| Cardiology Research, ISSN 1923-2829 print, 1923-2837 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Cardiol Res and Elmer Press Inc |
| Journal website https://cr.elmerpub.com |
Original Article
Volume 16, Number 1, February 2025, pages 53-63<
Heart Failure and Sepsis-Related Mortality Trends in the United States, 1999 - 2019: An Analysis of Gender, Race/Ethnicity, and Regional Disparities
Olivia Foleya, b, Ali Bin Abdul Jabbara, Kimberly K. Levinea, Ahmed El-Shaera, Abubakar Tauseefa, Ahmed Aboeataa
aDepartment of Internal Medicine, Creighton University School of Medicine, Omaha, NE 68124, USA
bCorresponding Author: Olivia Foley, Department of Internal Medicine, Creighton University School of Medicine, Omaha, NE 68124, USA
Manuscript submitted November 1, 2024, accepted December 4, 2024, published online December 31, 2024
Short title: Heart Failure and Sepsis-Related Mortality
doi: https://doi.org/10.14740/cr1749
| Abstract | ▴Top |
Background: Heart failure (HF) and sepsis are significant causes of disease burden and mortality among the elderly population of the USA. HF causes fluid overload, which complicates the treatment approach when patients develop sepsis necessitating fluid resuscitation. While individual disease states have been studied extensively, the trends in mortality for concurrent sepsis and HF are not well known.
Methods: Mortality trends due to sepsis and HF in individuals aged 65 and older in the USA from 1999 to 2019 were analyzed using the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) database. Differences in age-adjusted mortality rate (AAMR) and average annual percent change (AAPC) over the past two decades based on gender, race, region, and place of death were examined.
Results: Between 1999 and 2019, there were a total of 5,887,799 deaths related to HF, 2,584,523 deaths related to sepsis, and 250,115 deaths related to both HF and sepsis. There was also a decrease in AAMR for HF-related (AAPC -0.80%) and sepsis-related (AAPC -0.28) deaths but an increase in combined HF and sepsis-related AAMR (AAPC 1.06%). Men had consistently higher AAMRs compared to women and a greater increase in mortality (AAPC in men 1.53% vs. women 0.56%). African American patients had a higher AAMR than White patients throughout the study period, though the difference narrowed. African Americans saw a decrease in overall HF and sepsis-related AAMR from 48.90 to 40.56 (AAPC -0.83), whereas AAMR for the White population increased from 27.26 to 33.81 (AAPC 1.37). Regionally, the Northeast had the highest AAMR in 1999 (32.32) but decreased to the lowest AAMR by 2019 (30.77). Totally, 203,368 (81.31%) of all deaths related to HF and sepsis were in medical facilities, 18,430 (7.37%) were in home/hospice facilities, and 24,713 (9.88%) in nursing homes.
Conclusions: HF and sepsis-related mortality in the elderly population increased over the past two decades, with men and African Americans at disproportionately higher risk.
Keywords: Heart failure; Sepsis; Mortality trends
| Introduction | ▴Top |
Heart failure (HF) and sepsis are major causes of disease burden in the USA. Approximately 6.7 million Americans over the age of 20 suffer from HF, with HF-related mortality rising since 2012 [1]. The prevalence of patients with HF is also expected to increase to 8.5 million Americans by 2030 [1]. Along with this, 1.7 million Americans develop sepsis each year, with the Centers for Disease Control and Prevention (CDC) listing sepsis as the third most common cause of death in US hospitals [2-4]. Cardiac abnormalities found in both acute and chronic HF can lead to myocardial damage and fluid retention, placing patients with HF at high risk of developing other diseases and both cardiovascular and non-cardiovascular causes of death [5-9]. The host-mediated immune response in sepsis causes fluid to shift from a patient’s vasculature to interstitial space, causing overall organ dysfunction and potentially leading to septic shock and death [5, 6, 10]. Sepsis also causes significant cardiac depression independently of preexisting cardiac conditions via inhibitory effects of beta-adrenergic activity, resulting in decreased heart rate and contractility, as well as increased cytokine-mediated production of reactive oxygen species, which are directly cytotoxic to cardiomyocytes [6, 11-13]. Cardiovascular disease caused by sepsis is a leading cause of rehospitalization and death, indicating that patients with preexisting HF may experience even more deleterious effects from developing sepsis [6, 14-17].
According to a literature review conducted in 2019, sepsis is responsible for about one-fourth of deaths in patients with pre-existing HF [5]. The relationship between sepsis and HF complicates treatment because treating sepsis involves fluid resuscitation, which can be compromised due to concomitant HF [5, 18, 19]. Managing both conditions in the same patient is challenging and leads to worse outcomes [5, 6, 20]. Even though infections are considered one of the most common causes of hospitalization for HF patients, optimum medical management for HF patients admitted with sepsis is still an interplay of risk vs. benefit with no formal guidelines [6, 21]. Despite the well-known fact that infection and resulting sepsis increase the risk of mortality in patients with HF, national estimates of deaths related to both HF and sepsis are not well established [7, 22, 23]. The purpose of this study is to analyze contemporary trends in HF and sepsis-related mortality via a publicly available national database of recorded deaths in the USA. Researchers also aim to provide information regarding which demographic groups are most impacted by concurrent HF and sepsis so that targeted interventions can be implemented to improve their outcomes.
| Materials and Methods | ▴Top |
Study design and database
In this repeated cross-sectional study, the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database was analyzed from 1999 to 2019 in adults ≥ 65 years [24]. All deaths related to HF and septicemia as a contributing or underlying (primary) cause of death on nationwide death certificates were queried [24]. The International Classifications of Disease (ICD), 10th Revision were utilized to gather information on related cases (Supplementary Material 1, cr.elmerpub.com) [24]. This study queries the two conditions together to identify patients who had both HF and sepsis as contributing or underlying causes of death. Deaths related to HF alone and septicemia alone were also analyzed. Mortality data were then further analyzed based on gender, race, region and place (type of facility) of death. Gender comparison included males or females, while race specifically compared Black or African American patients to White patients. Regions examined were the Northeast, Midwest, South, and West regions of the USA as defined by Census Bureau classification, and each region was also stratified by race. Place of death included medical facility (inpatient medical facility, outpatient medical facility, or emergency room (ER)), decedent’s home/hospice facility, or nursing home/long-term care.
