishikesh, Rishikesh, Uttarakhand, India
ffDepartment of Scientific Communications, Mangrove Creations, New Delhi, India
ggCorresponding Authors: Anu Grover, Scientific Communications, Mangrove Creations, New Delhi, India; H.K. Chopra, Department of Cardiology, Medanta Moolchand Heart Institute, New Delhi, India
Manuscript submitted July 10, 2025, accepted August 23, 2025, published online October 10, 2025
Short title: BEAT-HTN India
doi: https://doi.org/10.14740/cr2110
| Abstract | ▴Top |
Background: Hypertension is a growing public health concern in India, increasingly interlinked with metabolic disorders such as diabetes and characterized by significant regional and demographic variation. Despite advancements in diagnosis and treatment, control rates remain unsatisfactory. Elevated resting heart rate (HR), an emerging marker of sympathetic overactivity, may offer additional insight into the underlying pathophysiology of Indian hypertensives. The objective of the study was to assess the prevalence of hypertension across India, explore its association with diabetes, elevated HR, and regional variation, and evaluate the potential role of sympathetic overdrive as a common pathophysiological thread.
Methods: A nationwide, cross-sectional survey was conducted among 41,370 adults across 31 Indian regions. Data on systolic and diastolic blood pressure, resting HR, diabetes history, age, gender, and region were collected and analyzed to identify patterns of comorbidity and demographic distribution.
Results: Overall hypertension prevalence was 29.8% (95% confidence interval (CI): 29.4 - 30.2), higher among males, 33.2% (95% CI: 32.6 - 33.8) than females, 27.2% (95% CI: 26.6 - 27.8). A notable proportion (14.6%, 95% CI: 14.2 - 15.0) of hypertensives also had diabetes, with this comorbidity more prevalent in males (15.8%, 95% CI: 15.2 - 16.4) than females (13.3%, 95% CI: 12.8 - 13.8). The mean resting HR was 83.9 bpm across all participants, exceeding 80 bpm even among normotensives, and was highest in diabetic hypertensives (85.9 vs. 82.2 bpm in non-diabetics; P < 0.05). Hypertension was more common in older adults, males, and those residing in urbanized or rapidly transitioning regions. Though obesity data were not captured, the strong associations between hypertension, diabetes, and elevated HR point toward underlying metabolic dysfunction and sympathetic overactivity.
Conclusion: This large-scale survey reinforces the complex cardiometabolic burden in India and highlights elevated resting HR as a potential surrogate marker of sympathetic overactivity in hypertensives, especially those with diabetes. Regional and demographic disparities underscore the need for integrated, population-specific approaches that go beyond blood pressure control to address the broader spectrum of metabolic and autonomic dysfunction.
Keywords: Hypertension; Diabetes; Resting heart rate; Sympathetic overactivity; India; Epidemiology; Comorbidity; Regional variation
| Introduction | ▴Top |
Non-communicable diseases (NCDs), especially cardiovascular diseases (CVDs), continue to be the leading cause of premature mortality worldwide [1]. In India, hypertension remains a key and rapidly growing contributor to this burden, affecting nearly one in every four adults. Alarmingly, despite various awareness campaigns and treatment availability, only about 10% of individuals with hypertension achieve optimal blood pressure (BP) control [2]. The ICMR-INDIAB national cross-sectional study estimated the weighted prevalence of hypertension at 35.5%, reflecting the extensive reach of this condition across the country [3]. Hypertension is a well-established modifiable risk factor for CVDs, including ischemic heart disease, stroke, heart failure (HF), and chronic kidney disease (CKD) [4]. In India, CVDs account for nearly 28.1% of all deaths, with high systolic BP (SBP) alone contributing to 8.5% of disability-adjusted life years (DALYs) [5]. Furthermore, hypertension is responsible for 57% of stroke-related deaths and 24% of coronary heart disease (CHD) mortality [6].
Traditionally viewed in isolation, hypertension is now increasingly recognized as part of a broader metabolic continuum, often coexisting with obesity, insulin resistance, and dyslipidemia, collectively constituting metabolic syndrome. A growing body of literature documents the interrelationship between obesity, diabetes, and CVDs, emphasizing visceral adiposity’s significant role in driving systemic inflammation, sympathetic overactivity, and endothelial dysfunction, key precursors to hypertension and atherosclerosis [7-10]. The rising prevalence of obesity in India, especially among urban youth and middle-aged adults, further exacerbates the hypertension burden. A hospital-based study by Chopra et al 2007 found abdominal waist circumference (> 90 cm in males and > 80 cm in females) as the most reliable predictor of metabolic risk, highlighting its significance in early identification of high-risk individuals [11]. Moreover, 3D echocardiographic assessments have shown that metabolic syndrome frequently coexists with subclinical CVD. The left ventricular myocardial performance index (LVMPI) has emerged as a sensitive early marker of diastolic dysfunction [12]. Similarly, left ventricular hypertrophy (LVH), particularly concentric hypertrophy, increases progressively with declining renal function, highlighting the need for early CV risk assessment in patients with CKD [13].
With hypertension and metabolic syndrome on the rise, diastolic heart failure (DHF), which now accounts for over half of all HF cases, has become a major clinical challenge. Early-stage dysfunction is often subclinical and may go undetected without advanced imaging modalities [14]. Although body mass index (BMI) or waist circumference was not directly measured in this survey, the role of obesity cannot be overlooked in any epidemiological study on hypertension. Recent data from NFHS-5 and other national registries indicate a significant rise in overweight and obesity rates across all socioeconomic strata, further linking hypertension with the broader obesity-diabetes-CVD triad [15]. This interconnected cluster of lifestyle-related conditions represents a modern-day syndemic that requires an integrated public health response.
