| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Review
Volume 16, Number 6, December 2025, pages 475-478
Exercise Oscillatory Ventilation: A Potential New Risk Factor for Sudden Cardiac Death in Hypertrophic Cardiomyopathy
Stefanos G. Sakellaropoulosa, b, c, l, Muhemin Mohammedc, d, Panagiotis Sakellaropoulose, Muhammad Alif, Athanasios Papadisc, Ilias Piperopoulosg, Eugenia Kloufetouh, Benedict Schulte Steinbergi, Claire Rogersj, Andreas Mitsisk
aDepartment of Cardiology, University Hospital and University of Basel, Basel, Switzerland
bDepartment of Internal Medicine, Medical Center of Wurenlingen, Wurenlingen, Switzerland
fClinic of Cardiology Salzgitter, Salzgitter, Germany
cSwiss Cardiovascular Centre, Bern University Hospital, Bern, Switzerland
dClinic of Internal Medicine, Hospital Affoltern, Affoltern, Switzerland
eDepartment of Biopathology and Medical Biochemistry, Kalamata General Hospital, Kalamata, Greece
gDepartment of Microbiology, General Hospital of Xanthi, Xanthi, Greece
hDepartment of Neurology, University Hospital of Ioannina, Ioannina, Greece
iDepartment of Cardiology and Angiology, Robert Bosch Hospital, Baden-Wurttemberg, Germany
jDepartment of Cardiology and Angiology, SRH Health Center Bad Herre-nalb, Bad Herrenalb, Germany
kDepartment of Cardiology, Nicosia General Hospital, Nicosia, Cyprus
lCorresponding Author: Stefanos G. Sakellaropoulos, Department of Cardiology, University Hospital and University of Basel, Basel, Switzerland
Manuscript submitted August 11, 2025, accepted October 24, 2025, published online December 20, 2025
Short title: EOV as a Risk Marker for SCD in HCM
doi: https://doi.org/10.14740/cr2131
- Abstract
- Introduction and Pathophysiology of Exercise Oscillatory Ventilation (EOV)
- Definition
- Reversibility of EOV
- Heart Rate Variability (HRV) and Respiratory Variability
- EOV in HCM and Future Aspects
- References
| Abstract | ▴Top |
Other than the traditional risk factors for sudden cardiac death (SCD) in hypertrophic cardiomyopathy (HCM) - detected by means of anamnesis, Holter monitoring, exercise testing, echocardiography and cardiac magnetic resonance imaging - exercise oscillatory ventilation (EOV), detected by cardiopulmonary exercise testing (CPET), has recently been observed in patients with HCM. EOV is considered as one of the most important independent risk factors for morbidity, mortality and SCD in patients with reduced, as well as with preserved ejection fraction. Considering HCM as a prototype of heart failure with preserved ejection fraction, we would like to present a short, specific review concerning EOV as a potential new risk factor for SCD in HCM.
Keywords: Exercise oscillatory ventilation; Hypertrophic cardiomyopathy; Heart failure
| Introduction and Pathophysiology of Exercise Oscillatory Ventilation (EOV) | ▴Top |
The pathomechanism of EOV is in essence based on a disturbed feedback loop between the pulmonary system, peripheral chemoreceptors in the carotid arteries, and the central respiratory receptors in the medulla oblongata. This implies that instability in any of these regulatory factors leading to an unstable ventilatory regulation can give rise to breathing oscillation pattern.
The study from Corra et al showed that EOV is not present in healthy individuals; EOV was observed only in cardiovascular disease (CVD) patients and in those with depressed left ventricular ejection fraction (LVEF) [1].
This kind of instability may be caused by 1) delay in circulation; 2) system damping reduction; or 3) an increase in controller gain [2-4].
As described by Dhakal et al in patients with heart failure, a reduced cardiac output prolongs circulation time “from lungs to chemoreceptors and respiratory centers” and leads to a consequential delay of feedback signals from respiratory chemoreceptors, which leads to ventilatory instability [5].
Increase in controller gain refers to an increased sensitivity of the peripheral and central receptors responding to changes in arterial partial pressure of arterial carbon dioxide (PaCO2) and partial pressure of arterial oxygen (PaO2), which also leads to a pathological ventilatory regulation [5].