The Institutional Review Board (IRB) approval was not required for this study. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Statistical analysis
Age-adjusted mortality rates (AAMRs) were calculated for collected data. This measurement helps control for variation in age, allowing for data comparison [25]. The Joinpoint Regression Program (Joinpoint version 4.9.0.0) from the National Cancer Institute, Bethesda, Maryland, was utilized to analyze mortality during the study period [26]. This multiple joinpoint regression program utilized already calculated AAMRs to determine annual percentage changes (APCs) and average annual percent changes (AAPCs) in mortality trends across the study period [26, 27]. The model fits linear segments to the data where significant temporal variation occurred [26]. APCs with 95% confidence intervals (CIs) for AAMRs were calculated for the line segments connecting a joinpoint using the Monte Carlo permutation test [26]. The Monte Carlo permutation test for joinpoint analysis determines the number of joinpoints or points where a significant change in trend occurs in a regression model. The weighted averages of the APCs were then calculated and reported as the AAPC with corresponding 95% CIs, summarizing the reported mortality trend for the entire study period. APC and AAPCs representing mortality trends were analyzed utilizing a two-tailed t-test with statistical significance set at P ≤ 0.05. Significant results are represented by an asterisk “*” in the results and figures.
| Results | ▴Top |
Overall
Between 1999 and 2019, a total of 5,887,799 deaths related to HF, 2,584,523 deaths related to sepsis, and 250,115 reported deaths related to both occurred [24]. Of total reported deaths, 135,074 were female, 115,041 were male, 30,024 were Black or African American patients, 213,272 were White patients, and the remaining 6,819 reported deaths were of other racial origins (Table 1). Other racial origins included Hispanic or Latino, Asian or Pacific Islander, and American Indian or Alaska Native groups. These groups could not be analyzed due to data suppression by the CDC WONDER database.
 Click to view | Table 1. Annual HF + Sepsis Deaths, Stratified by Gender and Race, Along With HF and Sepsis Deaths From 1999 to 2019 |
Between 1999 and 2019, the AAMR for HF (AAPC -0.80%) and sepsis (AAPC -0.28%) both decreased, but the combined HF and sepsis-related AAMR increased (AAPC 1.06%) (Supplementary Material 2, cr.elmerpub.com). AAMR for HF-related deaths only decreased from 793.08 deaths per 100,000 people in 1999 to 598.65 deaths per 100,000 people in 2012 (APC: -2.27, 95% CI: -2.47 to -2.08) and then increased to 680.62 deaths per 100,000 people between 2012 and 2019 (APC: 2.00, 95% CI: 1.51 to 2.56) (Fig. 1, Supplementary Material 3, cr.elmerpub.com).
 Click for large image | Figure 1. Trends in age-adjusted mortality rate (AAMR) related to HF, sepsis, and both in the USA (1999 - 2019). HF: 1999 to 2012 APC: -2.27*, 2012 to 2019 APC: 1.99*. Sepsis 1999 to 2012 APC: -0.48*, 2012 to 2017 APC: 1.66*, 2017 to 2019 APC: -3.69*. *Statistically significant results. HF: heart failure; APC: annual percentage change. |
AAMR for sepsis-related deaths only decreased from 305.98 in 1999 to 282.85 in 2012 (APC: -0.48, 95% CI: -0.84 to -0.25), increased to 308.75 in 2017 (APC: 1.66, 95% CI: 0.90 to 3.37), and decreased again to 288.49 in 2019 (APC: -3.69, 95% CI: -5.66 to -1.35) (Fig. 1, Supplementary Material 3, cr.elmerpub.com). AMMR for combined HF and sepsis-related deaths increased from 28.85 in 1999 to 30.24 in 2005 (APC: 0.53, 95% CI: -0.92 to 5.15) (Fig. 1, Supplementary Material 4, cr.elmerpub.com). AAMR then decreased to 25.25 in 2012 (APC: -1.96, 95% CI: -6.27 to 3.64), and finally increased to 33.71 in 2019 (APC: 4.65*, 95% CI: 3.06 to 7.40) (Fig. 1, Supplementary Material 3, cr.elmerpub.com).
Gender stratified
Men had consistently higher AAMRs compared with women and a greater increase in mortality (AAPC in men 1.53% vs. women 0.56%) throughout the study period (Supplementary Material 5, cr.elmerpub.com). Men’s AAMR increased from 32.59 deaths per 100,000 people in 1999 to 34.13 in 2005 (APC: 0.90, 95% CI: -0.62 to 7.00), decreased to 30.19 in 2012 (APC: -1.48, 95% CI: -6.03 to 6.38), then increased drastically to 41.78 in 2019 (APC: 5.20*, 95% CI: 3.00 to 8.19) (Fig. 2, Supplementary Material 4, cr.elmerpub.com). In women, the AAMR increased from 26.59 deaths per 100,000 people in 1999 to 27.82 in 2005 (APC: 0.24, 95% CI: 1.09 to 4.04), decreased to 21.93 in 2012 (APC: -2.47, 95% CI: -6.19 to 0.42), and significantly increased to 27.99 in 2019 (APC: 3.96*, 95% CI: 2.67 to 5.90) (Fig. 2, Supplementary Material 4, cr.elmerpub.com).