India is undergoing a rapid epidemiological transition, with urbanization and lifestyle changes contributing significantly to the rising prevalence and regional disparities in hypertension. To address these challenges, a comprehensive pan-India evaluation of hypertension is imperative, not just to assess prevalence, but also to understand its demographic trends, regional variations, and association with key comorbidities like diabetes and elevated heart rate (HR). Such efforts are aligned with the 2024 World Hypertension Day theme, “Measure Your Blood Pressure Accurately, Control It, Live Longer,” and are vital to formulate national strategies and health policies [16]. The BEAT-HTN India Survey (Burden, Epidemiology, and Trends of Hypertension) was thus conceptualized to fill critical data gaps and provide evidence-based insights into the evolving burden of hypertension and its metabolic determinants in Indian population.
| Materials and Methods | ▴Top |
Study design and setting
This BEAT-HTN India Survey was designed as a nationwide, cross-sectional community-based screening initiative conducted under the “BP Right Karo” campaign. The survey spanned 1 year, from October 2023 and October 2024, and covered a representative mix of urban, semi-urban, and rural populations across various regions of India. The objective was to estimate the burden, demographic distribution, and associated trends of hypertension in Indian adults.
Ethical considerations
The study followed ethical standards for research involving human participants and complied with the Declaration of Helsinki. Verbal informed consent was obtained prior to data collection. As the survey involved anonymous community-level screening without clinical intervention or sensitive data collection, prior ethics approval was not required for data collection. However, ethics approval for publication was obtained from the Kusum Independent Ethics Committee (approval no. ECR/1802/Inst/MH/2023), in accordance with ICH-GCP, ICMR guidelines, and the New Drugs and Clinical Trials Rules, 2019.
Participants
Participants were recruited through community-based screening camps and outpatient clinics. Eligible participants included adults aged ≥ 18 years, recruited from 28 Indian states and three Union Territories, representing a total of 31 regions. Participation was voluntary, and verbal informed consent was obtained from each participant. A total of 41,370 individuals were included in the final analysis. Trained personnel collected demographic data (age, sex, and geographic region), self-reported history of hypertension and/or diabetes, and use of antihypertensive medication.
BP measurement protocol
Standardized procedures and validated devices were used uniformly across all sites, to minimize inter-observer variability. Participants were seated in a calm setting, with a rest period of at least 10 min before the first reading. Two measurements were taken, 1 min apart. An average of the two readings was considered final and rounded to the nearest whole number. Participants were advised to avoid caffeine or tea at least 10 min prior to measurement. HR was also recorded using the same device.
Definition and classification of hypertension
The Indian Guidelines on Hypertension (IGH) 2019 were used to define and classify BP levels in adults (Table 1) [17]. This guideline was chosen to ensure relevance and contextual accuracy, as it incorporates regional characteristics such as earlier age of onset, urban-rural variation, and BP variability with seasonal and environmental factors [18].
 Click to view | Table 1. Blood Pressure Classification According to the 2019 Indian Guidelines on Hypertension |
Anthropometric considerations
While anthropometric measures (weight, height, waist circumference) were not recorded as the primary focus of this survey was blood pressure, HR, and comorbid diabetes, the role of obesity as a parallel epidemic exacerbating hypertension is acknowledged. To address this gap, existing Indian evidence linking central obesity, metabolic syndrome, and cardiovascular risk has been incorporated to interpret our findings within a broader cardiometabolic context.
Statistical analysis
Descriptive statistical analyses were applied to summarize participant characteristics. Categorical variables were expressed as proportions with 95% confidence intervals (CIs), and continuous variables as means with standard deviations and 95% CIs where appropriate. The distribution of BP categories, (normal, high-normal, stage 1, stage 2, and stage 3 hypertension) was analyzed across age groups (18- 30, 31 - 50, 51 - 65, and > 65 years), gender and regions. Associations between hypertension and variables such as age, gender, region, and comorbid diabetes were examined using the Chi-square test. To further account for confounding, multivariable logistic regression was performed adjusting for age, sex, and region, with results reported as odds ratios (ORs) and 95% CIs. All data were compiled and analyzed using Microsoft Excel. A P-value of < 0.05 was considered statistically significant.
| Results | ▴Top |
A total of 41,370 adult participants were enrolled across 31 regions (28 states and three Union Territories), with a male predominance (62.8%). The mean age of the cohort was 53.4 ± 11.9 years. The average systolic and diastolic BP were 145.7 ± 18.5 and 89.4 ± 11.0 mm Hg respectively, with a mean HR of 83.9 ± 10.9 bpm. Table 2 summarizes the baseline demographic and clinical characteristics of the participants.
 Click to view | Table 2. Baseline Characteristics of Study Population |
Regional prevalence of hypertension
The burden of hypertension varied significantly across India’s four major geographical regions (Table 3, Fig. 1). The northern (80.2%) and western (79.6%) regions exhibited the highest hypertension prevalence, while the eastern region had the lowest (70.4%).
