| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 000, Number 000, April 2025, pages 000-000
Complex Interactions of Social Determinants of Health on Survival Outcomes in Hispanic Patients With Pulmonary Arterial Hypertension in a US-Mexican Border City
Hedaia Algheriania, f, Marco Cazares-Parsona, Michael Brockmana, Bobak Zakhirehb, Sunil Srinivasc, Debabrata Mukherjeec, Alok K. Dwivedid, Nils P. Nickele
aDepartment of Internal Medicine, Texas Tech University Health Sciences Center El Paso, El Paso, TX, USA
bPaul L. Foster School of Medicine, El Paso, TX, USA
cDepartment of Internal Medicine, Division of Cardiology, Texas Tech University Health Sciences Center El Paso, El Paso, TX, USA
dDivision of Biostatistics and Epidemiology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso, TX, USA
eDepartment of Internal Medicine, Division of Pulmonary and Critical Care, Texas Tech University Health Sciences Center El Paso, El Paso, TX, USA
fCorresponding Author: Hedaia Algheriani, Department of Internal Medicine, Texas Tech University Health Sciences Center El Paso, El Paso, TX 79905, USA
Manuscript submitted October 31, 2024, accepted March 6, 2025, published online April 22, 2025
Short title: SDOH on Survival in Patients With PAH
doi: https://doi.org/10.14740/cr1748
| Abstract | ▴Top |
Background: Pulmonary arterial hypertension (PAH) is a chronic disease of the pulmonary blood vessels that can lead to right heart failure, resulting in increased morbidity and mortality if left untreated. While right heart hemodynamics and functional capacity are a well-established predictors of outcome in PAH, emerging evidence suggests that social determinants of health (SDOH) may have a significant impact on patients with PAH, influencing outcomes and survival rates. This study explores the impact of SDOH and their intricate interactions on survival among a Hispanic patient cohort along the US-Mexico border.
Methods: A retrospective analysis was conducted on a single-center cohort of 158 PAH patients (72% female, mean age 58 years) using Cox proportional hazards models and latent class analyses. The primary outcome was mortality during the follow-up period, with secondary analyses examining the impact of individual and combined SDOH on survival.
Results: During a mean follow-up period of 3.8 years (range: 0.2 to 6 years), 37 patients (23.4%) died. Lack of health insurance (hazard ratio (HR) 2.17; 95% confidence interval (CI): 1.05 - 4.49, P = 0.037) and unemployment (HR 2.99; 95% CI: 1.42 - 6.30, P = 0.004) were significantly associated with a higher risk of death within 5 years of follow-up. Latent variable modeling revealed that patients aged ≥ 60 years, who were uninsured, unmarried, and unemployed along with greater PAH severity (measured with cardiac output, mean pulmonary arterial pressure, six-minute walk distance, and World Health Organization Functional Class > 2) had the highest risk of poor outcomes (HR 3.6, 95% CI: 1.9 - 6.8, P < 0.001). Interestingly, the type of insurance did not have a significant impact on survival.
Conclusion: The findings underscore the critical need for improved access to insurance coverage and enhanced social support to promote better health outcomes among this vulnerable Hispanic population. Addressing these SDOH is essential in closing the health disparity gap and improving survival rates in PAH patients.