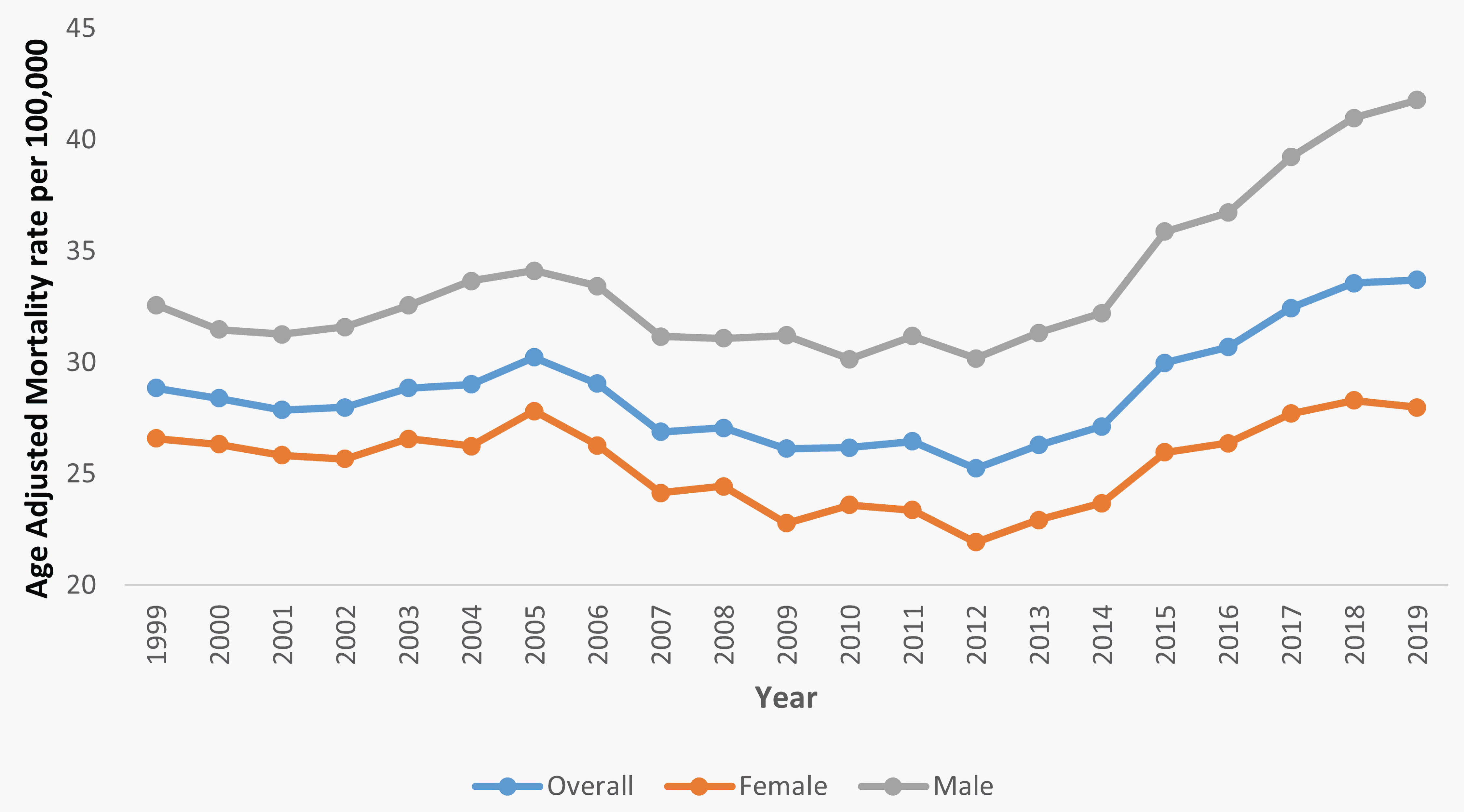 Click for large image | Figure 2. Trends in HF and sepsis-related age-adjusted mortality rates (AAMR) stratified by gender in the USA (1999 - 2019). Overall, 1999 to 2005 APC: 0.53, 2005 to 2012 APC: -1.96, 2012 to 2019 APC: 4.65*. Female 1999 to 2005 APC: 0.24, 2005 to 2012 APC: -2.47. Male 1999 to 2005 APC: 0.90, 2005 to 2012 APC: -1.48, 2012 to 2019 APC: 5.20*. *Statistically significant results. HF: heart failure; APC: annual percentage change. |
The overall AAMR for both genders increased from 28.85 deaths per 100,000 people in 1999 to 30.24 in 2005 (APC: 0.53, 95% CI: -0.92 to 5.15), decreased to 25.25 in 2012 (APC: -1.96, 95% CI: -6.27 to 3.64), and dramatically increased to 33.71 in 2019 (APC: 4.65*, 95% CI: 3.06 to 7.40) (Fig. 2, Supplementary Material 4, cr.elmerpub.com). Although the AAMR among male, female, and overall reported deaths declined between 2005 and 2012, all three AAMR values have increased significantly since 2012. This resulted in male, female, and overall average AAPC values of 1.5330* (95% CI: 1.15 to 2.13), 0.5564* (95% CI: 0.26 to 0.96), and 1.0613* (95% CI: 0.74 to 1.57), respectively (Supplementary Material 2, cr.elmerpub.com).
Race stratified
Although Black or African American patients saw a decrease in mortality overall (AAPC: -0.83*, 95% CI: -0.13 to -0.42), Black or African Americans had consistently higher AAMRs compared to White patients throughout the study period (Supplementary Material 6, cr.elmerpub.com). Although White patients had lower AAMR values when compared to Black or African American patients, they saw a significant increase in mortality over the study period (AAPC: 1.37*, 95% CI: 1.07 to 1.81) (Supplementary Material 6, cr.elmerpub.com).
Black and African American patients’ AAMR slightly decreased from 48.9 deaths per 100,000 in 1999 to 48.84 in 2005 (APC: -0.71, 95% CI: -1.95 to 2.55), decreased significantly to 36.32 in 2011 (APC: -4.58*, 95% CI: -8.61 to -3.11), and dramatically increased to 40.56 in 2019 (APC: 1.98*, 95% CI: 1.00 to 3.50) (Fig. 3, Supplementary Material 7, cr.elmerpub.com). White patients’ AAMR increased slightly from 27.26 deaths per 100,000 in 1999 to 28.9 in 2005 (APC: 0.75, 95% CI: -0.62 to 4.77), decreased to 24.52 in 2012 (APC: -1.68, 95% CI: -5.51 to 3.66), and finally significantly increased to 33.81 in 2019 (APC: 5.07*, 95% CI: 3.65 to 7.17) (Fig. 3, Supplementary Material 7, cr.elmerpub.com).
