Achieving Neuroprotection in the Setting of Early Extubation During Infant Cardiac Surgery: A Prospective, Randomized, and Blinded Study
DOI:
https://doi.org/10.14740/cr2029Keywords:
Fast tracking, Early extubation in pediatric cardiac surgery, Stress response, Neurodevelopmental outcomeAbstract
Background: This study aimed to investigate the impact of early extubation on stress response and neurodevelopmental outcomes after pediatric cardiac surgery utilizing cardiopulmonary bypass (CPB).
Methods: In this single-center prospective pilot study, we attempted to study the impact of using dexmedetomidine as an adjunct to facilitate early extubation after pediatric cardiac surgery requiring CPB during the first year of life. The study was conducted between May 2014 and January 2020. Perioperative data and stress hormone levels were collected at different points during the perioperative period. In addition, neurodevelopmental outcome measures including cognitive composite score, language (expressive and receptive) and motor (fine and gross) composites were evaluated at five time points including prior to surgery and up to 1 year after the procedure. Two-sample t-tests and Kruskal-Wallis tests were used to compare continuous parametric and non-parametric outcomes, respectively. Fisher’s exact or Chi-squared tests were used to compare categorical outcomes.
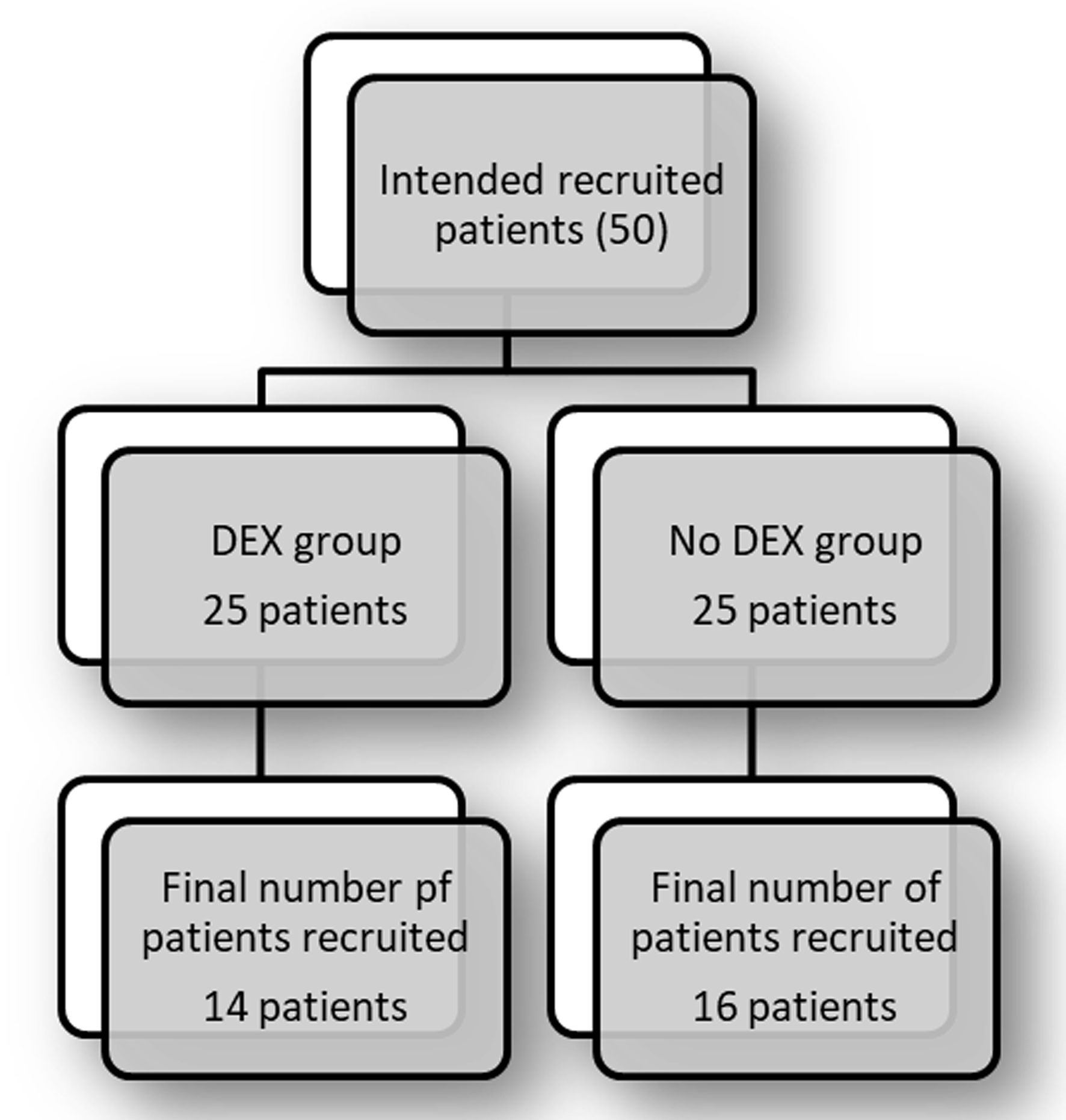
Results: A total of 30 subjects were included in the final cohort of patients. Of the 30 subjects, 14 patients were randomized to the dexmedetomidine group (dexmedetomidine plus fentanyl) (DEX group) and 16 patients were randomized to the no dexmedetomidine group (fentanyl only) (no DEX group). With few exceptions, both groups demonstrated appropriate blunting of the stress response. There was a significant increase in the ratio of the pro-inflammatory interleukin-10 (IL-10) to the anti-inflammatory interleukin-6 (IL-6) for the no DEX group at the end of the procedure when compared to the DEX group (10 ± 9 vs. 5 ± 4, P = 0.04). When looking at the Bayley cognitive composite score, the DEX group scored better than the no DEX group during the second visit (102 ± 11 vs. 88 ± 17, P = 0.023). By the fifth visit, the two groups scored similarly (94 ± 12 vs. 94 ± 12, P = 0.9 for the no DEX and DEX groups, respectively).
Conclusion: When looking at the neurodevelopmental outcome, our cohort had no significant changes in their Bayley scores from baseline with blunting of most stress markers. This study offers possible evidence of the safety of early extubation after pediatric cardiac surgery while maintaining the goal of neuroprotection.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.









