Effect of Angiotensin Receptor-Neprilysin Inhibitor in Patients With Heart Failure: A Real-World Study
DOI:
https://doi.org/10.14740/cr2074Keywords:
N-terminal pro-brain natriuretic peptide, Angiotensin receptor-neprilysin inhibitor, Heart failure with reduced left ventricular ejection fraction, Blood pressureAbstract
Background: This study evaluated the cardioprotective effects of angiotensin receptor-neprilysin inhibitor (ARNI) therapy in patients with heart failure (HF), focusing on blood pressure (BP) and cardiac or renal function.
Methods: A total of 46 patients who started ARNI therapy between December 2020 and March 2023 were included. Blood tests, echocardiography, and assessments of BP and cardiac function including N-terminal pro-brain natriuretic peptide (NT-proBNP) in blood were performed before and 6 months after they started ARNI therapy. The patients were divided into two groups: heart failure with reduced left ventricular (LV) ejection fraction (HFrEF) and non-HFrEF.
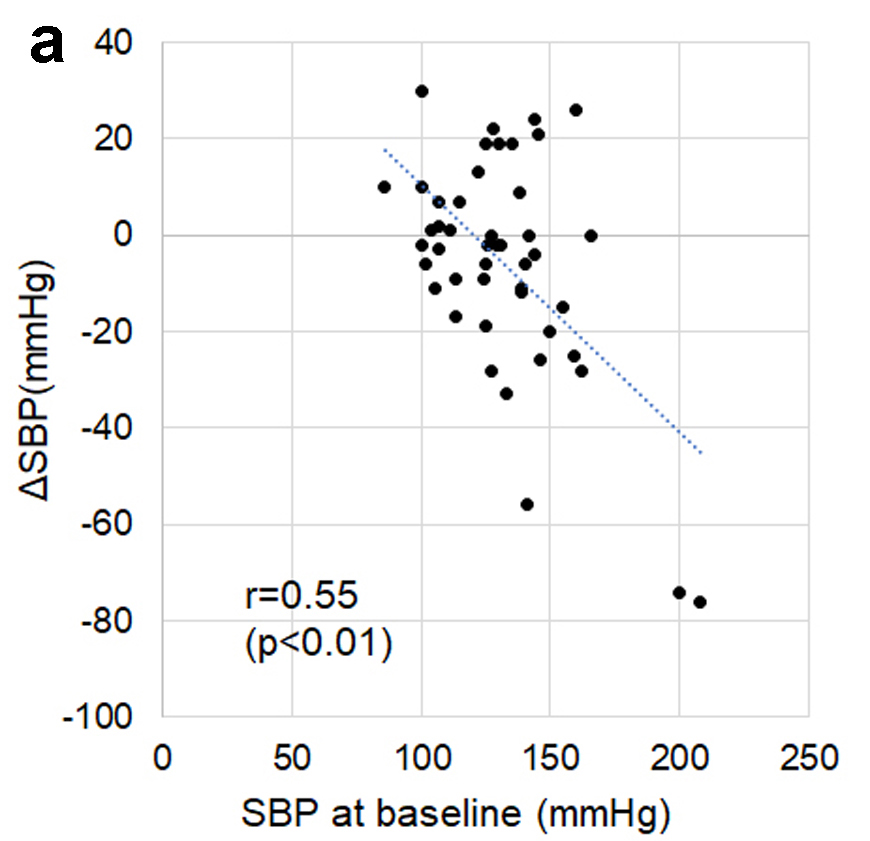
Results: Before treatment, the mean NT-proBNP level was 550 pg/mL, LVEF was 45%, and the estimated glomerular filtration rate (eGFR) was 52.7 mL/min/1.73 m2 in all patients. After 6 months of ARNI therapy, NT-proBNP levels significantly decreased to 462 pg/mL (P < 0.01), LVEF improved to 52% (P < 0.01), and BP showed a slight reduction, particularly in patients with high baseline BP. eGFR remained stable (P = 0.53). The results showed that ARNI treatment led to a reduction in NT-proBNP and improvements in cardiac function, with more pronounced effects in patients with HFrEF. BP changes correlated with baseline levels, stabilizing at around 125/70 mm Hg, and there were no significant differences in renal function between HFrEF and non-HFrEF patients.
Conclusions: ARNI therapy significantly reduced NT-proBNP levels and improved cardiac function, with mild antihypertensive effects and no major impact on renal function. These results highlight the importance of predicting the degree of BP reduction by BP at baseline before starting ARNI in HF patients.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.