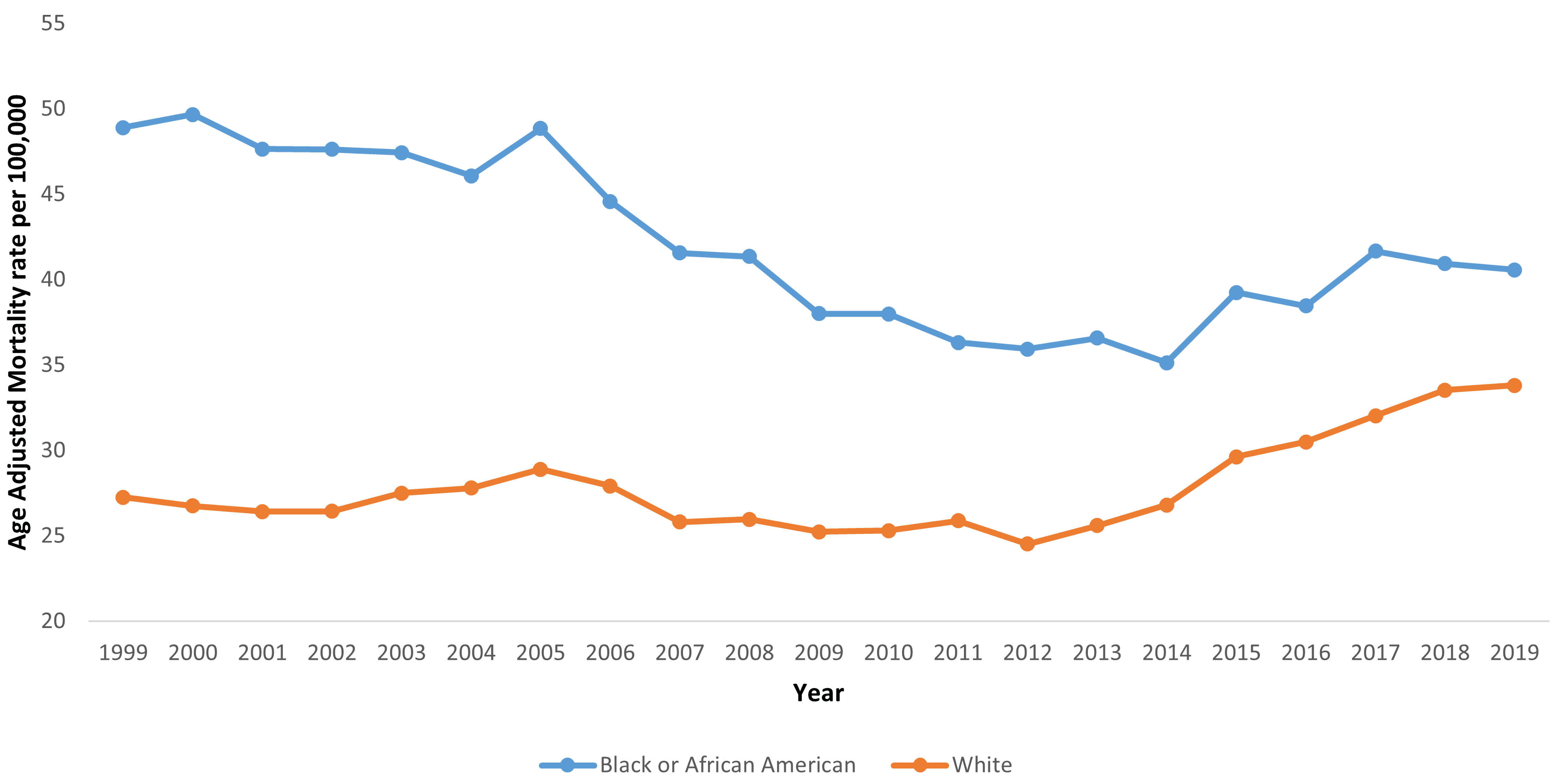 Click for large image | Figure 3. Trends in HF and sepsis-related age-adjusted mortality rates (AAMR) stratified by race in the USA (1999 - 2019). Black or African American 1999 to 2005 APC: -0.72, 2005 to 2011 APC: -4.58*, 2011 to 2019 APC: 1.98*. White 1999 to 2005 APC: 0.75, 2005 to 2012 APC: -1.68, 2012 to 2019 APC: 5.07*. *Statistically significant results. HF: heart failure; APC: annual percentage change. |
Region stratified
HF and sepsis-related deaths increased in all regions except the Northeast, with AAPCs of -0.11 (95% CI: -0.59 to 0.40), 1.02* (95% CI: 0.62 to 1.43), 0.96* (95% CI: 0.65 to 1.46), and 2.29* (95% CI: 1.86 to 2.95) for Northeast, Midwest, South, and West, respectively (Supplementary Material 8, cr.elmerpub.com).
The Northeast region AAMR slightly decreased from 32.32 deaths per 100,000 people in 1999 to 31.22 in 2006 (APC: -0.54, 95% CI: -2.02 to 4.00), decreased again to 25.38 in 2009 (APC: -5.03, 95% CI: -7.21 to 4.43), and finally increased to 30.77 in 2019 (APC: 1.72, 95% CI: -1.85 to 4.07) (Fig. 4, Supplementary Material 9, cr.elmerpub.com). The Northeast was the only region that did not see a significant increase in HF and sepsis-related mortality throughout the study period.
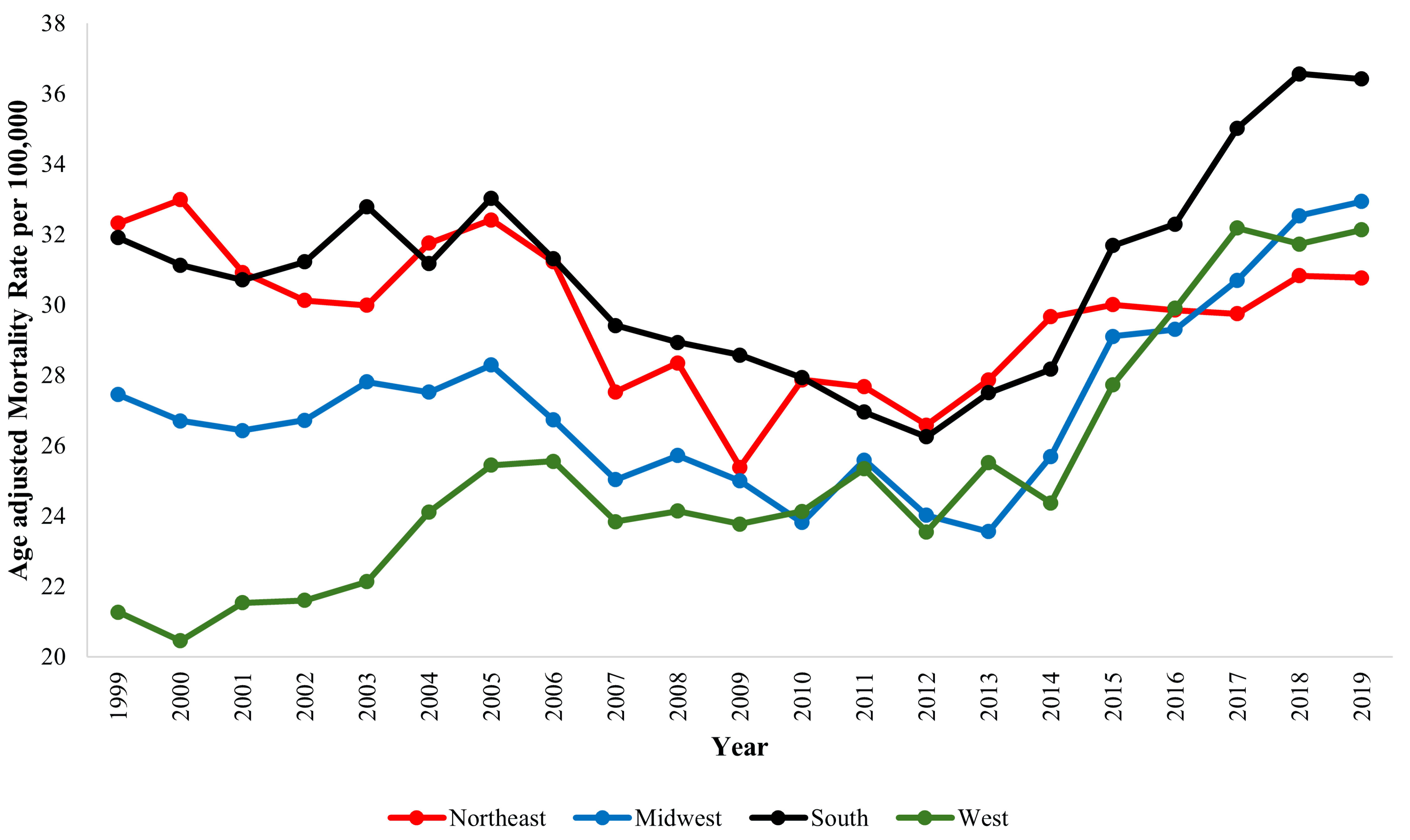 Click for large image | Figure 4. Trends in HF and sepsis-related age-adjusted mortality rates (AAMR) stratified by region in the USA (1999 - 2019). Northeast 1999 to 2006 APC: -0.54, 2006 to 2009 APC: -5.03, 2009 to 2019 APC: 1.72. Midwest 1999 to 2013 APC: -0.89*, 2013 to 2019 APC: 5.61*. South 1999 to 2005 APC: 0.42, 2005 to 2012 APC: -2.81*, 2012 to 2019 APC: 5.37*. West 1999 to 2005 APC: 3.16*, 2005 to 2014 APC: 0.11, 2014 to 2017 APC: 9.45, 2017 to 2019 APC: -0.72. *Statistically significant results. HF: heart failure; APC: annual percentage change. |
The Midwest region AAMR decreased from 27.45 deaths per 100,000 people in 1999 to 23.56 in 2013 (APC: -0.89*, 95% CI: -1.71 to -0.24) but then increased to 32.94 in 2019 (APC: 5.61*, 95% CI: 3.64 to 9.64) (Fig. 4, Supplementary Material 9, cr.elmerpub.com).
The South region AAMR increased slightly from 31.91 deaths per 100,00 people in 1999 to 33.03 in 2005 (APC: 0.42, 95% CI: -1.11 to 4.41), decreased significantly to 26.25 in 2012 (APC: -2.81*, 95% CI: -7.29 to -0.89), and dramatically increased to 36.42 in 2019 (APC: 5.37*, 95% CI: 4.03 to 7.39) (Fig. 4, Supplementary Material 9, cr.elmerpub.com).
The West region AAMR increased significantly from 21.27 deaths per 100,000 people in 1999 to 25.44 in 2005 (APC: 3.16*, 95% CI: 0.61 to 8.96), slightly decreased to 24.37 in 2014 (APC: 0.11, 95% CI: -4.74 to 5.08), increased to 32.18 in 2017 (APC: 9.45, 95% CI: -0.15 to 12.11), and slightly decreased to 32.13 in 2019 (APC: -0.72, 95% CI: -5.54 to 5.40) (Fig. 4, Supplementary Material 9, cr.elmerpub.com).
Region and race stratified
Data stratified based on the region of HF and sepsis-related death and race (Black or African American and White patients) were collected (Fig. 5).