Keywords: Pulmonary arterial hypertension; Social determinants of health; Health insurance; Employment status; Social support; Hispanic population; Health disparity
| Introduction | ▴Top |
Pulmonary arterial hypertension (PAH) is a chronic, progressive disease that can lead to right heart failure and death if left untreated. Significant progress has been made in the understanding of the pathophysiology and pathology of PAH [1, 2]. However, it is now evident that, besides the biological aspects of the disease, racial and socioeconomic factors play an important role in patient outcomes. Social determinants of health (SDOH) are factors outside the scope of medical care, such as income, religion, insurance status, social support structures, and language barriers [3]. Emerging evidence indicates that a considerable number of deaths in the USA can be linked to SDOH, highlighting potential risk factors that may be modifiable. Unfortunately, Hispanic patients are disproportionately affected by these SDOH, due to prevalent poverty rates, lower rates of insurance enrollment, poor education, and language barriers [4]. Furthermore, Hispanic patients with pulmonary hypertension (PH) are currently underrepresented in most randomized clinical trials (RCTs) and international patient registries [5-7]. Therefore, there is uncertainty when it comes to the diagnosis, management, and prognostication of Hispanic patients with PAH [8]. There is a particular lack of data regarding the impact of SDOH on survival outcomes in this patient population.
We sought to evaluate how readily obtainable SDOH, including language, marital status, employment, insurance coverage, and religious affiliation, may affect the 5-year survival rates of Hispanic patients with PAH from a single center located at the US-Mexican border. The goal of this study was to identify SDOH profiles that are linked to the highest risk of adverse clinical outcomes. We aim to use these findings to make well-informed recommendations for healthcare interventions that improve survival outcomes for these high-risk patient groups.
| Materials and Methods | ▴Top |
Study population
This single-center retrospective cohort study was conducted at University Medical Center (UMC) and Texas Tech University Health Sciences Center in El Paso, situated at the US-Mexican border, providing access to all advanced PAH-targeted therapies. Patients were enrolled in this registry either as inpatients with outpatient follow-up or as outpatients. The inclusion criteria were self-reported Hispanic ethnicity, a diagnosis of WHO group 1, and data on demographics, hemodynamics, functional class, six-minute walk distance (6MWD), primary language, marital status, employment, insurance status, religion, and clinical outcomes. The exclusion criteria were loss to follow-up or incomplete data on the above-mentioned variables. Between January 2015 and December 2023, 242 patients with PAH were registered in the local database, and 158 patients met all the inclusion criteria (Supplementary Figure 1, cr.elmerpub.com).
Outcome and SDOH
The outcome of interest was 5-year overall survival. Survival was assessed from the date of the initial PAH diagnosis until the occurrence of death or referral for lung transplantation with the latter as the endpoint. The last follow-up data with no events were considered as censored events. SDOH factors, such as marital status, employment, religious affiliation, and language skills, were self-reported by patients. Insurance status was obtained through a chart review. Age and sex were also included in the analysis. Considering the size of the study, some of these nominal categorical variables were modified, for example, employment (employed vs. unemployed/retired), insurance (insured vs. uninsured), marital status (in a relationship vs. not), religion (religious vs. not), and language (English vs. Spanish). In addition, we also collected PAH clinical severity covariates, including World Health Organization Functional Classification (WHO-FC, > 2 vs. ≤ 2), 6MWD, mean pulmonary pressure (mPAP), and cardiac output (CO) (Supplementray Tables 1, 2, cr.elmerpub.com). PAH was classified according to and treated based on disease severity and current guidelines [9] (Supplementary Tables 3, 4, cr.elmerpub.com).
Statistical analysis
All the SDOH characteristics, such as age and sex, were summarized for the entire cohort and by death status. Age was summarized using the mean with standard deviation (SD) while time to follow-up in years was described with mean and range. All categorical variables were described as frequencies and percentages. These variables were compared between death status by using either a Chi-square test or a t-test. In the primary analysis, we restricted all analyses to 5 years of follow-up data. We used both the unadjusted and multivariable Cox proportional hazards models to determine SDOH factors associated with overall survival. Prior to developing the Cox models, the proportionality assumption was tested using the Schoenfeld test. In absence of proportionality, we developed the multivariable Cox models. Considering the number of events, we used a stepwise backward approach with a 0.15 probability of removing a covariate in the Cox model (Supplementary Table 5, cr.elmerpub.com). However, we also developed a Cox model with using only significant SDOH factors. We explored two-way interactions across all combinations of factors affecting overall survival. Considering the significant multiple interactions, a latent class model (LCM) was developed, which produced the optimum number of groupings based on all baseline characteristics. The final latent class analysis (LCA) was selected by comparing the K-class model with the K-1 class model. If there were no significant improvements in the K-class model compared to the K-1 class model, we finalized with the K-1 class model. The classes from the final LCM were associated with overall survival in the Cox model. All these results were validated with Cox models using all follow-up data. Kaplan-Meier curves and log-rank tests were used to show the survival distribution and the effect of binary factors on survival outcomes. All statistical analyses were conducted using Stata 17. A P-value of less than 0.05 was considered statistically significant result. The statistical analysis adhered to standard guidelines.