 Click to view | Table 3. Regional Distribution of BP Categories |
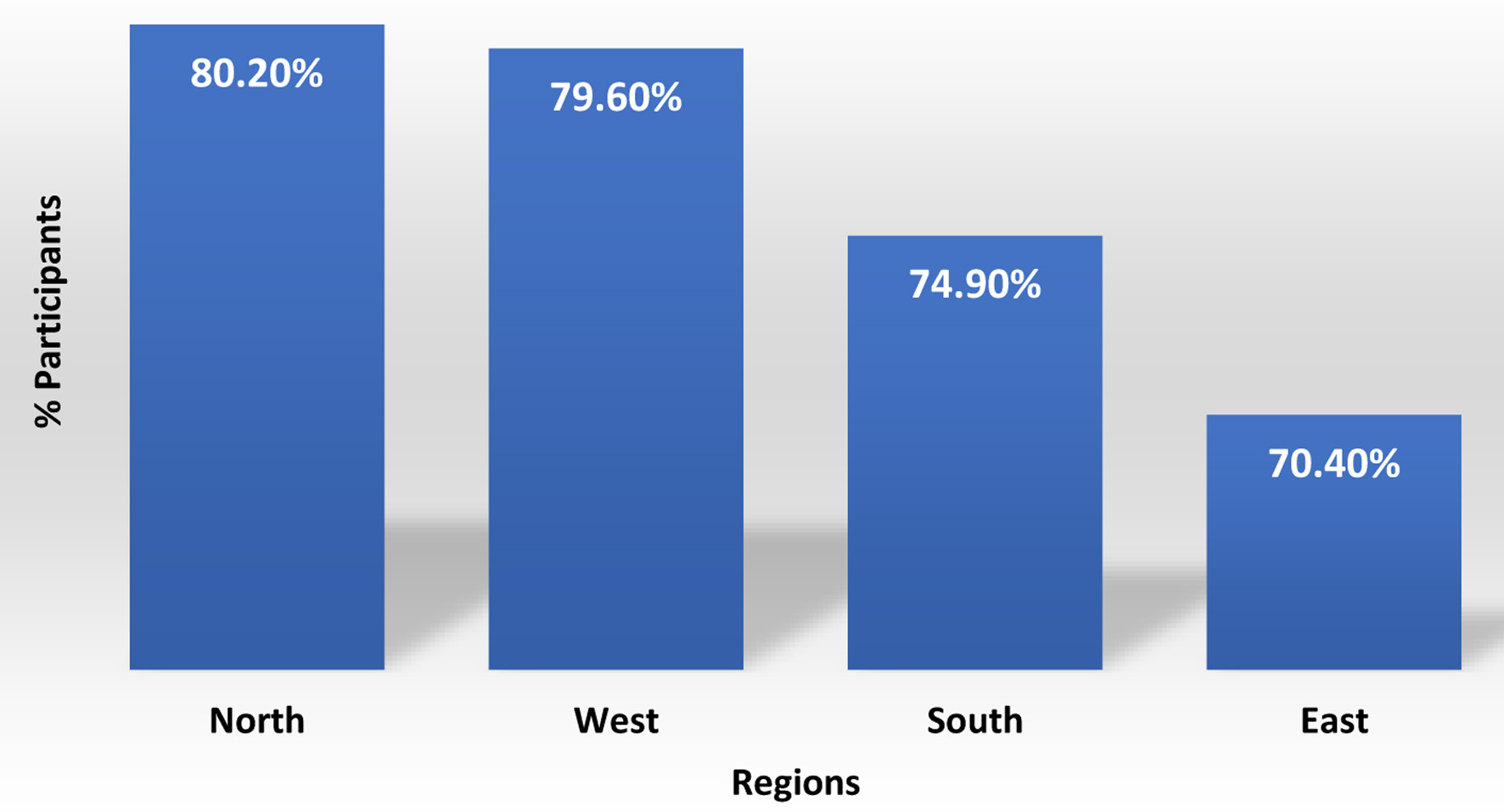 Click for large image | Figure 1. Region-wise prevalence of hypertension. |
Interestingly, the proportion of individuals with prehypertension was relatively consistent across all regions (ranging from 12.7% to 15.3%), highlighting the pervasive risk of future hypertension if early interventions are not implemented.
State-wise prevalence of hypertension in men and women
A state-level analysis revealed notable gender and regional disparities (Table 4). Men consistently had a higher prevalence of hypertension across most states. The highest male-to-female disparity was observed in Chandigarh (76% vs 23%), while Puducherry was the only region where female prevalence (60%) surpassed male prevalence (40%). Sikkim reported equal prevalence between genders.
 Click to view | Table 4. State-Wise Prevalence of Hypertension in Men and Women |
Himachal Pradesh (69%), Jharkhand (63%), and Haryana (58%) reported the highest male hypertension burden. Among women, Puducherry (60%), Tamil Nadu (33%), and Chhattisgarh (33%) had the highest rates. States with large sample sizes such as Maharashtra, Gujarat, and West Bengal showed substantial hypertension burdens in both genders.
Gender- and age-wise distribution of hypertension
When stratified by stages, stage 1 hypertension was most prevalent across the entire cohort (65.9%), more common in men (66.9%) than women (64.4%). Stage 2 hypertension affected 7.3% of the population (7.7% of men vs. 6.7% of women), while stage 3 hypertension was observed in 1.1% overall, again slightly higher in men (1.2% vs. 1.0%).
Interestingly, a larger proportion of women had normal (13.3%) and high-normal BP (14.6%) than men, suggesting better early BP control or underdiagnosis among women (Fig. 2).