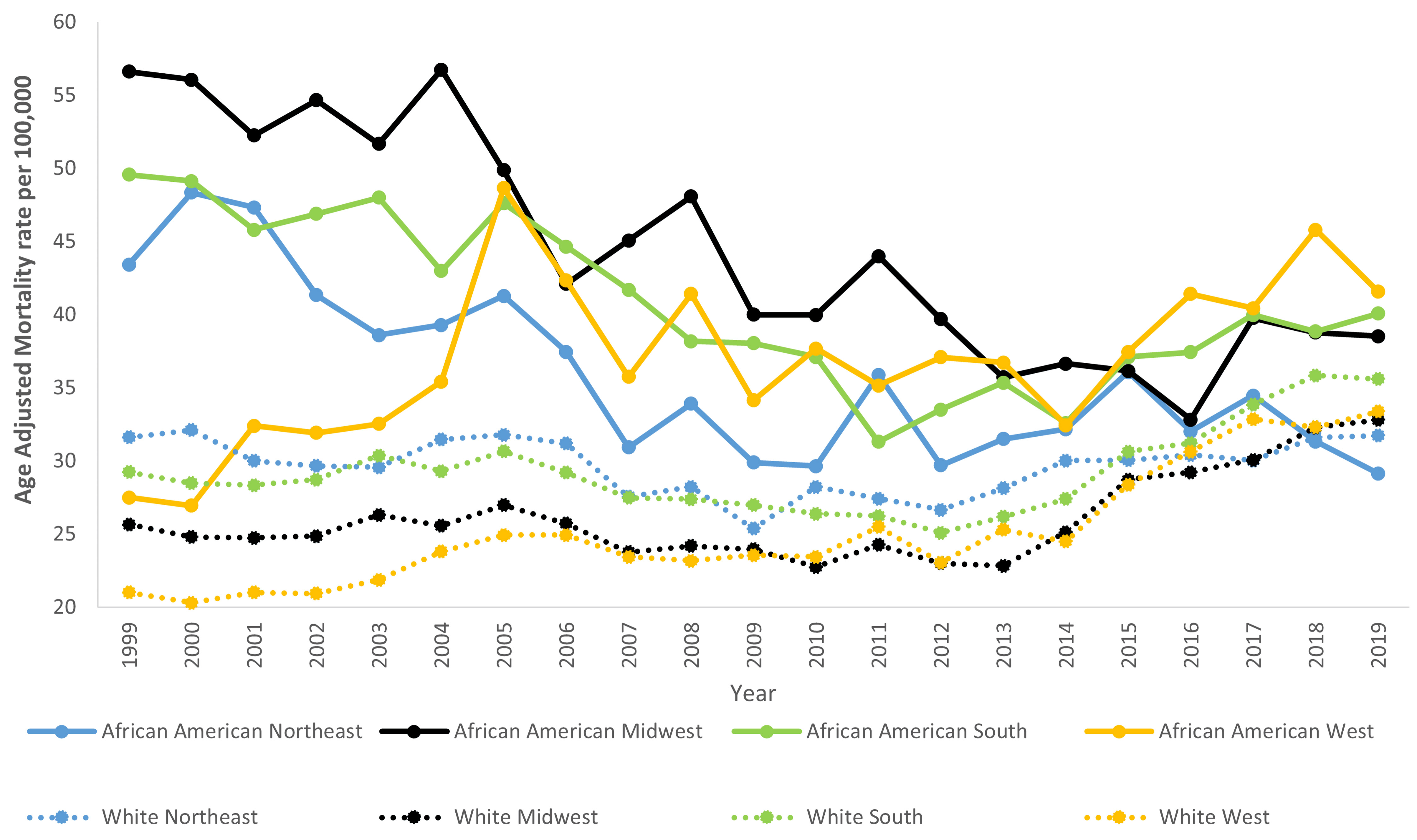 Click for large image | Figure 5. Trends in HF and sepsis-related age-adjusted mortality rates (AAMR) stratified by region and race in the USA (1999 - 2019). African American Northeast 1999 to 2009 APC: -3.94*, 2009 to 2019 APC: 0.05; African American Midwest 1999 to 2016 APC: -2.97*, 2016 to 2019 APC: 4.61; African American South 1999 to 2006 APC: -0.79, 2006 to 2011 APC: -6.02*, 2011 to 2019 APC: 3.18*; African American West 1999 to 2005 APC: 9.26*, 2005 to 2011 APC: -3.96*, 2011 to 2019 APC: 3.08*. White Northeast 1999 to 2006 APC: -0.22, 2006 to 2009 APC: -4.93, 2009 to 2019 APC: 1.98; White Midwest 1999 to 2012 APC: -0.85*, 2012 to 2019 APC: 5.30*; White South 1999 to 2005 APC: 0.70, 2005 to 2012 APC: -2.40*, 2012 to 2019 APC: 5.64*; White West 1999 to 2013 APC: 1.22, 2013 to 2019 APC: 5.47*. *Statistically significant results. HF: heart failure; APC: annual percentage change. |
Black or African American patients saw decreases in HF and sepsis-related mortality across every region (Northeast, Midwest, South, West) except in the West. The AAPCs for the Black or African American population in the Northeast, Midwest, South, and West regions were found to be -1.97* (95% CI: -2.91 to -0.95), -1.87* (95% CI: -2.76 to -1.26), -0.58 (95% CI: -0.96 to 0.002), and 2.69* (95% CI: 2.01 to 3.90), respectively (Supplementary Materials 10, 11, cr.elmerpub.com).
White patients saw increases in HF and sepsis-related mortality across every region (Northeast, Midwest, South, and West) except in the Northeast. The AAPCs for each region and White patients were found to be 0.14 (95% CI: -0.46 to 0.74), 1.26* (95% CI: 0.83 to 1.70), 1.29* (95% CI: 1.01 to 1.74), and 2.48* (95% CI: 1.86 to 3.06) for the Northeast, Midwest, South, and West regions, respectively (Supplementary Materials 12, 13, cr.elmerpub.com).
Place of death stratified
HF and sepsis-related mortality predominantly occurred in medical facilities (inpatient, outpatient, or ER), followed by nursing homes/long-term care and home/hospice facilities (Fig. 6a, b). Across the entirety of the study period, 203,368 (81.31%) of deaths took place in medical facilities, 24,713 (9.88%) took place in nursing homes/long-term care, and 18,430 (7.37%) took place in home/hospice facilities (Fig. 6c, d).
 Click for large image | Figure 6. (a, b) Trends in overall number of HF and sepsis-related deaths stratified by place of death in the USA (1999 - 2019). (c, d) Trends in the percentage of HF and sepsis-related deaths stratified by place of death in the USA (1999 - 2019). |
| Discussion | ▴Top |
Our study has many interesting findings: 1) Although AAMR contributing to HF-related and sepsis-related deaths both individually decreased, AAMR for combined HF and sepsis-related deaths increased throughout the study period; 2) HF and sepsis-related AAMR decreased in Black or African American patients and increased in White patients, though AAMR was still higher in Black or African Americans patients overall; 3) All regions saw an increase in AAMR, except for the Northeast USA, where AAMR remained stable. When stratifying both race and region, Black or African American patients saw a decline in AAMR in all regions except the West, where it remained stable. White patients experienced an increase in AAMR in all regions except the Northeast, where AAMR remained stable.