The study by Pardaens et al demonstrated that ergoreflex activity gives rise to hyperventilation in patients with recent heart failure decompensation or active heart failure symptoms. Output oscillations originating from neurologenic triggering within the medullary vasomotor center are considered the primary cause of the disappearance of respiratory oscillations found at rest or at low levels during intense exercise [6].
Furthermore, delay of respiratory and pulmonary blood flow during exercise, in comparison to fluctuations in patients with reduced LVEF, also attenuates delayed circulation, leading to changes in respiratory feedback mechanisms [7]. Moreover, based on recent studies, chest wall conformation influences ventilatory oscillations. Specifically, patients with pectus excavatum exhibit reduced mechanical capacity for oscillatory breathing. If so, this anatomic variation may give rise to attenuated EOV and correspondingly lower risk of SCD [8]. Investigating whether thoracic morphology modulates the prevalence or severity of EOV could refine the predictive value of cardiopulmonary exercise testing (CPET) in hypertrophic cardiomyopathy (HCM).
| Definition | ▴Top |
The length of an oscillation cycle in ventilation is defined as the time between two oscillations nadirs. Furthermore, oscillation amplitude is the difference between the peak ventilation of oscillation and the nadirs (Fig. 1) [9]. Several definitions exist, which are summarized in Table 1 [2, 10-13, 14].
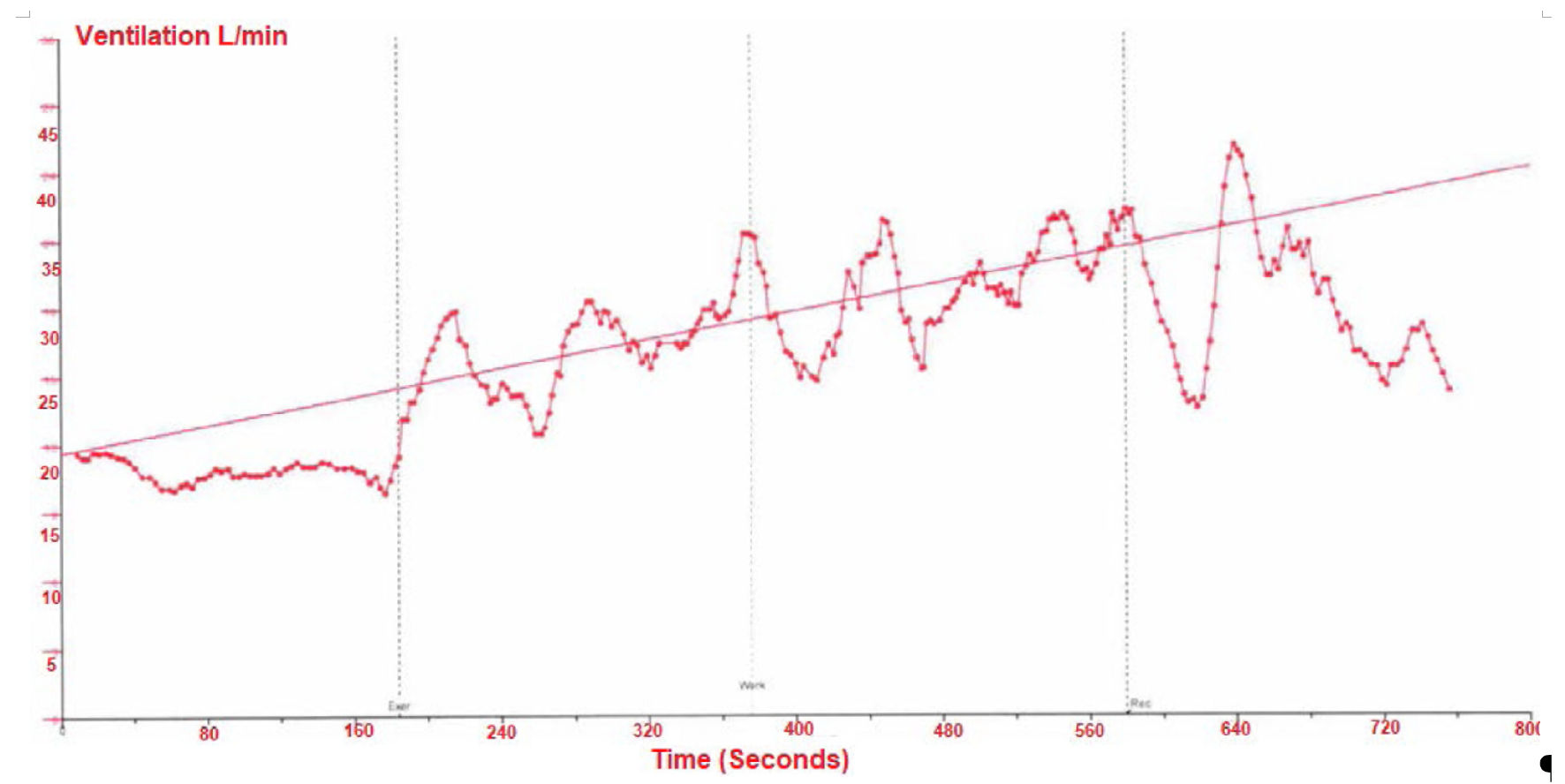 Click for large image | Figure 1. Exercise oscillatory ventilation (EOV). The length of an oscillation cycle in ventilation is defined as the time between two oscillations nadirs. Furthermore, oscillation amplitude is the difference between the peak ventilation of oscillation and the nadirs [19]. |
 Click to view | Table 1. Criteria for EOV |
| Reversibility of EOV | ▴Top |
Few small studies have demonstrated the reversibility of EOV with various therapeutic measures. Ribeiro et al [15] noticed reversibility of EOV with a phosphodiesterase-3 inhibitor. Furthermore, Castro et al [16] showed EOV reversal as well as improvement in New York Heart Association (NYHA) class with exercise training, although there was no improvement in LVEF.
Moreover, in a study by Marcus et al, using pacing-induced chronic heart failure (CHF) rabbit models, denervation of chemoreceptor in carotid bodies reduced oscillatory breathing patterns [17].
| Heart Rate Variability (HRV) and Respiratory Variability | ▴Top |
