Long-Term Clinical Outcomes in Patients With Transthyretin Cardiac Amyloidosis Versus Non-Ischemic Cardiomyopathy
DOI:
https://doi.org/10.14740/cr2050Keywords:
Cardiac amyloidosis, Non-ischemic cardiomyopathy, Pacemaker, Transthyretin, Heart failureAbstract
Background: We sought to compare the long-term outcomes in patients with transthyretin cardiac amyloidosis (CA) compared to those with non-ischemic cardiomyopathy (NICM) from a large healthcare system database.
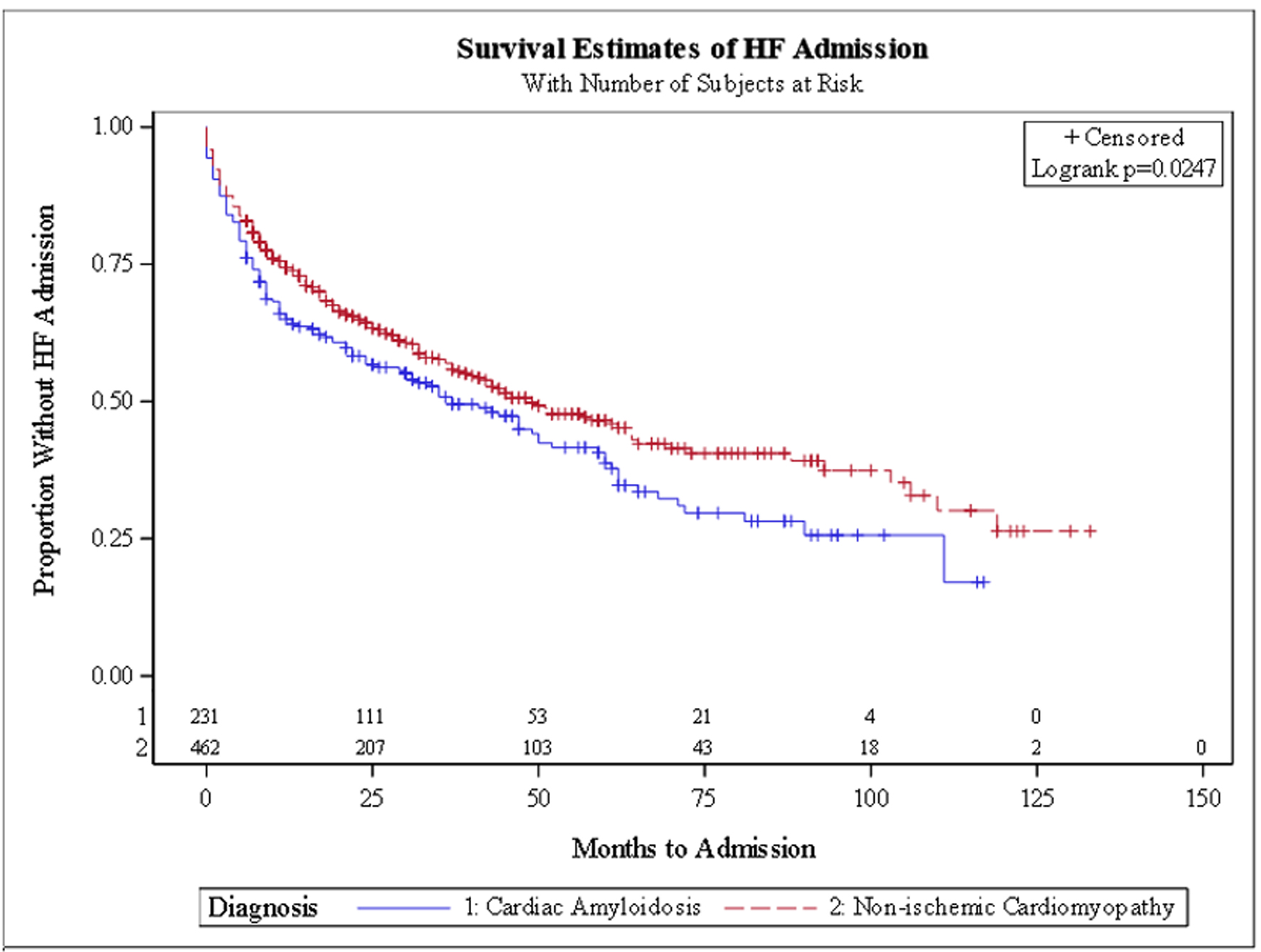
Methods: Patients with CA or NICM were identified from SSM Healthcare System’s data warehouse using ICD codes. Inclusion criteria included at least 6 months of follow-up. Outcomes studied were heart failure hospitalization (HFH), ventricular tachyarrhythmias (VTA), implantable cardiac defibrillator (ICD) and pacemaker (PM) placement. Multivariate logistic analysis and Kaplan-Meier survival curves were constructed.
Results: We identified 231 patients with CA and 462 with NICM, matched for age, race, and gender. CA patients had higher incidence of peripheral vascular disease (48.5% vs. 35.5%) and coronary artery disease (10.4% vs. 6.1%). Mean follow-up was 48.1 ± 33.1 months. CA patients had a higher rate of HFH (57.6% vs. 46.1%) and a lower rate of ICD (1.7% vs. 5.9%). In the multivariate model, CA patients had significantly higher odds for HFH (odds ratio: 1.86; 95% confidence interval: 1.29 - 2.68). Kaplan-Meier survival curves showed a trend toward earlier HFH and later PM or ICD implantation in CA patients.
Conclusions: In this retrospective study from a large healthcare system database, compared to NICM, transthyretin CA patients had significantly higher rates of HFH, similar odds of VTA, and a lower likelihood of receiving an intracardiac device.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.