This study was reviewed and approved by the Institutional Review Board (IRB) of The Texas Tech University Health Sciences Center (TTUHC), IRB # E22054. This research involved human participants and was conducted in compliance with ethical standards set forth in the Declaration of Helsinki.
| Results | ▴Top |
We identified 158 Hispanic patients with PAH. Seventy-two percent of the patients were female, with a mean age of 58 years. The mean follow-up time was 3.8 years (range: 0.2 - 6 years), with a mean time to clinical worsening (TTCW) of 2 years, and 37 patients died during follow-up. The survival rates were 92% at 1 year, 86% at 2 years, and 82% at 3 years. The majority of patients were on dual (45%) or triple PAH-targeted therapies (49%); only 5% received monotherapy. At baseline, most patients were WHO-FC III (63.9%), the mean 6MWD was 362 m (± 107.32 m), the mPAP was 43.25 mm Hg (± 12.74 mm Hg), and the mean CO was 3.85 L/min (± 1.73 L/min). Non-survivors had significantly worse WHO-FC (P < 0.001), lower 6MWD (P < 0.001), higher mPAP (P = 0.021), and lower CO (P = 0.007). At baseline, 58% of patients reported being fluent in English, and 42% reported only Spanish as their primary language. Thirty-seven percent of patients reported being single, 35% married, 11% widowed, 10% separated, 7% divorced, and 1% living with a life partner. Seventy-six percent of the patients had health insurance, 44% were employed, and 84% reported a religious affiliation. These factors were similarly distributed according to survival status except for insurance status. Uninsured patients (45.9% vs. 16.5%) were likely to be in the death group compared to the alive group (Table 1).
 Click to view | Table 1. Baseline Characteristics in the Entire Cohort and by Death Status |
Kaplan-Meier time-to-event survival analysis revealed that lack of insurance (P = 0.001), and lack of employment (P < 0.01) were associated with poor 5-year survival (Figs. 1a and 2a). Our data did not reveal difference in survival between types of insurance (Fig. 1b). In addition, age, sex, primary language, and relationship status did not show a significant difference in overall survival at 5 years (Supplementary Figure 2, cr.elmerpub.com).