The increase in the AAMR in combined HF- and sepsis-related deaths despite decreases in both individual AAMRs for HF-related deaths and sepsis-related deaths is potentially due to improvements in both HF and sepsis treatments. This allows mortality of both conditions to improve independently, in contrast to the confounding impacts on mortality when the two disease states occur concurrently. One review study published in 2023 emphasizes this point, highlighting the fact that in addition to traditional HF therapies, novel therapies are being developed that extend life and prevent death of HF patients [28]. Of the novel therapies mentioned, gene-editing therapy, regenerative medicine approaches, and precision medicine all work to prevent the progression of HF overall. Sepsis treatment has also significantly improved throughout the past few years, with many working to standardize an approach to sepsis treatment and care [29]. Empirical antimicrobial administration, fluid resuscitation, and use of vasoactive agents are all current hallmarks of sepsis treatment that are being refined continuously.
Along with this, many studies highlight the deleterious effects that concurrent HF and sepsis have on patient treatment outcomes. One prospective cohort study originally published in 2018 in the UK evaluated the connection between these two conditions. They found that of the 737 deaths that occurred among HF patients, 173 (23.5%) were due to sepsis [30]. This study also reasoned that as HF treatment advances, reduced mortality due to HF causes an increased contribution of other non-cardiovascular modes of death, such as sepsis. This, coupled with the HF- and sepsis-related mortality trends found in this paper, highlights a need for further development of more efficacious treatment for patients who experience these conditions concurrently.
Despite decreasing AAMR throughout the study period, Black or African American patients were still found to have higher mortality due to HF and sepsis-related death when compared to White patients. A contributing factor for this is Black or African American patients’ increased risk for HF overall, with the highest risk of death and hospitalization due to HF when compared to patients of other races [31]. A study published in 2021 found that although Black or African American patients have a higher disease burden of HF, this is not always driven by the presence of increased traditional cardiovascular risk factors. While the study found that traditional risk factors such as obesity, diabetes mellitus, and physical inactivity were more common in Black or African American patients when compared to White patients, factors such as social determinants of health and structural racism also contribute to their increased incidence of HF and worse clinical outcomes overall.