HRV is known to be related to average heart rate (HR) and respiratory rate. Any alterations of these two important parameters may give rise to changes in HRV [18].
The study by Gasior et al demonstrated that respiratory rate and HR influence HRV; however, the influence of breathing rate is HR-dependent. The correction of HRV for the HR decreases the association between respiratory rate and HRV [18].
And so, HR appears to be a main leading factor of reproducibility of HRV [18].
| EOV in HCM and Future Aspects | ▴Top |
As aforementioned, EOV has been investigated in patients with systolic and diastolic heart failure and is recognized as an independent risk factor for cardiovascular death. Parallelly, HCM is considered as a prototypical substrate for diastolic heart failure [19].
The retrospective study by Sakellaropoulos et al identified, to our knowledge for the first time, the presence of exercise oscillatory gas exchange kinetics in HCM, with a prevalence of 5%. It is associated with overt heart failure, peak VO2 ≤ 9.1 mL/kg/min, as well as an enlarged left atrial diameter, indexed with a cutoff of 25 mm/m2 [9].
We highly recommend that further larger studies should be conducted in order to investigate the potential role of EOV in the assessment of SCD in patients with HCM. Other than the traditional risk factors for the implantation of implantable cardioverter defibrillator (ICD) as a primary prophylaxis for SCD, we support CPET to be performed routinely, in order to evaluate HCM patients due to its highly prognostic and predictive power.
Concerning treatment, studies on myosin inhibitors demonstrate excellent results in the treatment of HCM [20], and an investigation on EOV could be a very promising and productive field of research.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Author Contributions
SGS and AM have contributed to the article concerning article design, providing clinical expertise to revise critically. MM, PS, MA, AP, IP, EK, BSS and CR have equally contributed to the article concerning literacy search.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Corra U, Piepoli M, Giordano A. Difference in prevalence of exertional oscillatory ventilation between healthy subjects and patients with cardiovascular disease. Monaldi Arch Chest Dis. 2020;90(1).
doi pubmed - Leite JJ, Mansur AJ, de Freitas HF, Chizola PR, Bocchi EA, Terra-Filho M, Neder JA, et al. Periodic breathing during incremental exercise predicts mortality in patients with chronic heart failure evaluated for cardiac transplantation. J Am Coll Cardiol. 2003;41(12):2175-2181.