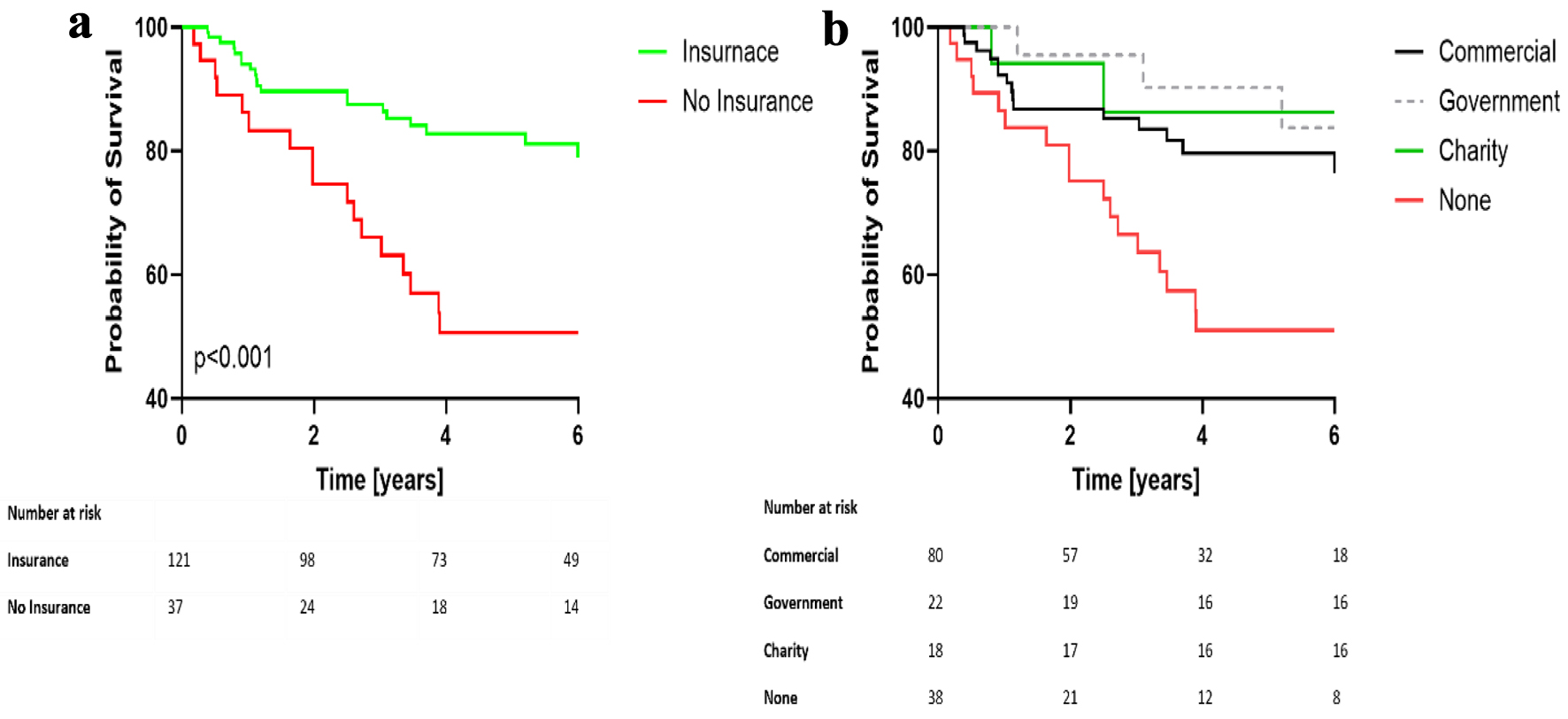 Click for large image | Figure 1. Kaplan-Meier analysis of overall survival according to insurance (a) and insurance type (b). (a) Survival probabilities for patients with and without insurance. (b) Survival rates based on insurance type. A P-value of less than 0.01 highlights a statistically significant difference among the groups. |
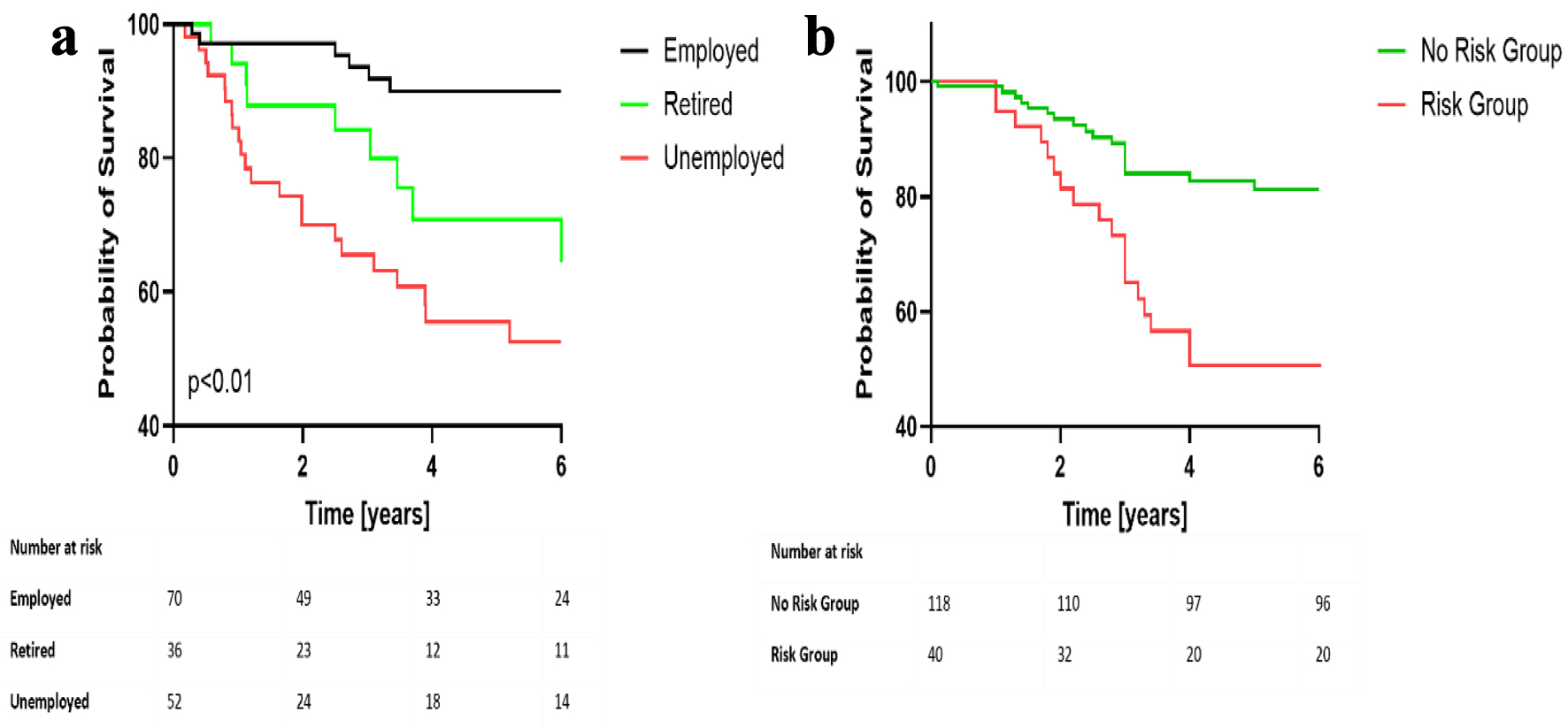 Click for large image | Figure 2. Kaplan-Meier analysis of overall survival according to employment status (a) and latent risk group (b). (a) Survival probabilities for patients based on employment status. (b) Survival probabilities based on latent risk group. A P-value of less than 0.01 indicates a statistically significant difference among the groups. |
In an unadjusted Cox regression analysis, lack of insurance had the strongest impact on poor overall survival (hazard ratio (HR) 2.92, P = 0.001) along with PAH severity measures captured as WHO-FC, 6MWD, mPAP, and CO (Table 2). In a multivariate Cox regression analysis, including all SDOH and PAH severity measures captured in this study, lack of health insurance (HR 2.17; 95% confidence interval (CI): 1.05 - 4.49, P = 0.037) and lack of employment (HR 2.99; 95% CI: 1.42 - 6.30, P = 0.004) had the strongest impact on survival (Table 3). This was further confirmed in the reduced Cox model which showed a statistically significant HR that was higher in the uninsured compared to the insured patients (Supplementary Table 1, cr.elmerpub.com). We found significant interactions between all SDOH captured in this study. Similarly, marital status interacted with religious affiliation and employment status with sex in relation to overall survival (Supplementary Table 2, cr.elmerpub.com). All PAH clinical severity measures were found to interact with SDOH factors in relation to overall survival (Supplementary Table 3, cr.elmerpub.com).