When looking at sepsis, although treatment protocols have been standardized, significantly worse outcomes and mortality rates are associated with Black or African American patients when compared to White patients [32]. A review study conducted in 2018 found that not only systemic bias contributes to these disparities, but numerous patient, community, and hospital-based factors do as well. Disparities in both HF and sepsis clinical outcomes among African American patients when compared to White patients likely contribute to the higher combined HF and sepsis-related AAMR. Worse outcomes of not only HF and sepsis individually in Black or African American patients, but also higher combined HF- and sepsis-related AAMR, indicate a need for further study among this patient population to specialize treatment and improve their outcomes overall.
All regions except the Northeast saw an increase in HF and sepsis-related mortality, and the Northeast was the only region where Black or African American patients did not have higher mortality compared to White patients. These results are consistent with regional trends in cardiovascular health data found in recent decades, including a retrospective cross-sectional study conducted between 2011 and 2017 [33]. This study examined the prevalence of ideal cardiovascular health index (CVHI) across the Northeast, Midwest, South, and West regions of the USA. CVHI, as measured in this study, analyzed blood pressure, blood glucose, lipid levels, body mass index (BMI), smoking status, physical activity and diet. Results found that over the course of the study period, the prevalence of ideal CVHI improved in the Northeast region, along with decreases in self-reported hypertension and numerous other cardiovascular risk factors in the region as well. The study highlights that significant improvement in the Northeast could be due to the on average higher socioeconomic status of the region when compared to other areas such as the South, highlighting another avenue for potential study [33]. It is crucial to understand not only trends in CVHI improvement but also HF- and sepsis-related mortality trends to determine which regions require more assistance in improving their HF- and sepsis-related outcomes overall.
Limitations
Due to CDC WONDER data being collected from a public health database, this study may have some limitations. Variables such as social determinants of health could contribute to a patient’s death that were not reported on the website or death certificate. Furthermore, we were only able to analyze racial disparities for White and Black or African American patients. Patients of other ethnic groups (Hispanic or Latino, Asian or Pacific Islander, American Indian or Alaska Native, etc.) could not be analyzed because of suppressed data for many years in each subgroup. CDC suppresses the counts of fewer than 10 in CDC WONDER data to protect the confidentiality of patients, and death rates are marked as unreliable for a count less than 20 per the CDC WONDER data use agreement. We also only analyzed data up until 2019 to avoid any potential skewing in mortality trends caused by the coronavirus disease 2019 (COVID-19) pandemic, which began in 2020. Despite taking this precaution, COVID-19 may have impacted data earlier than 2020, including in the latter part of 2019, prior to the medical community’s awareness of the virus. This represents another potential limitation of the study.
Conclusions
In conclusion, there has been a considerable increase in HF and sepsis-related mortality rates in the elderly population of the USA between 1999 and 2019. The results of this study revealed several continued disparities associated with gender, race, and region. These disparities in mortality must be further addressed to minimize HF and sepsis-related deaths in all population groups equitably.
| Supplementary Material | ▴Top |
Suppl 1. A list of ICD-10 codes used in this study.
Suppl 2. Multiple joinpoint model individual HF and sepsis deaths. HF and sepsis stratified data regarding mortality rates related to HF and sepsis between 1999 and 2019.
Suppl 3. HF and sepsis-related mortality trends stratified by HF, sepsis, and HF + sepsis combined.
Suppl 4. HF and sepsis related mortality trends stratified by gender.
Suppl 5. Multiple joinpoint model HF and sepsis deaths by gender. Overall and gender-stratified data regarding mortality rates related to HF and sepsis between 1999 and 2019.
Suppl 6. Multiple joinpoint model HF and sepsis deaths by race. Race-stratified data regarding mortality rates related to HF and sepsis between 1999 and 2019.
Suppl 7. HF and sepsis related mortality trends stratified by race.
Suppl 8. Multiple joinpoint model HF and sepsis deaths by region. Region-stratified data regarding mortality rates related to HF and sepsis between 1999 and 2019.
Suppl 9. HF and sepsis-related mortality trends stratified by region.
Suppl 10. HF and sepsis-related mortality trends stratified by region and Black or African American race.
Suppl 11. Multiple joinpoint model HF and sepsis deaths by race and region. Black or African American patient and region-stratified data regarding mortality rates related to HF and sepsis between 1999 and 2019.
Suppl 12. HF and sepsis-related mortality trends stratified by region and White race.
Suppl 13. Multiple joinpoint model HF and sepsis deaths by race and region. White patients and region-stratified data regarding mortality rates related to HF and sepsis between 1999 and 2019.
Acknowledgments
The authors would like to thank the Creighton University School of Medicine Department of Internal Medicine, and Internal Medicine Research Interest Group for providing guidance and support during the writing of this manuscript.
Financial Disclosure
There is no financial disclosure for any of the authors listed in this publication. Grant funding for submission requirements was provided by the Creighton University School of Medicine Department of Internal Medicine.
Conflict of Interest
There is no conflict of interest for any of the authors listed on this publication.
Informed Consent
No informed consent was required to perform this database-related study.
Author Contributions
Olivia Foley contributed to the writing and revision of the manuscript. Ali Bin Abdul Jabbar contributed to the conceptualization, design, and revision of the manuscript. Kimberly K. Levine contributed to the editing and formatting of the manuscript. Ahmed El-Shaer contributed to the final revision and approval of the manuscript. Abubakar Tauseef contributed to the final revision and approval of the manuscript. Ahmed Aboeata contributed to the final revision and approval of the manuscript. All authors read and approved the final manuscript.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
HF: heart failure; CDC: Centers for Disease Control and Prevention; CDC WONDER: Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research; AAMR: age-adjusted mortality rate; AAPC: average annual percent change; ICD: International Classification of Disease; ER: emergency room; APC: annual percentage change; CIs: confidence intervals; CICU: cardiac intensive care unit; PROGRESS: Promoting Global Research Excellence in Severe Sepsis; CVHI: cardiovascular health index; BMI: body mass index; COVID-19: coronavirus disease 2019
| References | ▴Top |
- Bozkurt B, Ahmad T, Alexander KM, Baker WL, Bosak K, Breathett K, Fonarow GC, et al. Heart failure epidemiology and outcomes statistics: a report of the heart failure society of America. J Card Fail. 2023;29(10):1412-1451.
doi pubmed - Bridget Balch. Association of American Medical Colleges. Sepsis is the third leading cause of death in U.S. hospitals. But quick action can save lives. 2023 [cited Sep 10, 2024]. p. 1. Available from: https://www.aamc.org/news/sepsis-third-leading-cause-death-us-hospitals-quick-action-can-save-lives.
- National Institute of General Medical Sciences [Internet]. Sepsis. 2024 [cited Sep 11, 2024]. Available from: https://www.nigms.nih.gov/education/fact-sheets/Pages/sepsis.aspx.
