Complex Interactions of Social Determinants of Health on Survival Outcomes in Hispanic Patients With Pulmonary Arterial Hypertension in a US-Mexican Border City
DOI:
https://doi.org/10.14740/cr1748Keywords:
Pulmonary arterial hypertension, Social determinants of health, Health insurance, Employment status, Social support, Hispanic population, Health disparityAbstract
Background: Pulmonary arterial hypertension (PAH) is a chronic disease of the pulmonary blood vessels that can lead to right heart failure, resulting in increased morbidity and mortality if left untreated. While right heart hemodynamics and functional capacity are a well-established predictors of outcome in PAH, emerging evidence suggests that social determinants of health (SDOH) may have a significant impact on patients with PAH, influencing outcomes and survival rates. This study explores the impact of SDOH and their intricate interactions on survival among a Hispanic patient cohort along the US-Mexico border.
Methods: A retrospective analysis was conducted on a single-center cohort of 158 PAH patients (72% female, mean age 58 years) using Cox proportional hazards models and latent class analyses. The primary outcome was mortality during the follow-up period, with secondary analyses examining the impact of individual and combined SDOH on survival.
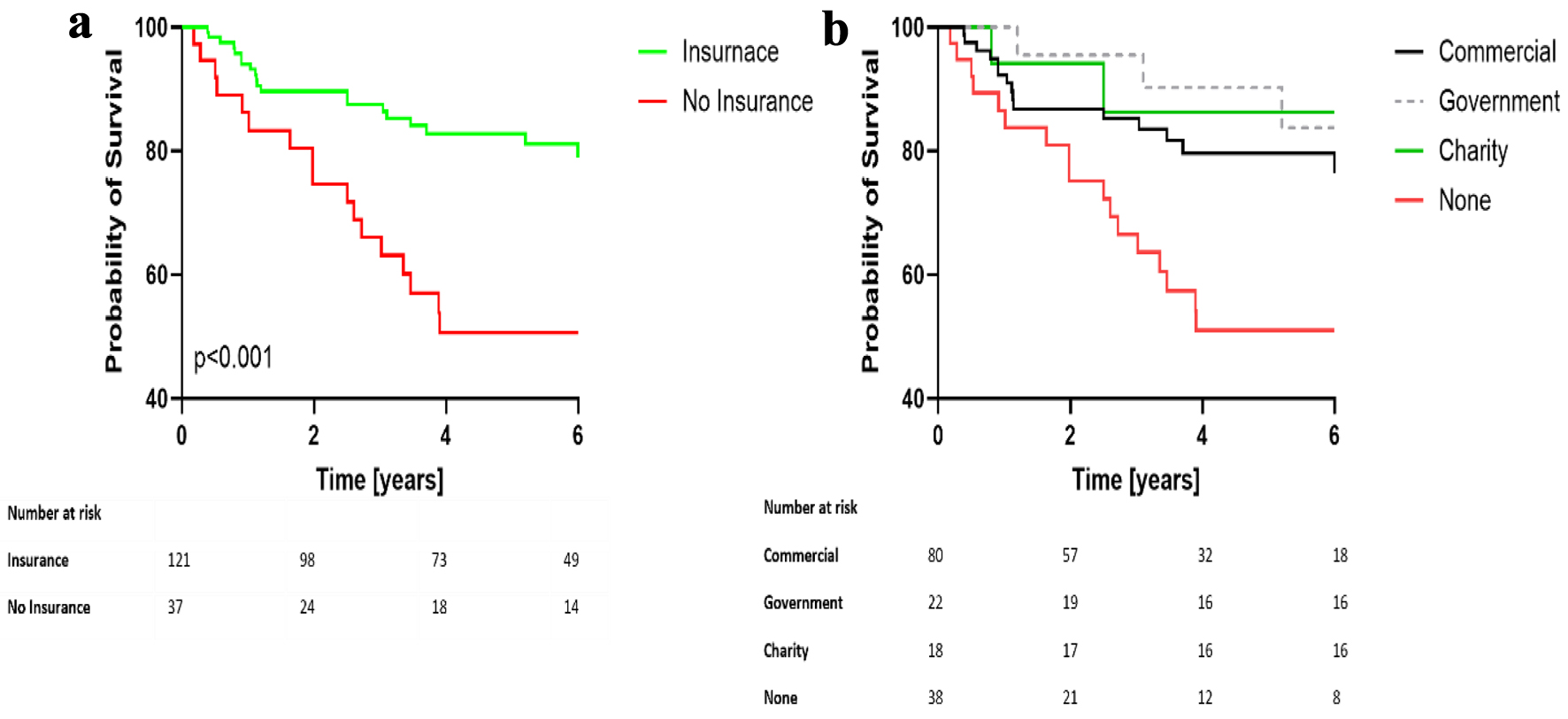
Results: During a mean follow-up period of 3.8 years (range: 0.2 to 6 years), 37 patients (23.4%) died. Lack of health insurance (hazard ratio (HR) 2.17; 95% confidence interval (CI): 1.05 - 4.49, P = 0.037) and unemployment (HR 2.99; 95% CI: 1.42 - 6.30, P = 0.004) were significantly associated with a higher risk of death within 5 years of follow-up. Latent variable modeling revealed that patients aged ≥ 60 years, who were uninsured, unmarried, and unemployed along with greater PAH severity (measured with cardiac output, mean pulmonary arterial pressure, six-minute walk distance, and World Health Organization Functional Class > 2) had the highest risk of poor outcomes (HR 3.6, 95% CI: 1.9 - 6.8, P < 0.001). Interestingly, the type of insurance did not have a significant impact on survival.
Conclusion: The findings underscore the critical need for improved access to insurance coverage and enhanced social support to promote better health outcomes among this vulnerable Hispanic population. Addressing these SDOH is essential in closing the health disparity gap and improving survival rates in PAH patients.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.