 Click to view | Table 2. Unadjusted Association of Each Factor With Overall Survival |
 Click to view | Table 3. Adjusted Association of Each Factor With Overall Survival |
Considering complex multiple interactions, LCA yielded two optimum classes, namely the low-risk class and the high-risk class. Latent risk modeling showed that patients ≥ 60 years, without insurance, unmarried, and unemployed along with PAH severity as measured by 6MWD, WHO-FC > 2, mPAP and CO had worse outcomes, compared to patients without these risk factors present (Supplementary Table 4, cr.elmerpub.com). The high-risk class consisted of patients who were not living in a relationship and were mostly uninsured. These patients were slightly older and more likely to be unemployed compared to low-risk class patients. The high-risk class patients demonstrated a significantly greater risk of mortality (HR 3.56, 95% CI: 1.87 - 6.80, P < 0.001) compared to low-risk class patients. This association remained consistent (HR 3.36; 95% CI: 1.73 - 6.53, P < 0.001) in a restricted analysis of 5-year follow-up data (Fig. 2).
| Discussion | ▴Top |
PAH is a debilitating disease that significantly impacts overall health, quality of life, and emotional and social well-being [10, 11]. It is now well recognized that, besides disease biology, measured by hemodynamic variables and functional capacity, non-physiological factors such as SDOH play a significant role in patients’ quality of life and outcomes [12]. SDOH refers to the factors in people’s daily lives that impact their health. These include their living environment, social networks and interactions, economic stability, and access to high-quality healthcare. Despite their impact on quality of life, these factors are unfortunately often overlooked when caring for patients with PAH.
In this Hispanic PAH cohort, right heart hemodynamics, functional class, and functional capacity were important predictors of 5-year mortality. However, in this cohort, SDOH also had a significant impact on survival, especially lack of insurance and employment. In the context of PAH, factors such as race, income, marital status, and gender are particularly interrelated [12]. Given the high regional variability of SDOH, we aimed to investigate easily obtainable data points in a single-center setting, to guide local management [13, 14]. We found that lack of insurance and unmarried status had the greatest impact on 5-year survival across all WHO group 1 Hispanic patients. It is interesting to note that the type of insurance was not associated with outcomes. This result is promising and should encourage the healthcare team to seek local or regional resources to obtain insurance for their patients. It is now evident that PAH has a significant negative impact on social function, as well as emotional and mental health [10]. Our data support these findings, showing that 37% were single, and only 33% were married. Notably, patients who were married had a better 5-year survival. Our data support the notion that social networks, including patient support groups, could improve HRQOL and potentially survival in PAH [15]. Bernardo et al similarly reported that Hispanic ethnicity was not associated with differences in survival after adjusting for SDOH and other factors [16]. However, Hispanic patients with PAH had a less favorable SDOH profile and had less optimal healthcare insurance, lower annual income, lower education levels, and a higher likelihood of being unemployed than non-Hispanic White patients. These and our data suggest that SDOH are important to consider when assessing the association between ethnicity and outcomes in PAH.
Over the last three decades, PAH research has mainly focused on disease biology, along with developing new and refined pharmacological treatment algorithms. However, interventions addressing SDOH have not been widely implemented in clinical practice. There is increasing evidence that a holistic, integrated community-based approach, one that integrates both the biological aspects of the disease and the individual patient’s social context, can improve outcomes in chronic diseases [17-19].
By considering factors such as insurance status, social support networks, and access to care, healthcare teams can tailor interventions to meet the unique needs of each patient. This comprehensive approach, alongside guideline-directed PAH management, could not only improve clinical outcomes but also enhance patient engagement and adherence to treatment plans. Incorporating SDOH into PAH care represents a promising avenue for advancing patient-centered medicine and addressing health disparities in vulnerable populations.