- ScienceDaily. Sepsis increased risk of heart failure and rehospitalization after hospital discharge. J Am Heart Assoc. Feb 1, 2023.
- Arfaras-Melainis A, Polyzogopoulou E, Triposkiadis F, Xanthopoulos A, Ikonomidis I, Mebazaa A, Parissis J. Heart failure and sepsis: practical recommendations for the optimal management. Heart Fail Rev. 2020;25(2):183-194.
doi pubmed - Jones TW, Smith SE, Van Tuyl JS, Newsome AS. Sepsis with preexisting heart failure: management of confounding clinical features. J Intensive Care Med. 2021;36(9):989-1012.
doi pubmed - Logeart D, Isnard R, Resche-Rigon M, Seronde MF, de Groote P, Jondeau G, Galinier M, et al. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: the OFICA study. Eur J Heart Fail. 2013;15(4):465-476.
doi pubmed - Henkel DM, Redfield MM, Weston SA, Gerber Y, Roger VL. Death in heart failure: a community perspective. Circ Heart Fail. 2008;1(2):91-97.
doi pubmed - Bozkurt B, Coats AJ, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, Anker SD, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail. 2021;27(4):387-413.
doi pubmed - Zhu MY, Tang XK, Gao Y, Xu JJ, Gong YQ. Impact of heart failure on outcomes in patients with sepsis: A systematic review and meta-analysis. World J Clin Cases. 2023;11(15):3511-3521.
doi pubmed - Hunter JD, Doddi M. Sepsis and the heart. Br J Anaesth. 2010;104(1):3-11.
doi pubmed - Evans T. CMJv18n2-CMEEvans.indd [Internet]. Vol. 17, CME INFECTIOUS DISEASES Clinical Medicine. 2017. Available from: www.nice.org.uk/guidance/ng51.
- Zhang Y, McCurdy MT, Ludmir J. Sepsis management in the cardiac intensive care unit. J Cardiovasc Dev Dis. 2023;10(10):429.
doi pubmed - Patel N, Bajaj NS, Doshi R, Gupta A, Kalra R, Singh A, Berra L, et al. Cardiovascular events and hospital deaths among patients with severe sepsis. Am J Cardiol. 2019;123(9):1406-1413.
doi pubmed - Inoue S, Suzuki-Utsunomiya K, Komori Y, Kamijo A, Yumura I, Tanabe K, Miyawaki A, et al. Fermentation of non-sterilized fish biomass with a mixed culture of film-forming yeasts and lactobacilli and its effect on innate and adaptive immunity in mice. J Biosci Bioeng. 2013;116(6):682-687.
doi pubmed - Mankowski RT, Yende S, Angus DC. Long-term impact of sepsis on cardiovascular health. Intensive Care Med. 2019;45(1):78-81.
doi pubmed - Powell RE, Kennedy JN, Senussi MH, Barbash IJ, Seymour CW. Association between preexisting heart failure with reduced ejection fraction and fluid administration among patients with sepsis. JAMA Netw Open. 2022;5(10):e2235331.
doi pubmed - National Heart Lung, Blood Institute Prevention, Early Treatment of Acute Lung Injury Clinical Trials Network. Shapiro NI, Douglas IS, Brower RG, Brown SM, et al. Early Restrictive or liberal fluid management for sepsis-induced hypotension. N Engl J Med. 2023;388(6):499-510.
doi pubmed - Cuthbert JJ, Clark AL. Diuretic Treatment in patients with heart failure: current evidence and future directions - part I: loop diuretics. Curr Heart Fail Rep. 2024;21(2):101-114.
doi pubmed - Dong N, Gao N, Hu W, Mu Y, Pang L. Association of fluid management with mortality of sepsis patients with congestive heart failure: a retrospective cohort study. Front Med (Lausanne). 2022;9:714384.
doi pubmed - Alon D, Stein GY, Korenfeld R, Fuchs S. Predictors and outcomes of infection-related hospital admissions of heart failure patients. PLoS One. 2013;8(8):e72476.
doi pubmed - Vaduganathan M, Patel RB, Michel A, Shah SJ, Senni M, Gheorghiade M, Butler J. Mode of death in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2017;69(5):556-569.
doi pubmed - Hamaguchi S, Kinugawa S, Sobirin MA, Goto D, Tsuchihashi-Makaya M, Yamada S, Yokoshiki H, et al. Mode of death in patients with heart failure and reduced vs. preserved ejection fraction: report from the registry of hospitalized heart failure patients. Circ J. 2012;76(7):1662-1669.
doi pubmed - Centers for Disease Control and Prevention, National Center for Health Statistics. [Internet]. National Center for Health Statistics Mortality Data on CDC WONDER, Multiple Cause of Death Files, 1999-2020. 2021 [cited Jul 18, 2024]. Available from: http://wonder.cdc.gov/mcd-icd10.html.
- Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47(3).
pubmed - Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351.
doi pubmed - Gillis D, Edwards BPM. The utility of joinpoint regression for estimating population parameters given changes in population structure. Heliyon. 2019;5(11):e02515.
doi pubmed - Sapna F, Raveena F, Chandio M, Bai K, Sayyar M, Varrassi G, et al. Advancements in heart failure management: a comprehensive narrative review of emerging therapies. Cureus. 2023.
- Guarino M, Perna B, Cesaro AE, Maritati M, Spampinato MD, Contini C, De Giorgio R. 2023 update on sepsis and septic shock in adult patients: management in the emergency department. J Clin Med. 2023;12(9):3188.
doi pubmed - Walker AMN, Drozd M, Hall M, Patel PA, Paton M, Lowry J, Gierula J, et al. Prevalence and predictors of sepsis death in patients with chronic heart failure and reduced left ventricular ejection fraction. J Am Heart Assoc. 2018;7(20):e009684.
doi pubmed - Pina IL, Jimenez S, Lewis EF, Morris AA, Onwuanyi A, Tam E, Ventura HO. Race and ethnicity in heart failure: JACC focus seminar 8/9. J Am Coll Cardiol. 2021;78(25):2589-2598.
doi pubmed - DiMeglio M, Dubensky J, Schadt S, Potdar R, Laudanski K. Factors underlying racial disparities in sepsis management. Healthcare (Basel). 2018;6(4).
doi pubmed - Parcha V, Kalra R, Suri SS, Malla G, Wang TJ, Arora G, Arora P. Geographic variation in cardiovascular health among American adults. Mayo Clin Proc. 2021;96(7):1770-1781.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiology Research is published by Elmer Press Inc.