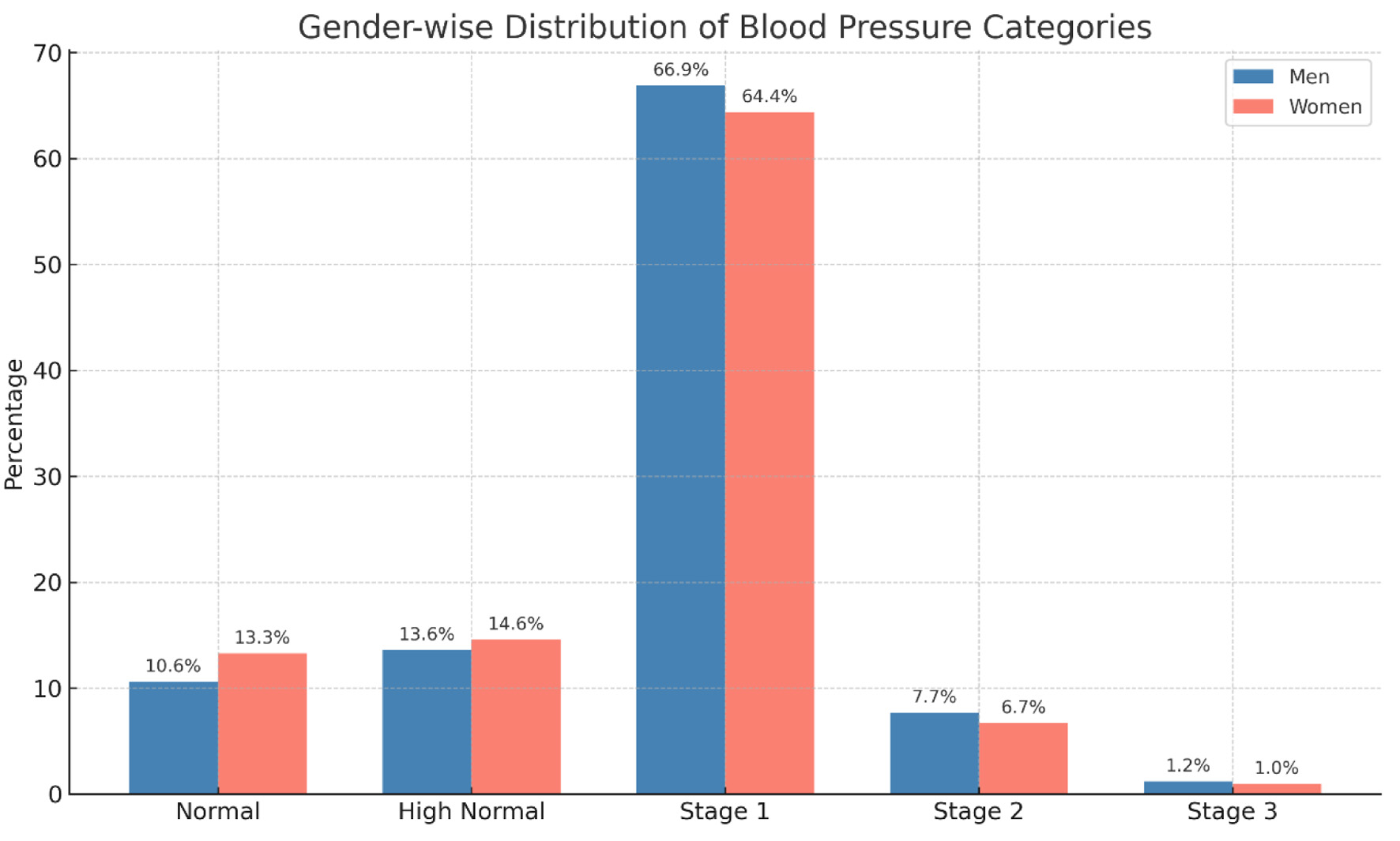 Click for large image | Figure 2. Gender-wise distribution across hypertension stages. |
A clear age-related increase in hypertension prevalence was noted in both genders: 1) Among women, prevalence rose sharply from 21.7% in 18 - 30 years old group to 61.6% in the 31 - 50 years, peaking at 84.3% in those above 65. Concurrently, the proportion of normotensive women declined from 64.1% in the youngest group to 6.2% in the oldest (Fig. 3). 2) A similar trend was observed among men, with prevalence increasing from 30.0% (18 - 30 