doi pubmed - Khoo MC, Kronauer RE, Strohl KP, Slutsky AS. Factors inducing periodic breathing in humans: a general model. J Appl Physiol Respir Environ Exerc Physiol. 1982;53(3):644-659.
doi pubmed - Andreas S, Hagenah G, Moller C, Werner GS, Kreuzer H. Cheyne-Stokes respiration and prognosis in congestive heart failure. Am J Cardiol. 1996;78(11):1260-1264.
doi pubmed - Dhakal BP, Lewis GD. Exercise oscillatory ventilation: Mechanisms and prognostic significance. World J Cardiol. 2016;8(3):258-266.
doi pubmed - Pardaens S, Vanderheyden M, Calders P, Willems AM, Bartunek J, de Sutter J. Activation of the ergoreceptors in cardiac patients with and without heart failure. J Card Fail. 2014;20(10):747-754.
doi pubmed - Agostoni P, Apostolo A, Albert RK. Mechanisms of periodic breathing during exercise in patients with chronic heart failure. Chest. 2008;133(1):197-203.
doi pubmed - Sonaglioni A, Nicolosi GL, Trevisan R, Lombardo M, Grasso E, Gensini GF, Ambrosio G. The influence of pectus excavatum on cardiac kinetics and function in otherwise healthy individuals: A systematic review. Int J Cardiol. 2023;381:135-144.
doi pubmed - Sakellaropoulos SG, Baggish AL, Fifer MA, Lewis GD. Exercise oscillatory ventilation in hypertrophic cardiomyopathy. Curr Probl Cardiol. 2022;47(5):100911.
doi pubmed - Sun XG, Hansen JE, Beshai JF, Wasserman K. Oscillatory breathing and exercise gas exchange abnormalities prognosticate early mortality and morbidity in heart failure. J Am Coll Cardiol. 2010;55(17):1814-1823.
doi pubmed - Kremser CB, O'Toole MF, Leff AR. Oscillatory hyperventilation in severe congestive heart failure secondary to idiopathic dilated cardiomyopathy or to ischemic cardiomyopathy. Am J Cardiol. 1987;59(8):900-905.
doi pubmed - Corra U, Pistono M, Mezzani A, Braghiroli A, Giordano A, Lanfranchi P, Bosimini E, et al. Sleep and exertional periodic breathing in chronic heart failure: prognostic importance and interdependence. Circulation. 2006;113(1):44-50.
doi pubmed - Ben-Dov I, Sietsema KE, Casaburi R, Wasserman K. Evidence that circulatory oscillations accompany ventilatory oscillations during exercise in patients with heart failure. Am Rev Respir Dis. 1992;145(4 Pt 1):776-781.
doi pubmed - Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, Forman D, et al. Clinician's Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(2):191-225.
doi pubmed - Ribeiro JP, Knutzen A, Rocco MB, Hartley LH, Colucci WS. Periodic breathing during exercise in severe heart failure. Reversal with milrinone or cardiac transplantation. Chest. 1987;92(3):555-556.
doi pubmed - Castro RR, Antunes-Correa LM, Ueno LM, Rondon MU, Negrao CE, Nobrega AC. Reversal of periodic breathing after aerobic training in heart failure. Eur Respir J. 2010;35(6):1409-1411.
doi pubmed - Marcus NJ, Del Rio R, Schultz EP, Xia XH, Schultz HD. Carotid body denervation improves autonomic and cardiac function and attenuates disordered breathing in congestive heart failure. J Physiol. 2014;592(2):391-408.
doi pubmed - Gasior JS, Sacha J, Jelen PJ, Zielinski J, Przybylski J. Heart rate and respiratory rate influence on heart rate variability repeatability: effects of the correction for the prevailing heart rate. Front Physiol. 2016;7:356.
doi pubmed - Sakellaropoulos SG, Steinberg BS. Hypertrophic cardiomyopathy: a cardiovascular challenge becoming a contemporary treatable disease. Cardiol Res. 2023;14(4):243-249.
doi pubmed - Lekaditi D, Sakellaropoulos S. Myosin Modulators: The new era of medical therapy for systolic heart failure and hypertrophic cardiomyopathy. Cardiol Res. 2021;12(3):146-148.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.