Limitations
This single-center, retrospective study includes a relatively small cohort of Hispanic patients with PAH, which limits its generalizability. Additionally, capturing SDOH is inherently challenging, and our analysis relied on self-reported data that may not fully reflect each patient’s actual living conditions. Furthermore, we did not assess clinical worsening of PAH, hospitalizations, or hospital admissions and readmission rates. Additionally, we were unable to obtain complete records regarding patient mortality, which could have markedly influenced our outcome analysis. Considering the dynamic nature of PAH and its treatment, escalation or de-escalation of PAH-specific therapies was not captured as a variable, which may have influenced patient outcomes. Consequently, our findings might have differed had we selected alternative endpoints.
Conclusions
In summary, our study shows that easily obtainable and potentially modifiable SDOH have a significant impact on outcomes in patients with PAH. We found significant interactions between PAH severity and all five SDOHs with an impact on survival. However, latent variable modeling showed that lack of insurance and lack of employment had the most significant impact on poor outcomes in our patient population.
These findings have important implications for physicians taking care of Hispanic patients with PAH. Therapeutic interventions focused on securing insurance and strengthening social networks could significantly improve outcomes for this vulnerable population.
| Supplementary Material | ▴Top |
Supplementary Table 1. Adjusted significant association of SDOH with overall survival.
Supplementary Table 2. Complex interactions between factors on overall survival.
Supplementary Table 3. Complex interactions between social determinants of health factors and clinical factors on overall survival.
Supplementary Table 4. PAH-targeted therapies.
Supplementary Table 5. Distribution of covariates by latent classes.
Supplementary Figure 1. Flowchart detailing the patient enrollment process.
Supplementary Figure 2. Kaplan-Meier survival estimates: overall survival analysis by age (A), gender (B), language (C), and marital status (D).
Acknowledgments
We would like to express our gratitude to the staff and patients of the University Medical Center Hospital and Texas Tech Pulmonology Cinic for their cooperation and support throughout this study. Special thanks to the data management team for their diligent work in maintaining and organizing the patient records.
Financial Disclosure
There was no specific funding source to be mentioned.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
All subjects provided written informed consent.
Author Contributions
NPN has designed and performed the study. HA, MPC, and MB have assisted with and supported the sample collection. NPN, HA, and BZ drafted the manuscript, and SS and DM did critical editing. AKD assisted with the subsequent statistical analysis. NPN and HA have carefully supervised the manuscript preparation and writing.
Data Availability
The authors declare that the data supporting the findings of this study are available within the article and its supplementary files.
Abbreviations
CI: confidence interval; HR: hazard ratio; HRQOL: health-related quality of life; IRB: Institutional Review Board; LCA: latent class analysis; PAH: pulmonary arterial hypertension; RCT: randomized clinical trial; SDOH: social determinants of health; TTCW: time to clinical worsening; TTUHSC: Texas Tech University Health Sciences Center; UMC: University Medical Center; WHO: World Health Organization
| References | ▴Top |
- Hemnes AR, Celermajer DS, D'Alto M, Haddad F, Hassoun PM, Prins KW, Naeije R, et al. Pathophysiology of the right ventricle and its pulmonary vascular interaction. Eur Respir J. 2024;64(4):2401321.
doi pubmed - Guignabert C, Aman J, Bonnet S, Dorfmuller P, Olschewski AJ, Pullamsetti S, Rabinovitch M, et al. Pathology and pathobiology of pulmonary hypertension: current insights and future directions. Eur Respir J. 2024;64(4):2401095.
doi pubmed - Carmichael AE, Lennon NH, Qualters JR. Analysis of social determinants of health and individual factors found in health equity frameworks: Applications to injury research. J Safety Res. 2023;87:508-518.