years) to 65.8% (31 - 50 years), and reaching 87.2% in those above 65. Normotension in men dropped from 50.8% to 4.0% over the same span (Fig. 4).
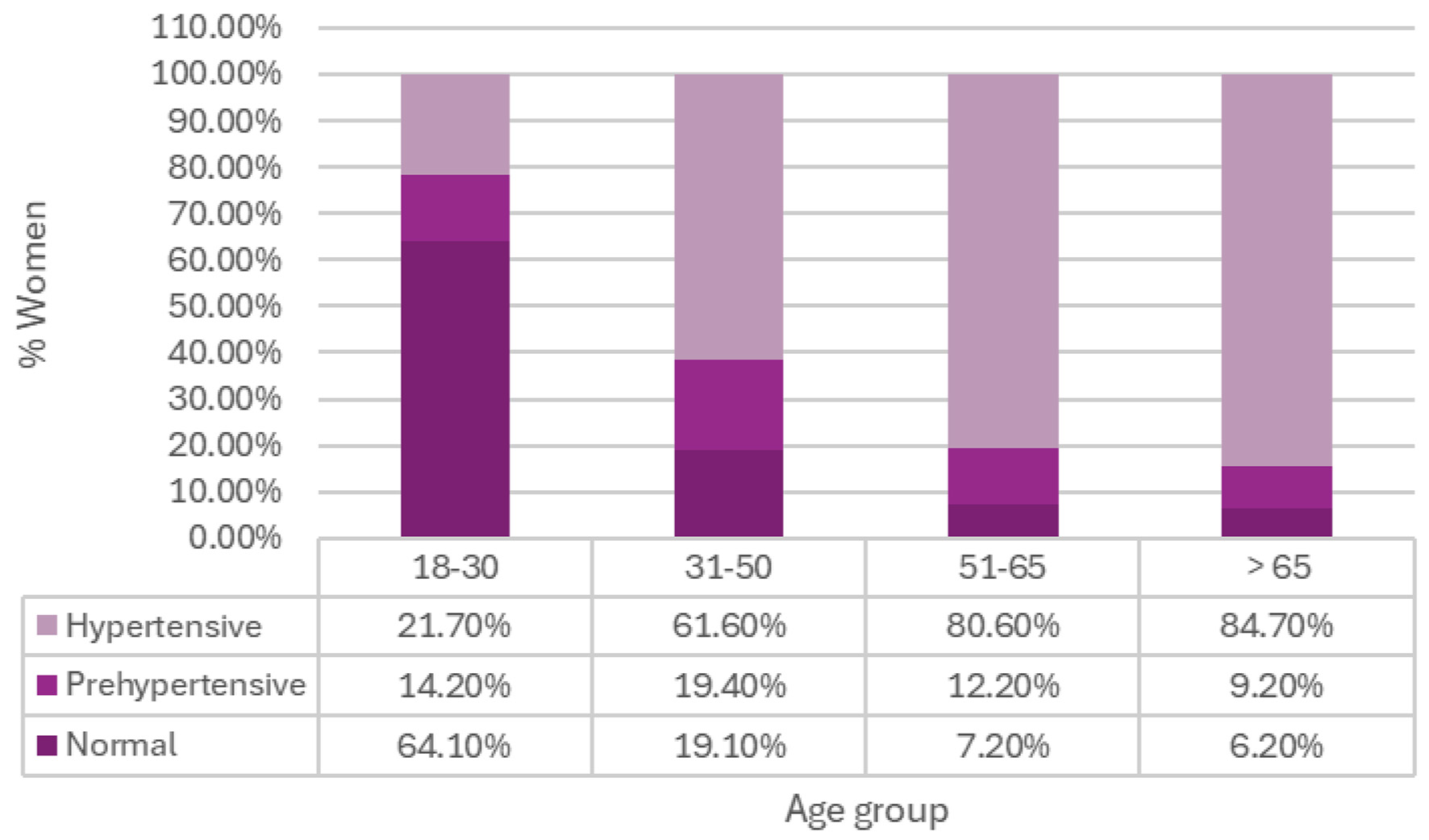 Click for large image | Figure 3. Prevalence of hypertension by age amongst women. |
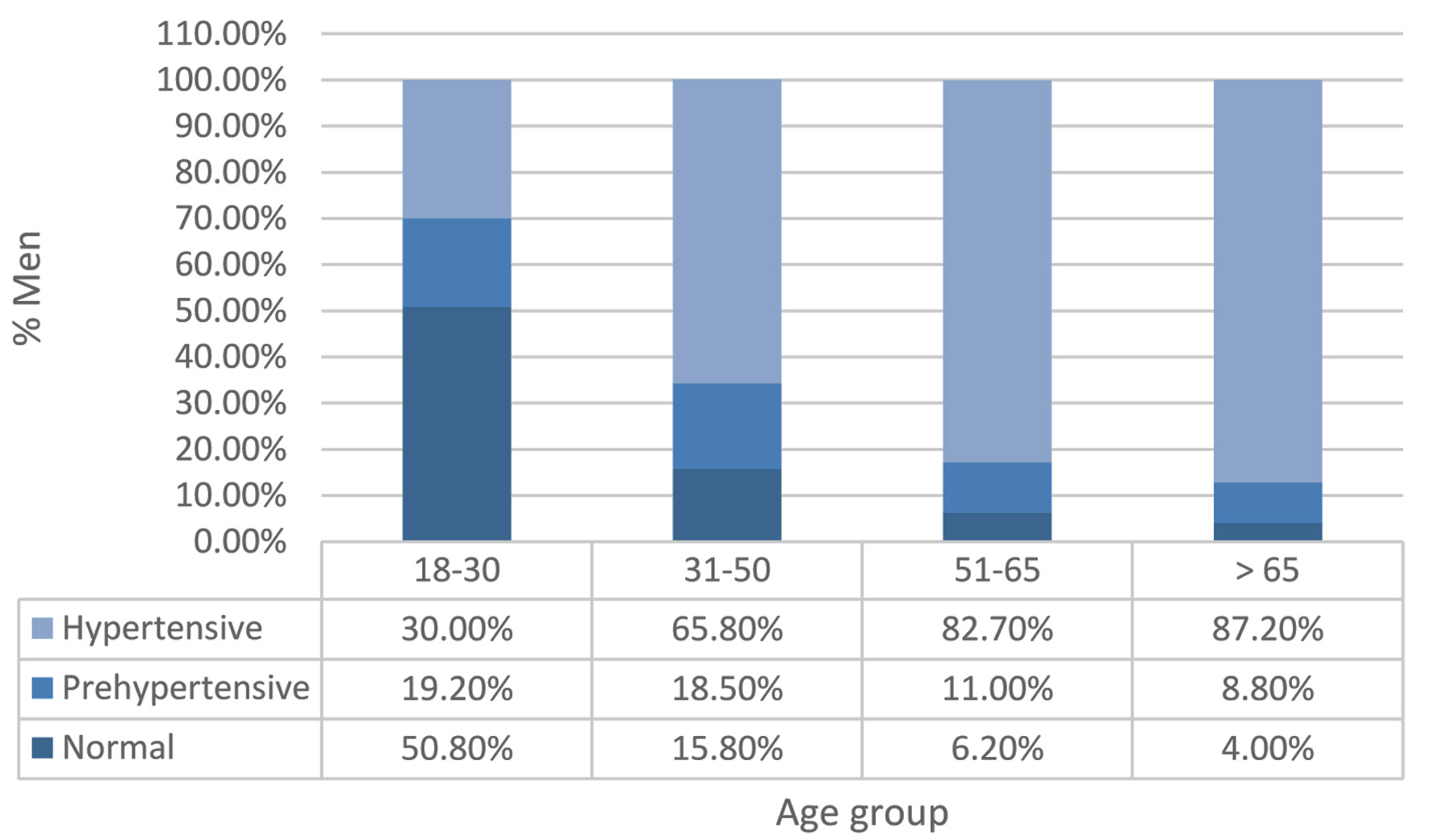 Click for large image | Figure 4. Prevalence of hypertension by age amongst men. |
Hypertension and HR
HR patterns were also evaluated across different age groups and genders (Table 5). Analysis of HR across age groups revealed a progressive rise with increasing age.
 Click to view | Table 5. Mean Heart Rate (bpm (95% CI)) by Age and Gender |
The mean HR was lowest in the 18 - 30 group (80.0 bpm) and highest among those aged ≥ 65 (84.8 bpm). Gender differences were marginal, with slightly lower HRs in young women (79.5 bpm) compared to men (80.4 bpm). By age 51 and beyond, both genders had similar HRs (approximately 84.8 bpm).
Association between diabetes, hypertension, and HR
Among the 41,370 participants, 48.4% (n = 20,005) were identified as having both diabetes and hypertension. This subgroup exhibited a significantly higher mean HR (85.86 ± 11.12 bpm) compared to participants without diabetes (82.15 ± 10.46 bpm). This difference was statistically significant (P < 0.05) (Table 6).
 Click to view | Table 6. Comparison of Heart Rate Between Diabetic and Non-Diabetic Hypertensive Participants |
Adjusted predictors of hypertension and diabetes
Beyond descriptive analyses, we performed multivariable logistic regression to adjust for potential confounders (age, sex, and region) and to identify independent predictors of hypertension, diabetes, and their coexistence. Logistic regression adjusting for age, sex, and region showed that advancing age independently increased the odds of hypertension (OR 1.06, 95% CI: 1.05 - 1.06) and diabetes (OR 1.04, 95% CI: 1.04 - 1.04). Male sex was associated with higher odds of hypertension (OR 1.14, 95% CI: 1.08 - 1.20) and combined hypertension with diabetes (OR 1.16, 95% CI: 1.11 - 1.21). Regional variation was evident, with higher odds in the North (hypertension OR 1.29; diabetes OR 1.34) and South (hypertension OR 1.12; diabetes OR 1.37), and lower odds in the West (hypertension OR 0.87; diabetes OR 0.93). Importantly, comorbidity effects were strong, diabetics had nearly fivefold higher odds of hypertension (OR 4.70), while hypertensives had a similar risk of diabetes (OR 4.79). These findings confirm that advancing age and regional variation are dominant drivers of India’s hypertension and diabetes burden, with comorbidity substantially amplifying cardiovascular risk.
| Discussion | ▴Top |
The findings of this large-scale, nationwide survey highlight that nearly one in three Indian adults has hypertension, reinforcing the urgent need for clinicians to actively screen beyond traditional high-risk groups, especially in urbanizing regions. These findings provide critical insights into India’s escalating burden of hypertension and highlight the complex interplay of metabolic risk factors driving the NCD epidemic.
Although direct anthropometric measurements were not captured, the strong coexistence of diabetes, elevated resting HR, and age-related trends strongly suggests obesity as a unifying driver of cardiometabolic risk [19]. Obesity is increasingly recognized as a chronic, low-grade inflammatory condition [20], which promotes endothelial dysfunction, insulin resistance, and sympathetic overactivity, three mechanisms central to hypertension and CVD [21]. Large epidemiological studies confirm obesity as a catalyst for hypertension, type 2 diabetes, coronary artery disease, arrhythmias, and HF [22, 23]. With abdominal obesity rates rising sharply in India, clinicians should consider obesity a cardiovascular risk equivalent and proactively screen and intervene at earlier stages.
Our findings reaffirm known demographic patterns: hypertension prevalence was higher among older adults, men, and urban dwellers. Even without direct obesity data, the clustering of diabetes and elevated HR signals to metabolic syndrome and autonomic dysfunction as underlying mechanisms. The mean resting HR of 83.9 bpm in this cohort, above the ESC/ESH threshold of 80 bpm for elevated CV risk [24], particularly in those with diabetes, should be regarded by clinicians as a practical red flag for heightened sympathetic overdrive and increased CV risk [25, 26]. Indian and global evidence, consistently link elevated HR to poor outcomes [27-30], and our findings reinforce the value of incorporating HR assessment into routine hypertension care to refine risk stratification and management.
Regional disparities in hypertension prevalence, from higher rates in Himachal Pradesh and Jharkhand to lower prevalence in select Union Territories, reflect India’s diversity in lifestyle, dietary patterns, and stages of urbanization. These observations have direct public health implications; targeted, region-specific strategies may yield greater impact than uniform national approaches.
The coexistence of hypertension and diabetes across all demographic groups further signals India’s epidemiological shift toward multimorbidity. For clinicians, this underscores the importance of moving from siloed, disease-specific care models to integrated cardiometabolic management. Interventions must simultaneously address obesity, insulin resistance, and autonomic dysregulation to curb the broader cardiometabolic continuum [31]. Importantly, hypertensive individuals with controlled BP remain at higher risk if HR is elevated, with studies showing a 53% increased incidence of CV events in such cases [32]. This highlights HR as a clinically actionable marker for guiding therapy beyond BP targets [33].
Our results also resonate with earlier Indian studies, such as The BEAT survey [34], which reported a mean HR of 82.79 bpm in hypertensives, and global data identifying elevated HR as a predictor of cardiovascular morbidity and mortality, particularly in younger men. The distinct cardiovascular profile of individuals with both diabetes and hypertension, marked by consistently higher HRs, further strengthens the case for aggressive, integrated management of these high-risk patients [35, 36].
In context, this present survey complements prior national efforts such as the Great India Blood Pressure Survey [37], and extends them by adding the dimension of resting HR as a surrogate of autonomic imbalance. Together, these datasets form a robust evidence base for clinicians and policymakers to design more nuanced, high-impact interventions for hypertension and related NCDs in India.
This study has certain limitations. The absence of anthropometric and lifestyle data (e.g., diet, activity, smoking, stress, family history) limits mechanistic interpretation. Participants < 18 years were not included. As participation was voluntary, selection bias cannot be excluded. Finally, the cross-sectional design limits causal inference. Future longitudinal studies are needed to validate these associations and guide targeted intervention.