doi pubmed - Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, Davis D, Escamilla-Cejudo JA. Hispanic health in the USA: a scoping review of the literature. Public Health Rev. 2016;37:31.
doi pubmed - Goel K, Hon SM, Farber HW, George MP. Pulmonary arterial hypertension: what rare diseases tell us about disparities in disease registries, clinical trials, and treatment algorithms. Chest. 2021;160(5):1981-1983.
doi pubmed - Medrek SK, Sahay S. Ethnicity in pulmonary arterial hypertension: possibilities for novel phenotypes in the age of personalized medicine. Chest. 2018;153(2):310-320.
doi pubmed - Talwar A, Garcia JGN, Tsai H, Moreno M, Lahm T, Zamanian RT, Machado R, et al. Health disparities in patients with pulmonary arterial hypertension: a blueprint for action. An Official American Thoracic Society Statement. Am J Respir Crit Care Med. 2017;196(8):e32-e47.
doi pubmed - Fadah K, Cruz Rodriguez JB, Alkhateeb H, Mukherjee D, Garcia H, Schuller D, Mohammad KO, et al. Prognosis in Hispanic patient population with pulmonary arterial hypertension: An application of common risk stratification models. Pulm Circ. 2023;13(2):e12209.
doi pubmed - Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, Carlsen J, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618-3731.
doi pubmed - Delcroix M, Howard L. Pulmonary arterial hypertension: the burden of disease and impact on quality of life. Eur Respir Rev. 2015;24(138):621-629.
doi pubmed - Verma S, Cardenas-Garcia J, Mohapatra PR, Talwar A. Depression in pulmonary arterial hypertension and interstitial lung diseases. N Am J Med Sci. 2014;6(6):240-249.
doi pubmed - Grinnan D, Kang L, DeWilde C, Badesch D, Benza R, Bull T, Chakinala M, et al. Prediction of patient outcomes through social determinants of health: The Pulmonary Hypertension Association Registry (PHAR) evaluation. Pulm Circ. 2022;12(3):e12120.
doi pubmed - Singh GK, Daus GP, Allender M, Ramey CT, Martin EK, Perry C, Reyes AAL, et al. Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935-2016. Int J MCH AIDS. 2017;6(2):139-164.
doi pubmed - Zhang Y, Li J, Yu J, Braun RT, Casalino LP. Social determinants of health and geographic variation in medicare per beneficiary spending. JAMA Netw Open. 2021;4(6):e2113212.
doi pubmed - Balasubramanian A, Larive AB, Horn EM, DuBrock HM, Mehra R, Jacob MS, Hemnes AR, et al. Health-related quality of life across the spectrum of pulmonary hypertension. Chest. 2024;165(6):1493-1504.
doi pubmed - Bernardo RJ, Lu D, Ramirez RL, 3rd, Hedlin H, Kawut SM, Bull T, De Marco T, et al. Hispanic ethnicity and social determinants of health in pulmonary arterial hypertension: the pulmonary hypertension association registry. Ann Am Thorac Soc. 2022;19(9):1459-1468.
doi pubmed - Towfighi A, Cheng EM, Ayala-Rivera M, Barry F, McCreath H, Ganz DA, Lee ML, et al. Effect of a coordinated community and chronic care model team intervention vs usual care on systolic blood pressure in patients with stroke or transient ischemic attack: the SUCCEED randomized clinical trial. JAMA Netw Open. 2021;4(2):e2036227.
doi pubmed - Allen JK, Dennison-Himmelfarb CR, Szanton SL, Bone L, Hill MN, Levine DM, West M, et al. Community Outreach and Cardiovascular Health (COACH) Trial: a randomized, controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers. Circ Cardiovasc Qual Outcomes. 2011;4(6):595-602.
doi pubmed - Gary TL, Bone LR, Hill MN, Levine DM, McGuire M, Saudek C, Brancati FL. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med. 2003;37(1):23-32.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.