Conclusion
With data from over 41,000 participants across both urban and rural regions, this nationwide survey represents one of the most comprehensive cross-sectional assessments of hypertension, resting HR, and comorbidities such as diabetes conducted in India to date. Despite the absence of direct anthropometric measurements, the findings strongly point toward underlying metabolic dysfunction likely driven by obesity as a unifying pathway linking elevated BP, diabetes, and increased HR.
Regression analyses further emphasized that age, male sex, and regional disparities are independent determinants of hypertension and diabetes, underscoring the need for integrated, region-specific strategies in India.
Resting HR emerged as a clinically relevant surrogate for autonomic imbalance, with its elevation observed in both diabetic and non-diabetic hypertensives. This pattern underscores a broader, systemic concern: the rising prevalence of sympathetic overactivity in the Indian population. As corroborated by emerging global and Indian evidence, the dynamic interplay between obesity, insulin resistance, and autonomic dysregulation lies at the heart of the current cardiometabolic epidemic.
Taken together, these insights call for a paradigm shift in region-specific hypertension management from a BP-centric model to a more holistic, integrated approach. Also, these findings highlight the urgent need for early screening, lifestyle interventions, and community awareness, supported by longitudinal research to guide tailored public health strategies.
| Supplementary Material | ▴Top |
Suppl 1. A complete list of participating physicians.
Acknowledgments
The authors gratefully acknowledge the invaluable support and coordination provided by the data collection teams across 31 regions of India. We also extend our sincere thanks to the physicians and study coordinators who actively participated in the community-based screening initiatives. A complete list of participating physicians is provided in the Supplementary Material 1 (cr.elmerpub.com).
Financial Disclosure
This manuscript was developed with financial support from JB Chemicals & Pharmaceuticals Ltd.
Conflict of Interest
The authors declare no conflict of interest related to this study.
Informed Consent
Verbal informed consent was obtained from all participants prior to data collection.
Author Contributions
Dr HK Chopra contributed to the conception and design of the study. Dr. Anu Grover supported in the analysis of data and writing of the manuscript. All other authors critically reviewed the manuscript. All authors have read and approved the final version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article and its supplementary information file.
| References | ▴Top |
- Chopra HK, Ram CVS. Recent guidelines for hypertension. Circ Res. 2019;124(7):984-986.
doi pubmed - India Hypertension Control Initiative - a patient-centred approach to control hypertension at the Primary care level. https://www.who.int/about/accountability/results/who-results-report-2020-mtr/country-story/2022/india-hypertension-control-initiative---a-patient-centred-approach-to-control-hypertension-at-the-primary-care-level.
- Anjana RM, Unnikrishnan R, Deepa M, Pradeepa R, Tandon N, Das AK, Joshi S, et al. Metabolic non-communicable disease health report of India: the ICMR-INDIAB national cross-sectional study (ICMR-INDIAB-17). Lancet Diabetes Endocrinol. 2023;11(7):474-489.
doi pubmed - Chopra HK, Kumar V. HTN to HFpEF and left atriopathy: advanced therapeutic navigation. In: Chopra HK, Nanda NC, Narula J, Wander GS, Bajaj S, Kumar V, et al., editors. Textbook of Cardiology Advances in HFpEF Management. New Delhi: Jaypee Brothers Medical Publishers; 2024.
- Amarchand R, Kulothungan V, Krishnan A, Mathur P. Hypertension treatment cascade in India: results from National Noncommunicable Disease Monitoring Survey. J Hum Hypertens. 2023;37(5):394-404.
doi pubmed - Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, Prabhakaran D. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170-1177.
doi pubmed - Srikant S, Chopra HK. NT Pro BNP: diagnostic, prognostic and therapeutic implication. In: Chopra HK, Nanda NC, Narula J, Wander GS, Manjunath CN, Chandra P (eds) Textbook of Cardiology Hypertension: New Frontiers. New Delhi: Jaypee Brothers Medical Publishers. 2021.
- Dhawan N, Chopra HK. Nosie pollution, hypertension and HFpEF. In: Chopra HK, Nanda NC, Narula J, Wander GS, Bajaj S, Kumar V, et al., editors. Textbook of Cardiology Advances in HFpEF Management. New Delhi: Jaypee Brothers Medical Publishers. 2024.
- Sawhney J, Chopra HK. Power and promise of home BP monitoring. In: Chopra HK, Nanda NC, Narula J, Wander GS, Manjunath CN, Chandra P (eds) Textbook of Cardiology Hypertension: New Frontiers. New Delhi: Jaypee Brothers Medical Publishers. 2021.
- Prakash R, Chopra HK. Hypertension in patients undergoing percutaneous coronary intervention. In: Chopra HK, Nanda NC, Narula J, Wander GS, Manjunath CN, Chandra P (eds) Textbook of Cardiology Hypertension: New Frontiers. New Delhi: Jaypee Brothers Medical Publishers. 2021.
- Chopra H, Kaur S, Sambi RS. Potbelly—the most powerful predictor of metabolic syndrome and premature morbidity and mortality. Indian Heart J. 2007;59(1):56-63.
pubmed - Chopra HK, Aggarwal KK, Krishna CK, Sambi RS, Parashar SK, Gupta R, Kasliwal RR, et al. 3D echocardiography: "The most powerful predictor of masked CVD in metabolic syndrome". Indian Heart J. 2009;61(3):231-241.
pubmed - Sambi RS, Gaur AK, Hotchandani R, Aggarwal KK, Kaur S, Gupta M, Jain S, et al. Patterns of left ventricular hypertrophy in chronic kidney disease: an echocardiographic evaluation. Indian Heart J. 2011;63(3):259-268.
pubmed - Chopra HK. Diastolic heart failure: a clinical challenge early recognition & timely intervention is the need of the hour. Indian Heart J. 2009;61(2):138-145.
pubmed - Sahadevan P, Kamal VK, Sasidharan A, Bagepally BS, Kumari D, Pal A. Prevalence and risk factors associated with undiagnosed diabetes in India: Insights from NFHS-5 national survey. J Glob Health. 2023;13:04135.
doi pubmed - World Hypertension Day. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/About/world-hypertension-day.
- Shah SN, Munjal YP, Kamath SA, Wander GS, Mehta N, Mukherjee S, Kirpalani A, et al. Indian guidelines on hypertension-IV (2019). J Hum Hypertens. 2020;34(11):745-758.
doi pubmed - Pareek A, Messerili FH, Ram VS, Chopra HK. Impaired pressure natriuresis and its clinical implications from uncontrolled hypertension to heart failure. In: Chopra HK, Nanda NC, Narula J, Wander GS, Bajaj S, Kumar V, et al., editors. Textbook of Cardiology Advances in HFpEF Management. New Delhi: Jaypee Brothers Medical Publishers. 2024.
- Brown OI, Drozd M, McGowan H, Giannoudi M, Conning-Rowland M, Gierula J, Straw S, et al. Relationship among diabetes, obesity, and cardiovascular disease phenotypes: a UK biobank cohort study. Diabetes Care. 2023;46(8):1531-1540.
doi pubmed - Khanna D, Khanna S, Khanna P, Kahar P, Patel BM. Obesity: a chronic low-grade inflammation and its markers. Cureus. 2022;14(2):e22711.
doi pubmed - Tysoe O. Obesity induces systemic insulin resistance via endothelium-specific insulin receptor inhibition. Nat Rev Endocrinol. 2025;21(4):199.
doi pubmed - Babu GR, Murthy GVS, Ana Y, Patel P, Deepa R, Neelon SEB, Kinra S, et al. Association of obesity with hypertension and type 2 diabetes mellitus in India: A meta-analysis of observational studies. World J Diabetes. 2018;9(1):40-52.
doi pubmed - Chopra I, Kamal KM, Candrilli SD, Kanyongo G. Association between obesity and therapeutic goal attainment in patients with concomitant hypertension and dyslipidemia. Postgrad Med. 2014;126(1):66-77.
doi pubmed - Grassi G, Dell'Oro R, Quarti-Trevano F, Vanoli J, Oparil S. Sympathetic Neural Mechanisms in Hypertension: Recent Insights. Curr Hypertens Rep. 2023;25(10):263-270.
doi pubmed - Reule S, Drawz PE. Heart rate and blood pressure: any possible implications for management of hypertension? Curr Hypertens Rep. 2012;14(6):478-484.
doi pubmed - Padmanabhan TN, Dani S, Chopra VK, Guha S, Vasnawala H, Ammar R. Prevalence of sympathetic overactivity in hypertensive patients - a pan India, non-interventional, cross sectional study. Indian Heart J. 2014;66(6):686-690.
doi pubmed - Rao D, Balagopalan JP, Sharma A, Chauhan VC, Jhala D. BEAT survey: a cross-sectional study of resting heart rate in young (18-55 Year) hypertensive patients. J Assoc Physicians India. 2015;63(5):14-17.
pubmed - Gupta R, Gaur K, Ahuja S, Anjana RM. Recent studies on hypertension prevalence and control in India 2023. Hypertens Res. 2024;47(6):1445-1456.
doi pubmed - Daniel RA, Haldar P, Prasad M, Kant S, Krishnan A, Gupta SK, Kumar R. Prevalence of hypertension among adolescents (10-19 years) in India: a systematic review and meta-analysis of cross-sectional studies. PLoS One. 2020;15(10):e0239929.
doi pubmed - Abariga SA, Khachan H, Al Kibria GM. Prevalence and determinants of hypertension in India based on the 2017 ACC/AHA guideline: evidence from the india national family health survey. Am J Hypertens. 2020;33(3):252-260.
doi pubmed - Brar V, Kandala NB, Terry A, Thind A. Predictors of multimorbidity (Defined as Diabetes + Hypertension) amongst males aged 15-54 in India: an urban/rural split analysis. Int J Public Health. 2024;69:1606660.
doi pubmed - Julius S, Palatini P, Kjeldsen SE, Zanchetti A, Weber MA, McInnes GT, Brunner HR, et al. Usefulness of heart rate to predict cardiac events in treated patients with high-risk systemic hypertension. Am J Cardiol. 2012;109(5):685-692.
doi pubmed - Benetos A, Rudnichi A, Thomas F, Safar M, Guize L. Influence of heart rate on mortality in a French population: role of age, gender, and blood pressure. Hypertension. 1999;33(1):44-52.
doi pubmed - Dalal J, Dasbiswas A, Sathyamurthy I, Maddury SR, Kerkar P, Bansal S, Thomas J, et al. Heart rate in hypertension: review and expert opinion. Int J Hypertens. 2019;2019:2087064.
doi pubmed - Huggett RJ, Scott EM, Gilbey SG, Stoker JB, Mackintosh AF, Mary DA. Impact of type 2 diabetes mellitus on sympathetic neural mechanisms in hypertension. Circulation. 2003;108(25):3097-3101.
doi pubmed - Coats AJ, Cruickshank JM. Hypertensive subjects with type-2 diabetes, the sympathetic nervous system, and treatment implications. Int J Cardiol. 2014;174(3):702-709.
doi pubmed - Ramakrishnan S, Zachariah G, Gupta K, Shivkumar Rao J, Mohanan PP, Venugopal K, Sateesh S, et al. Prevalence of hypertension among Indian adults: Results from the great India blood pressure survey. Indian Heart J. 2019;71(4):309-313.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.